PSYCHIATRY AND NARCOLOGY. «CONTROVERSIAL ISSUES OF GENDER IDENTITY»
Objective — to study and analyze the current trends among Western scientists and mental health professionals regarding issues of gender identity; to study the data of foreign and domestic studies concerning the problems of gender incongruence, gender dysphoria and their comorbidity with mental disorders, personality disorders, especially with schizophrenia and autism spectrum disorders; to identify promising areas of scientific research in this direction. Source search in electronic databases was carried out mainly for the past 5 years among foreign and russian publications, including Web of science, Researchgate.net, Google Scholar, Elibrary, Cyberleninka systems, using phrases such as gender identity disorder, gender identity disorder comorbidity, gender identity disorder schizophrenia, gender identity disorder autism, gender nonconformity, mentalization personality disorder. The article presents the data of modern publications and studies, showing, on the one hand, the tendency of Western experts to depathologize gender incongruence, promote gender transition, on the other hand, an active study of the relationship between this phenomenon with autism and schizophrenia spectrum disorders, personality disorders. According to the presented studies, the influence of mentalization features on the presence of mental disorders and gender incongruence is revealed.
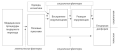
Today, psychiatric care for people with transgender people in the Russian Federation is difficult due to non-compliance with ethical principles in the work of the psychiatric service. The article deals with the unresolved ethical conflict regarding gender reassignment procedures between proponents of "not allowed, forbidden" with the attitude of psychiatrists to issue permission for sex reassignment only to "real" transsexuals, and supporters of the opposite liberal attitude towards issuing permission. for gender reassignment procedures for almost all applicants. Our article discusses ethical issues to help transgender people. The ethical principles of autonomy, harmlessness and beneficence in this article are intended to help transgender people. The authors ethically write about adding and not adding a transgender diagnosis to the International Classification of Diseases. This article raises concerns about the benefits and harms, the principle of respect for autonomy and the principle of beneficence, in order to provide good quality ethical care for transgender people. The authors discuss the problem of the ethical attitude of a psychiatrist to the mental health of transgender subjects. The authors discuss the ethical problem of the psychiatrist's attitude to the mental health of transgender subjects, medicalization and medical paternalism with the help of transgender people. This article raises considerations about the ethical role of the psychiatrist in gender reassignment procedures for subjects with varying degrees of mental health. The authors propose an algorithm for providing psychiatric care to persons who have undergone gender reassignment, which includes an in-depth examination by psychiatrists, psychologists, sexologists and a collegial conclusion on the state of mental health of a transgender person in the triad: mentally healthy or "have mental disorders", "borderline" or "mental psychotic disorders".
Recently, the issues of violations of gender identity are becoming more relevant and discussed, the number of patients with a request for a sex change is increasing. The complexity of this issue requires clinicians to be competent in helping transgender people, as they sometimes face many obstacles in the way of receiving care in medical institutions: the lack of specialists in the regions, a clear algorithm for helping transgender people, discrimination, stigmatization, and financial difficulties. At the same time, there are more and more foreign studies devoted to "detransition", i.e. "reverse" gender reassignment, which may indicate existing problems in the diagnosis of these conditions and methods of providing medical care to patients with gender identity disorders. The most difficult issues when working with patients experiencing gender dysphoria, in addition to identifying the true causes of gender identity disorders, are the preservation of fertility after gender-affirmative interventions, possible regrets after operations, and the provision of medical care to minors. Changes in the classification of gender disorders, including the exclusion of transsexualism from the class of mental disorders, creates the basis for discussions about the clinical, psychopathological and phenomenological features of these conditions. The scientific review provides information on the clinical and psychological aspects of gender identity disorders, as well as on therapeutic interventions for individuals with this pathology, using a multidisciplinary approach. Certain stages of the provision of medical and social assistance are described to reduce risks and more successful, professional assistance to persons with a gender incongruence.
Objective: a psychopathological analysis of the ideas of sex change and a description of the state of the sexual sphere in patients with schizotypal disorder. Materials and methods: we examined 38 patients who applied with a request to change their passport sex and were diagnosed with schizotypal disorder, 27 of them were women, 9 were men. Methods: clinical-psychopathological, sexological. To assess the sexual sphere and identify the motivation for changing sex and plans for the future a specially designed questionnaire was used. Results: variants of the ideas of gender reassignment were identified: obsessive, fixed, dominant, overvalued, delusional, their features specific to schizotypal disorder were described. For each variant, varying degrees of severity of violations of criticality and features of sexual behavior are described. An analysis of the characteristics of the sexual sphere of the studied groups showed the predominance of delays in psychosexual development and the associated deactualization of this sphere. In order to characterize the ability to adequately assess one's state, it is necessary to assess criticality as a variant of capacity, the issue of its methodology needs to be developed. Conclusions: the selected options differ in the degree of violation of criticality, which should be taken into account when deciding whether to change the passport gender.
Purpose: to study the formed images of sexual self-consciousness in persons who applied for permission to change their sex. Materials and methods: 80 people were examined, 40 of whom applied for permission to change their sex (20 people male and 20 people of the female biological sex). The comparison group — 20 men and 20 women, whose gender identity coincides with the biological sex. Methods — Sandra Bem's BSRI (Bem Sex-Role Inventory) test, V.V. Stolin's self-attitude questionnaire, O.L. Kustovoi's questionnaire. Results: it has been established that in the group of transsexuals with a female biological sex, images of a man and a woman are clearly distinguished, the self-image is closer to the desired image of a man, while the image of a woman is less achievable. The group of male transsexuals is closer to the image of the “Ideal Man” than to the image of the “Ideal Woman”. The key features that correspond to their self-determination as women are revealed: passivity, dependence on others, compromise, gullibility. According to the self-perception of all 4 groups, the “Ideal Woman” is happier than the “Ideal Man”. In the transsexuals’ group of male biological sex, were found no differences with the indicators of conditionally healthy groups of both sexes in the parameter “Love for children”, in contrast to the group of female transsexuals of the biological sex. Male transsexuals are looking for a radically new way to meet their needs without judgment from society. Summary: the indicators of self-relationship in the comparison groups are higher than in the groups of persons striving for a sex change.
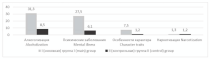
Objective: to identify potentially reversible clinical and socio-demographic factors influencing the social adaptation of patients with gender incongruence (GI). Materials and methods: a retrospective analysis of 926 patient records with MtF and FtM GI was performed. Results: among the patients who applied, 44.38% were MtF, 55.62% were FtM. The mean age was 24.0 years (from 13 to 65 years). The educational level of patients is mainly represented by higher (44.2%) and specialized (22.3%) education, 43% of persons lived in the village, 57% - in urban areas. The majority of those who applied grew up in a complete family (82.02%). The first manifestations of GI started mainly in the prepubertal (26.4%) and parapubertal (61.6%) period (up to 13 years). The average age of accepting oneself as a transgender person was 17.0 years. Steps to reduce dysphoria and receive specialized care are usually taken after the age of 20. 83.1% of transgender patients had depressive episodes, and a third (38.5%) had autoaggression. Additional psychiatric diagnoses were present in 24.5% of patients and are represented by 3 groups of diseases: group 1 (6.2%) — potentially reversible neurotic disorders; group 2 (14.1%) — background mental illnesses that are not the cause of GI; group 3 (4.3%) — other mental states with “ideas of sex change”. Conclusions: improvement of social adaptation and prevention of emotional and psychological experiences in persons with GI, assistance is possible at several levels: family, educational institutions, medical community, patient organizations.
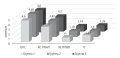
Objective: to study the influence of etiological factors on the possibility of the formation of organic personality disorder. Materials and methods: 80 patients with organic personality disorder were examined. The control group was represented by 82 healthy volunteers. Research methods: anamnestic, clinical, and statistical. Results: it was established that heredity aggravated by mental illness, alcoholization and drug addiction of relatives of different kinship lines, perinatal pathology factors associated with the child, diseases suffered in childhood (infectious diseases, etc.), which resulted in severe outcomes in the early stages of treatment in the form of hospitalizations or other complications in the form of pneumonia, bronchitis, etc., convulsive conditions, traumatic brain injuries received in childhood, reveal a reliably significant probability for the occurrence of organic personality disorder. The effect factor of operative interventions performed under general anesthesia in childhood did not show a statistically significant effect. Conclusions: heredity, perinatal pathology, some diseases suffered in childhood, convulsive states and various types of traumatic brain injury significantly increase the likelihood of organic personality disorder.
The article presents the current state of the problem of patients with gender dysphoria. The heterogeneity of clinical groups within which this phenomenon occurs is shown. It is indicated that a thorough clinical and paraclinical examination is necessary for the correct choice of further therapeutic and diagnostic tactics. As an example, a clinical case of a 14-year-old patient who applied to a medical center due to dissatisfaction with her sexual identity, as well as problems of increasing social maladaptation, in the form of self-harm and suicidal behavior is given. During the examination, the patient was diagnosed with schizotypal disorder in which optional symptoms developed in the form of gender dysphoria due to the presence of symptoms of dysmorphic mania in combination with affective manifestations. Correctly chosen therapeutic tactics led to stabilization of the patient's condition and complete relief of symptoms of gender dysphoria.
The change in the position of transsexualism in the new ICD classification, the hot debate about the psychopathological structure of this phenomenon and its relation to other mental disorders determine the relevance of considering the following clinical case.
A detailed clinical description demonstrates the possibility of combining two initially independent disorders - transsexualism and schizophrenia - which gave a bright individual color to the clinical picture and caused difficulties both in the medical and legal aspects of patient care.
At the age of 25, a patient with clinical signs of transsexualism developed acute paraphrenia psychosis. Without medical assistance, according to the mechanisms of sanogenesis, the severity of the condition decreased, but the psychotic state was not recovered. Features of the onset and dynamics of psychosis typical for the continuous type of paranoid schizophrenia (acuteness of development and absence of signs of syndromotaxis) allow us to attribute it to episodic with progressive or stable deficit paranoid schizophrenia variant. It is noteworthy that after the onset of psychosis, the stereotype of the development of birth-assigned gender rejection syndrome did not undergo significant changes: the formation of crossdressing, inverse psychosexual identity and inverse gender identity were finally completed; mimicry reactions became bright, self-destructive tendencies began to appear more and more clearly, and the patient applied for permission to change gender.
In the described clinical situation, the primary task is to overcome the acute schizophrenia psychosis. After solving this problem, the secondary prevention and rehabilitation program development becomes more important. Formally, the patient does not have the right to change sex, since she suffers from schizophrenia, which is a contraindication for sex transformation. In the state of psychosis, the patient essentially loses her civil procedural capacity. Informally, the question remains relevant.
EPIDEMIOLOGY
Gender transition medical procedures are effective in alleviating gender disphoria. However, their mechanisms of action are not yet fully understood. Hormone-replacement therapy (HRT) and surgeries modify sex characteristics. According to the biomedical model, perception of one's own sex characteristics is the primary contributor to gender dysphoria. Perception of the person in the wrong gender by others and/or their negative reaction is another (and less explored) mechanism leading to gender dysphoria. In order to conduct high-quality epidemiological studies, it is vital to take into consideration and measure intermediate outcomes, such as the degree of feminization/masculinization and the person's perceived gender. Sex characteristics are measurable, so it is possible to develop a feminization/masculinization scale. However, the task is complicated by the fact that various sex characteristics contribute unequally to the person's perceived gender, for which reason they should enter the scale with different coefficients. While such coefficients might be derived from controlled experiments, gender attibution in the real world depends on innumerable social factors. Reaction by others on the person's perceived gender is an additional factor affecting social gender dysphoria. Determining biological factors affecting the effectiveness of HRT in feminization and masculinization is a separate problem.
ENDOCRYNOLOGY
Glucocorticoids (GC) are one of the most common drugs in the practice of doctors of various specialties because of their therapeutic effects. The increased number of usage is related to the current SARS-CoV-2 virus pandemic. However, GC therapy has serious obstacles caused by side effects, including those leading to fatal outcomes. Side effects include: glucose and lipid metabolism impairments, weight gain, sleep disorders, thromboembolism, atherosclerosis, osteoporosis, myopathy, etc. The described processes cause a direct increase in the risk of developing cardiovascular diseases (CVD) even with short-term therapy and low doses of GC, which affects the further life, prognosis and outcomes of the underlying disease. This review describes in detail the pathogenetic mechanisms and the mutual influence of the side effects of GC, their contribution to the subsequent occurrence of CVD and focuses on the danger of irrational use of GC therapy.
Objective: to study the steroid metabolomics in women with normal body weight and various PCOS phenotypes by gas chromatography-mass spectrometry (GC-MS). Materials and methods: forty-eight(48)women with PCOS aged 25±0,3 yearswith a BMI less than 25 kg/m2 were examined. The control group (CG) consisted of twenty-five (25) healthy women aged 26±0,6 years with a BMI of 23 (21-24) kg/m2. Immunoassays were used to determine the levels of hormones in serum. Urinary steroid profiles (USP) were studied by GC-MS method. Statistical data processing was performed using the software system STATISTICA for WINDOWS (ver. 10). Results: the article provides an analysis of the metabolism of androgens, glucocorticoids and progestogens in women with different phenotypes of polycystic ovary syndromeaccording to gas chromatography-mass spectrometry. Summary: the urinary excretion of androstenedione metabolites was increased in PCOS patients with androgen excess and anovulation (A and B phenotypes), dehydroepiandrosterone metabolites - in PCOS patients with androgen excess (A, B and C phenotypes). PCOS women with phenotype C showed raised urinary excretion of 11-oxo-pregnanetriol, pregnanetriol and 17-hydroxypregnanolone, a decrease in the ratios of the sum of tetrahydro derivatives of cortisol and cortisone to these progestogens, as well as determination of tetrahydro-21-deoxycorticol and nonclassical 5-ene-pregnenes according to GC-MS data. In fact, it indicated to deficiency of the 21-hydroxylase enzyme in these patients. It was found PCOS patients with androgen excess (A, B and C phenotypes) had the signs of insufficient 3β-hydroxysteroid dehydrogenase activity. PCOS women with phenotype A were revealed deficiency of 11β-hydroxysteroid dehydrogenase (type 1).
CARDIOLOGY
Objective: to study predictors of acute kidney injury (AKI) in patients with ST-segment elevation myocardial infarction (STEMI) complicated by cardiogenic shock (CS) who underwent percutaneous coronary intervention. Materials and methods: 109 patients with STEMI complicated by CS were studied after interventional intervention (mean age 63.1±10.1 years). The observation group included 33 patients with AKI, and the comparison group — 76 patients without AKI. AKI was diagnosed with an increase in plasma creatinine level by ≥26.5 mmol/l from the baseline level within 48 hours or by ≥1.5 times from its known or assumed basal level. To identify predictors of AKI, the method of simple and multiple logistic regression was used. Results: among patients with AKI, patients aged over 70 years (54.5% vs 15.8%, p<0.001), with concomitant chronic kidney disease (57.6% vs 26.3%, p=0.002), chronic heart failure with a low ejection fraction (69.7% vs 36.8%, p=0.001), an initial glomerular filtration rate of less than 60 ml/min/1.73 m2 (54.5% vs 22.4%, p=0.001) and a left ventricular ejection fraction below 40% (75.8% vs 51.3%, p=0.022) and a three-vascular lesion of the coronary arteries (63.6% vs 40.8%, p=0.028) were significantly more often observed. Conclusions: AKI in patients with STEMI complicated by CS after intracoronary intervention was associated with an age older than 70 years, the presence of a left ventricular ejection fraction of less than 40% and a glomerular filtration rate of less than 60 ml/min/1.73 m2.
Objective: estimation of parameters of vascular stiffness in patients with arterial hypertension (AH) and atherosclerosis of the arteries of the lower extremities (AALE) taking into account statin therapy. Materials and methods: 120 patients with AH were divided into 3 groups: group 1 — 46 patients with AH and clinically manifested AALE, group 2 — 39 patients with AH and asymptomatic AALE, group 3 — 35 patients with AH without AALE. The patients of each group were divided into 2 subgroups: the 1st subgroup — not receiving statins, the 2nd subgroup — taking statins. All patients underwent laboratory and instrumental studies, including the determination of vascular stiffness parameters using the Vasotens software («Peter Telegin», Nizhny Novgorod) and ultrasonic triplex scanning of the arteries of the lower extremities. Statistical data processing was carried out using Microsoft Office Excel 16 (2015, Microsoft, USA), Statistica 10.0 (StatSoft, USA), IBM SPSS Statistica 26.0 (IBM, USA). Results: lower values of total cholesterol were found in patients of the 2nd subgroup of all studied groups (p<0,05), as well as lower values of low-density lipoprotein cholesterol (LDLС) among patients of the 2nd subgroup of the second and third groups (<0,05). In patients of all groups, when using statins, the target values of LDLC were not achieved. Lower values of the arterial stiffness index (ASI) and augmentation index (AIx) were found in patients of the first group of the 2nd subgroup receiving statins in comparison with patients of the 1st subgroup (p<0,05). In patients of the second group of the 2nd subgroup, while taking statins, there was a clear trend towards a lower ASI value compared to the 1st subgroup (p=0.07). Conclusions: the use of statins in patients with hypertension and AALE of varying severity, despite the lack of achievement of target levels of LDLC, contributed to a decrease in vascular stiffness, and, consequently, a decrease in cardiovascular risk.
CLINICAL IMMUNOLOGY, ALLERGOLOGY
Anaphylaxis is a severe, life-threatening, systemic hypersensitivity reaction that develops rapidly and can lead to death. The diagnosis of anaphylaxis continues to be primarily clinical. Therefore, a large number of studies are initiated annually aimed at a deeper study of the mechanisms of the development of this disease and the search for its biomarkers, which could become an important tool to facilitate the verification of diagnosis, prevention and risk assessment of repeated episodes of anaphylaxis, stratification of the severity of its course, the risk of life-threatening episodes of systemic reactions, and be important in the development of new therapeutic strategies. This review provides information on the currently available data on potential biomarkers of anaphylaxis.
OBSTETRICS AND GYNECOLOGY
Endometrial polyps are the most commonly observed pathological finding in the uterus. However, to date, there is little data regarding the factors for the development of endometrial polyps in reproductive-age women. This fact determined the direction of our study. A search was conducted among scientific papers in the Science Direct, CochraneLibrary, PubMed databases by keywords (polyps, endometrium, risk factors, reproductive age) for 1994–2022. As a result of the analysis of the scientific literature, we came to the following conclusions: 1. The prevalence of endometrial polyps depends on the studied population, while the actual prevalence is difficult to determine, since the endometrial polyps can be asymptomatic and regress over time. 2. Implementation of endometrial polyps, apparently, depend not on one, but on many factors: genetic, hormonal, metabolic, medicinal. 3. Increasing the amount of endogenous estrogen, the introduction of exogenous estrogen without progesterone component and age are the most important predisposing risk factors for the development of endometrial polyps.
Objective: to determine prognostic significance of low molecular weight metabolites in women with missed abortion. Material and methods: the research included 100 women of reproductive age, 79 of them with missed abortion diagnosed by ultrasound and 21 with progressive pregnancy who were admitted for an artificial abortion. All women underwent immunohistochemical studies of the endometrium and organic acids in blood serum and endometrium were determined by HPLC. Reliably significant organic acids in blood serum and endometrium, associated with metabolic disorders of fatty acids, amino acids, as well as intermediate metabolites in the Krebs cycle. Statistical analysis of the obtained data was performed using the STATISTICA® for Windows, Release 6.0 module package from StatSoft® Inc., USA (2003), serial number AXAR802D898511FA. Results: statistically significant changes were revealed in the profile of organic acids in the studied women at the levels of lactic, pyruvic and 4-hydroxyphenylpyruvic acids. In women with missed abortion, the change in the lactate / pyruvate. In all women with missed abortion, 4-hydroxyphenylacetic were determined, in contrast to women with a progressing pregnancy, combined with morpho-immuno-histochemical features (pronounced focal necrosis, venous fullness, lymphohistiocytic infiltration, increased levels of HLA-DR, CD 16, CD20 expression, reduced VEGF and LIF expression). Conclusion: missed abortion is associated with the accumulation of intermediate metabolites of tyrosine catabolism (4-hydroxyphenyacetic, 4-hydroxyphenylpyruvic and homogentizic acids), which, despite normal levels of TSH and T4, may reflect organ dysfunction. Timely correction of iodine deficiency in the pre-conception period after missed abortion can be a criterion for a successful subsequent pregnancy. Overcoming iodine deficiency potentiates the possibility of a conceptual restoration of fertility after a previous NB.
Currently, the medical community has accumulated significant experience in the use of endovascular methods in obstetric practice to achieve hemostasis and prevent massive hemorrhage, including in patients with placenta accreta spectrum (PAS) disorders. Objective — to evaluate the effectiveness of various methods of uterine devascularization in reducing blood loss during caesarean section in patients with PAS. In this review, we analyzed relevant literature and assessed the quality of clinical trials based on a systematic search in the Embase, PubMed, Web of Science, and Cochrane Library databases. The review presents an overview of modern methods of uterine devascularization aimed at reducing intraoperative blood loss in patients with PAS. A comparative analysis of the effectiveness of such methods of uterine devascularization as temporary balloon occlusion of the internal iliac arteries, common iliac arteries, abdominal aorta, as well as arterial compression using distal hemostasis was carried out. We evaluated effectiveness of the methods by such indicators as the mean amount of blood loss and the frequency of hysterectomy. The most effective methods of hemostasis in patients with PAS are temporary balloon occlusion of the abdominal aorta and the method of distal hemostasis. At the same time, there is still no ideal method for uterine devascularization in PAS, and clinical research in this direction should be continued.
INTERNAL DISEASES
Objective: to study the comorbid background and mortality structure of patients with rheumatoid arthritis (RA) in the Stavropol region in a cohort of patients of the Stavropol Regional Clinical Hospital (SRCH) within the period 2015–2021. Materials and methods: There was carried out systematic review of the literature. There was carried out the analysis of the protocols of autopsies in the pathoanatomical department of the SRCH within 2015-2021. There were studied the comorbidity component and lethal outcomes of patients with RA in the pathoanatomical diagnosis. Results: the structure of the comorbid pathology of RA patients in the SRCH cohort included coronary heart disease (CHD), autoimmune thyroiditis (AT), respiratory diseases (RD), hypertension (HT), “Blastomatosis”, diabetes mellitus (DM), COVID-19 infection. The comorbidity profile of patients with RA in decreasing order of the incidence of the pathological condition was as follows: CHD (35.29%) > RD (29.41%) > (“Blastomatosis”, СOVID-19 by 11.75%) > (AT, HT, DM by 5.88%). The structure of the conditions that led to the death of patients with RA included: acute myocardial infarction (40.0%), hemorrhagic stroke (6.67%), breast cancer (13.33%), thyroid cancer (6.67%), viral pneumonia (20.0%), sepsis (13.33%). Conclusions: the data obtained provide information that can be used by rheumatologists to optimize the strategy for managing RA and the risk of comorbid conditions.
Infectious endocarditis is a formidable disease characterized by an extremely unfavorable prognosis in its natural course. Analyzing the literature data, it can be noted that the frequency of infectious endocarditis in the Russian Federation has relatively high prevalence rates in relation to other countries. Currently, the problem of early diagnosis of infectious endocarditis remains relevant. Despite the fact that the diagnosis of infectious endocarditis has improved, mainly as a result of the improvement of echocardiographic and microbiological approaches, the introduction of new antibacterial drugs and cardiac surgery technologies into clinical practice, the clinical picture, changes in laboratory parameters can lead to the exclusion of immuno-inflammatory, rheumatic, oncological, hematological diseases, complicating and delaying the diagnosis of infectious endocarditis. The first clinical signs of infectious endocarditis may be nonspecific, and the disease remains unrecognized for weeks or even months. The high frequency of thrombotic, thrombohemorrhagic complications indicates profound changes in the hemostasis system in infectious endocarditis and the need to disclose the pathogenesis of these disorders. The combination of these factors led to the late diagnosis of this disease in the patient. The aim of the study is to study the possibility of improving the results of diagnosis and therapy of patients with infectious endocarditis in clinical practice.
PAEDIATRICS
Scientifically based and experimentally confirmed data on the morphogenesis of the lymphatic system are necessary to clarify critical periods of development characterized by an increased risk of congenital anomalies of the lymphatic system in order to plan and implement effective prevention, diagnosis and correction of related abnormalities. Among the studied anomalies of lymphatic vessels, lymphangioma is most often mentioned — a congenital benign tumor consisting of many cysts of various sizes. Detection of primary fetal lymphangioma in the early stages of intrauterine development is extremely rare. The purpose of the study: to report a case of early diagnosis of congenital cystic lymphangioma and lymphedema of the left lower limb of the fetus. Congenital (primary) peripheral lymphedema, limb lymphangioma is associated with a malformation of the lymphatic system. Taking into account the fact that operative methods of correction of all types of primary lymphedema are considered unreasonable and ineffective, the main attention requires timely detection of this congenital malformation during screening studies of the fetus and the issuance of recommendations for the management of pregnancy, up to termination for medical reasons. It is necessary to raise the issue of genetic counseling of the couple and conducting the necessary genetic studies. The use of modern diagnostic methods allows for the prevention and treatment of abnormalities in the development of the lymphatic system at an earlier stage of the intrauterine period.
ISSN 2618-7876 (Online)