Scroll to:
Endometriosis of the uterine scar after cesarean section is like an invisible disease. Difficulties in diagnosis
https://doi.org/10.21886/2219-8075-2025-16-3-5-15
Abstract
Objective: to analyze cases of surgical correction of uterine scar failure aſter cesarean section, to determine the frequency of detection of endometriosis of the uterine scar according to histological findings and to identify the effectiveness of diagnostic methods.
Materials and methods: a retrospective analysis of the medical records of 52 patients from January 2022 to December 2024, who underwent surgical correction of a uterine scar aſter cesarean section with its failure, was carried out.
Results: our correlation analysis revealed that in most cases, uterine scar endometriosis was asymptomatic, however, in rare cases, a connection was observed between patients’ complaints of abnormal uterine bleeding (AUB) and uterine scar endometriosis. The absence of complaints in endometriosis confirms its asymptomatic course. Due to the latent and difficult to diagnose course of the disease, as part of pre-pregnancy preparation in women with a uterine scar, it is necessary to use a comprehensive diagnostic approach, combining non-invasive methods with hysteroscopy, to increase the frequency of detection of scar endometriosis. This will allow timely surgical treatment and prevent disease progression.
Conclusion: ultrasound examination as a method for diagnosing endometriosis of the uterine scar aſter ACS showed low sensitivity in detecting this pathology, despite the high resolution of modern ultrasound devices. Magnetic resonance imaging and diagnostic hysteroscopy are recommended as diagnostic methods. In turn, a combination of methods for diagnosing a scar on the uterus aſter ACS as part of pregravid preparation will make it possible to increase the frequency of detecting endometriosis of the uterine scar and will allow timely surgical treatment of the identified pathology.
For citations:
Grigoryants A.A., Avrutskaya V.V., Krukier I.I., Levkovich M.A., Ermolova M.V. Endometriosis of the uterine scar after cesarean section is like an invisible disease. Difficulties in diagnosis. Medical Herald of the South of Russia. 2025;16(3):5-15. (In Russ.) https://doi.org/10.21886/2219-8075-2025-16-3-5-15
Introduction
At present, there is a steady increase in the incidence of cesarean section (CS), which has consequently led to a rise in postoperative complications, one of the most significant being uterine scar dehiscence [1][2]. The prevalence of uterine scar defects is reported to range from 35.0% to 60.0% among women of reproductive age with a history of cesarean delivery [3][4][5][6].
In cases of uterine scar dehiscence accompanied by niche formation, the risk of serious obstetric complications is markedly elevated. These complications include uterine rupture at the site of the scar, cesarean scar pregnancy, placental implantation into the scar area, and cesarean scar endometriosis [7]. Clinically, such patients often present with abnormal uterine bleeding, chronic pelvic pain, or infertility [8][9][10].
One relatively rare but clinically significant cause of uterine scar dehiscence after a CS is endometriosis [11]. According to published studies, cesarean scar endometriosis accounts for approximately 0.42–4.0% of all endometriosis cases [12][13].
Endometriosis is a chronic disease characterized by the proliferation of endometrial-like tissue outside the uterine cavity, typically affecting women of reproductive age1 [14][15].
Only a limited number of clinical cases of endometriosis involving a surgical uterine scar were described in the medical literature, making this form of the disease relatively rare. However, with the increasing prevalence of endometriosis among women of reproductive age and the growing number of cesarean deliveries, the incidence of postoperative scar endometriosis has risen accordingly. Data suggest that patients with two cesarean deliveries are more likely to develop scar endometriosis than those with a single CS [16].
A review of the literature indicates that cesarean delivery may serve as a triggering mechanism for the development of scar endometriosis due to iatrogenic implantation of endometrial cells into the surgical wound, followed by their proliferation and cystic transformation [17].
Scar endometriosis may be an independent factor contributing to the development of uterine scar dehiscence. Several authors have suggested that postoperative scar endometriosis can impair wound healing and predispose to the formation of a deficient uterine scar [18].
Importantly, the diagnosis of cesarean scar endometriosis remains challenging due to the lack of specific imaging features on ultrasound and magnetic resonance imaging (MRI). Hysteroscopy is considered the most informative diagnostic tool, revealing endometrial invaginations from the uterine cavity, irregular or eroded scar contours, and open-type endometriotic tracts containing characteristic “chocolate-like” fluid [19]. Nevertheless, in many cases, the diagnosis of scar endometriosis is made incidentally through histological examination [20].
The aim of this study was to analyze cases of surgical correction of uterine scar dehiscence following CS, to determine the incidence of cesarean scar endometriosis based on histopathological findings, and to evaluate the diagnostic efficacy of different imaging and endoscopic methods.
Materials and Methods
A retrospective analysis of 52 medical case histories was conducted over the period from January 2022 to December 2024.
Inclusion criteria: patients who underwent surgical correction of uterine scar dehiscence after a CS and were planning pregnancy.
Exclusion criteria: patients with uterine scars resulting from conservative myomectomy.
The following parameters were analyzed: patient age; the number of previous CSs; the presence of postoperative complications according to obstetric discharge summaries; presenting complaints at the time of hospital admission; results of pelvic ultrasound and MRI; findings from diagnostic hysteroscopy; histopathological reports.
Statistical analysis was performed using the R programming language within the RStudio environment, version 1.1.456 (open-source software available at https://github.com/rstudio/rstudio).
Correlations between dichotomous categorical variables were assessed using the contingency coefficient, and statistical significance was verified by the two-tailed Fisher’s exact test. For non-dichotomous categorical data, associations were evaluated using the Pearson and Tschuprow coefficients of contingency. A p-value < 0.05 was considered statistically significant.
Results
Analysis of patients’ medical histories revealed that the majority of participants (33; 63.5%) had undergone a single cesarean delivery, 12 patients (23.1%) had undergone two CSs, and 7 (13.4%) had experienced three CSs. The mean age of patients was 29.0 ± 2.3 years.
The frequency of postoperative complications after a CS is presented in Table 1.
Таблица / Table 1
Частота осложнений после ОКС
Frequency of complications after ACS
|
1 ОКС/ACS (n=33) |
2 ОКС/ACS (n=12) |
3 ОКС/ACS (n=7) |
|
|
Эндометрит Endometritis |
5 (15,2%) |
2 (16,7%) |
3 (42,9%) |
|
Гематомы в рубце Hematomas in the scar |
1 (3%) |
2 (16,7%) |
2 (28,6%) |
When analyzing the patients’ complaints prior to planned surgical correction of the uterine scar, it was found that more than half of the women (36; 69.2%) reported no symptoms, while 10 patients (19.2%) complained of menstrual irregularities in the form of abnormal uterine bleeding (AUB), and 6 women (11.5%) reported localized pain in the scar area.
According to ultrasound (US) findings, cesarean scar endometriosis was diagnosed in 2 patients (3.8%), and according to MRI in 3 patients (5.8%). The mean preserved myometrial thickness above the apex of the scar was 1.5 ± 0.5 mm on ultrasound and 1.0 ± 0.5 mm on MRI.
Diagnostic hysteroscopy revealed features of scar endometriosis in 6 patients (11.6%). Histological examination of the excised uterine scar confirmed the presence of endometriosis in 15 cases (28.8%).
Thus, in 9 patients (17.3%), cesarean scar endometriosis was identified only by histological examination, whereas ultrasound, MRI, and hysteroscopy did not reveal this pathology. According to histological data, the presence of scar endometriosis was associated with the number of cesarean deliveries (Figure 1).
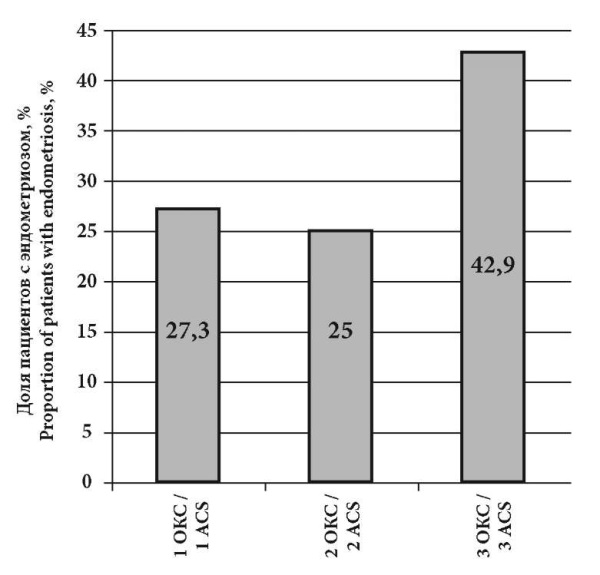
Рисунок 1. Доля пациентов с различным количеством ОКС в анамнезе с диагнозом «Эндометриоз рубца» по результатам гистологического заключения (в %)
Figure 1. The proportion of patients with different numbers of ACS in the anamnesis with a diagnosis of scar endometriosis according to the results of the histological report (in %)
Given the high incidence of scar endometriosis detected postoperatively, a correlation analysis was performed between the patients’ clinical complaints and histological findings. The evaluated clinical manifestations included AUB and pain localized to the cesarean scar. Statistical significance was assessed using the two-tailed Fisher’s exact test (Table 2).
Таблица / Table 2
Результаты корреляционного анализа жалоб пациенток и наличия эндометриоза по гистологическому заключению
Results of correlation analysis of patients' complaints and presence of endometriosis according to histological conclusion
|
Корреляция Correlation |
Используемый коэффициент корреляции Correlation coefficient used |
Коэффициент корреляции (r) Correlation coefficient (r) |
Статистическая значимость Statistical significance |
|
Нарушения менструального цикла / Эндометриоз рубца Menstrual disorders / Endometriosis of the scar |
Коэффициент контингенции Contingency factor |
0,436 |
P<0,054 |
|
Жалобы на боли в области рубца / Эндометриоз рубца Complaints of pain in the scar area / Endometriosis of the scar |
0,169 |
P<0,338 |
|
|
Нарушения менструального цикла + Жалобы на боли в области рубца / Эндометриоз рубца Menstrual cycle disorders + Complaints of pain in the scar area / Endometriosis of the scar |
0,207 |
P<0,196 |
|
|
Без жалоб / Эндометриоз рубца No complaints / Endometriosis of the scar |
0,451 |
P<0,053 |
Примечание: жирным выделено статистически значимое различие коэффициента корреляций (р<0,05).
Note: statistically significant differences in the correlation coefficient (p<0.05) are highlighted in bold.
The analysis demonstrated statistically significant correlations between patient complaints of abnormal uterine bleeding and the presence of scar endometriosis confirmed by histology. In addition, a correlation was found between histologically confirmed scar endometriosis and the absence of clinical symptoms (Figure 2).
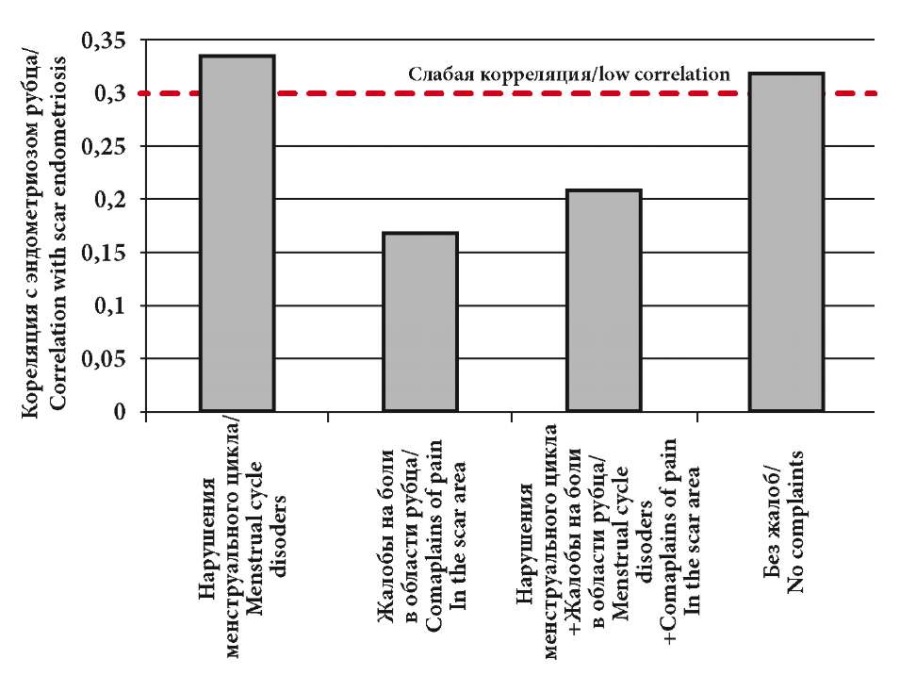
Рисунок 2. Корреляционный анализ жалоб пациенток и наличия эндометриоза
Figure 2. Correlation analysis of patient complaints and the presence of endometriosis
A further analysis was conducted to identify possible causes of scar endometriosis formation depending on post-cesarean complications, such as scar hematoma or postpartum endometritis. Correlation was calculated using the two-tailed Fisher’s exact test (Table 3).
Таблица / Table 3
Результаты корреляционного анализа осложнений после ОКС и эндометриоза рубца по данным гистологического исследования
Results of correlation analysis of complications after ACS and scar endometriosis according to histological examination data
|
Корреляция Correlation |
Используемый коэффициент корреляции Correlation coefficient used |
Коэффициент корреляции (r) Correlation coefficient (r) |
Статистическая значимость корреляции Statistical significance |
|
Микрогематомы в области рубца / Эндометриоз рубца Microhematomas in the scar area / Endometriosis of the scar |
Коэффициент контингенции Contingency factor |
0,097 |
p<0,659 |
|
Эндометрит/ Эндометриоз рубца Endometritis/Rum Endometriosis |
0,095 |
p<0,704 |
Примечание: жирным выделено статистически значимое различие коэффициента корреляций (р<0,05).
Note: statistically significant differences in the correlation coefficient (p<0.05) are highlighted in bold.
The analysis revealed no statistically significant associations between postoperative complications following a CS and the development of scar endometriosis (Figure 3).
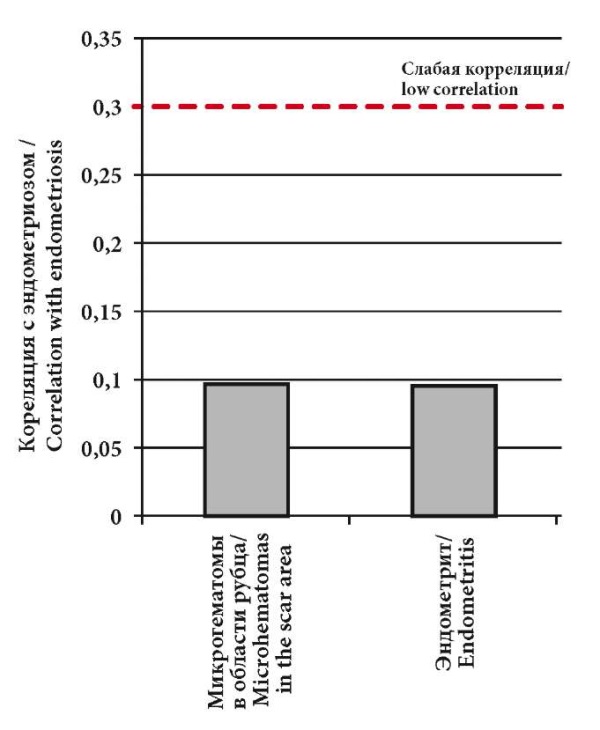
Рисунок 3. Корреляция осложнений после ОКС и эндометриоза рубца по данным гистологического исследования
Figure 3. Correlation of complications after ACS and scar endometriosis according to histological examination data
A correlation analysis was also performed between the diagnostic methods (hysteroscopy, ultrasound, and MRI) and histologically confirmed cases of scar endometriosis.
The statistical significance of the correlation coefficients was assessed using the two-tailed Fisher’s exact test (Table 4).
Таблица / Table 4
Результаты корреляционного анализа различных методов диагностики эндометриоза с данными гистологического исследования
Results of correlation analysis of various methods of endometriosis diagnostics with histological examination data
|
Корреляция Correlation |
Используемый коэффициент корреляции Correlation coefficient used |
Коэффициент корреляции (r) Correlation coefficient (r) |
Статистическая значимость корреляции Statistical significance |
|
Эндометриоз рубца (гистероскопия) / Эндометриоз рубца (гистология) Endometriosis of the scar (hysteroscopy) /Endometriosis of the scar (histology) |
Коэффициент контингенции Contingency factor |
0,533 |
P<0,024 |
|
Эндометриоз рубца (МРТ ОМТ) / Эндометриоз рубца (гистология) Endometriosis of the scar (MRI of the pelvic organs) /Endometriosis of the scar (histology) |
0,389 |
P<0,021 |
|
|
Эндометриоз рубца (УЗИ ОМТ) / Эндометриоз рубца (гистология) Endometriosis of the scar (Ultrasound of the pelvic organs) / Endometriosis of the scar (histology) |
0,314 |
P<0,079 |
|
|
Эндометриоз рубца (гистероскопия + МРТ ОМТ) / Эндометриоз рубца (гистология) Endometriosis of the scar (hysteroscopy + MRI of the pelvic organs) / Endometriosis of the scar (histology) |
0,533 |
P<0,024 |
|
|
Эндометриоз рубца (гистероскопия + УЗИ ОМТ) / Эндометриоз рубца (гистология) Endometriosis of the scar (hysteroscopy + Ultrasound of the pelvic organs) / Endometriosis of the scar (histology) |
0,605 |
P<0,024 |
|
|
Эндометриоз рубца (МРТ ОМТ + УЗИ ОМТ) / Эндометриоз рубца (гистология) Endometriosis of the scar (MRI of the pelvic organs + ultrasound of the pelvic organs / Endometriosis of the scar (histology) |
0,453 |
P<0,005 |
|
|
Эндометриоз рубца (гистероскопия + МРТ ОМТ + УЗИ ОМТ) / Эндометриоз рубца (гистология) Endometriosis of the scar (hysteroscopy + MRI of the pelvic organs + ultrasound of the pelvic organs) / Endometriosis of the scar (histology) |
0,605 |
P<0,024 |
Примечание: жирным выделено статистически значимое различие коэффициента корреляций (р<0,05).
Note: statistically significant differences in the correlation coefficient (p<0.05) are highlighted in bold.
A statistically significant moderate correlation was established between the results of hysteroscopy and the histological findings of endometriosis (Figure 4). In addition, a statistically significant moderate correlation was identified when combined diagnostic approaches were used — specifically, hysteroscopy with pelvic MRI, hysteroscopy with pelvic ultrasound, and the combination of hysteroscopy, MRI, and ultrasound. Statistically significant correlations of moderate strength were found primarily when two or more diagnostic modalities were combined.
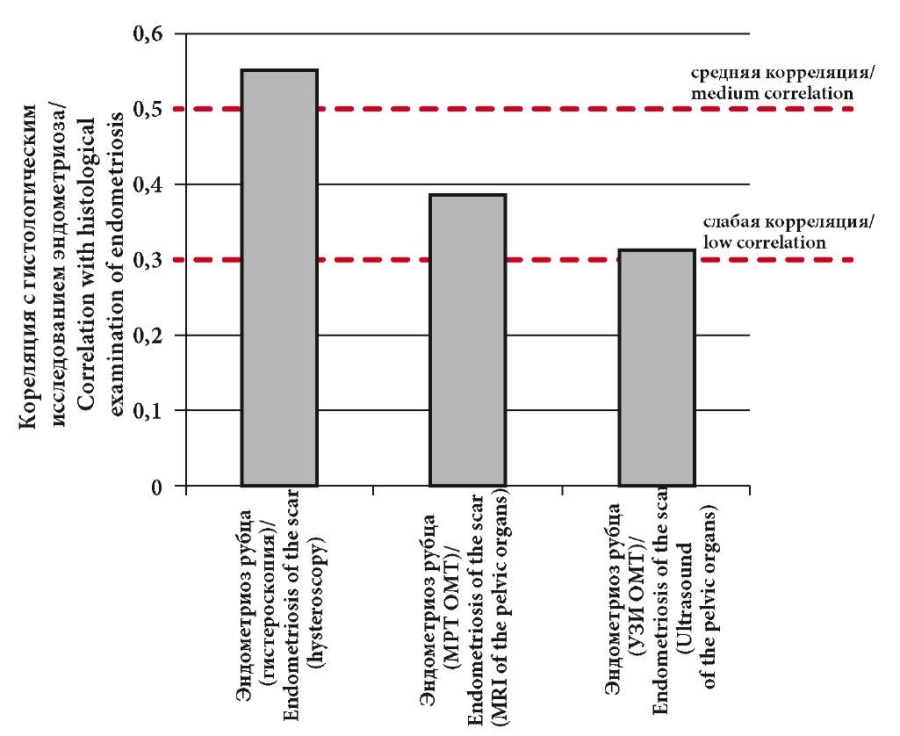
Рисунок 4. Корреляции различных методов диагностики эндометриоза с результатами гистологического исследования
Figure 4. Correlations of various methods of endometriosis diagnosis with the results of histological examination
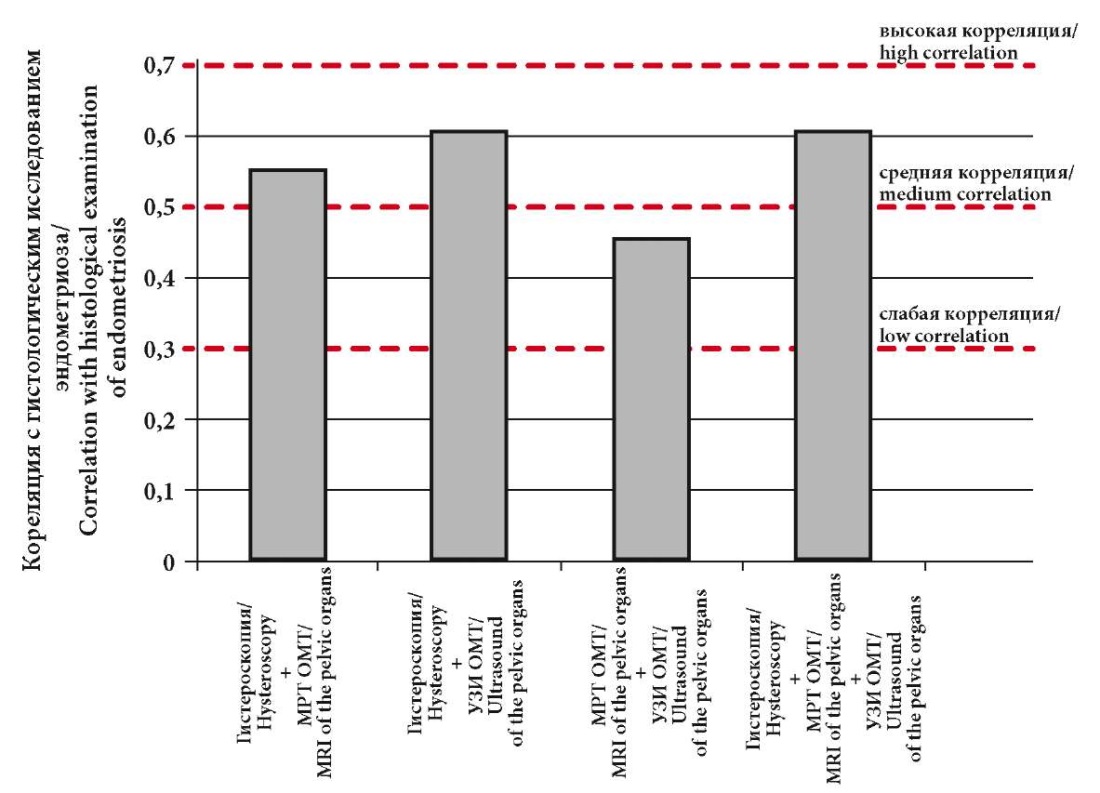
Рисунок 5. Корреляция различных комбинаций методов диагностики эндометриоза с результатами гистологического исследования
Figure 5. Correlation of various combinations of endometriosis diagnostic methods with the results of histological examination
Nevertheless, histological examination remains the gold standard for confirming the diagnosis of “Cesarean scar endometriosis”.
A comparative evaluation of various diagnostic methods for cesarean scar endometriosis was performed using the following parameters: accuracy, sensitivity, and specificity (Table 5).
Таблица / Table 5
Качественные характеристики различных методов диагностирования эндометриоза
Qualitative characteristics of various methods for diagnosing endometriosis
|
Метод диагностики Diagnostic method |
Качественные характеристики |
||
|
Точность, % Accuracy, % |
Чувствительность, % Sensitivity, % |
Специфичность, % Specificity, % |
|
|
УЗИ ОМТ Ultrasound of the pelvic organs |
100 |
13,33 |
100 |
|
МРТ ОМТ MRI of the pelvic organs |
100 |
20 |
100 |
|
Гистероскопия Hysteroscopy |
100 |
40 |
100 |
|
УЗИ ОМТ + МРТ ОМТ Ultrasound of the pelvic organs + MRI of the pelvic organs |
100 |
26,67 |
100 |
|
УЗИ ОМТ + Гистероскопия Ultrasound of the pelvic organs + Hysteroscopy |
100 |
46,67 |
100 |
|
МРТ ОМТ + Гистероскопия MRI of the pelvic organs + Hysteroscopy |
100 |
40 |
100 |
|
УЗИ ОМТ + МРТ ОМТ + Гистероскопия Ultrasound of the pelvic organs + MRI of the pelvic organs + Hysteroscopy |
100 |
46,67 |
100 |
|
Гистология Histology |
100 |
100 |
100 |
All methods demonstrated high accuracy and specificity, but low sensitivity, which is the key limiting factor in diagnosis. Only histological examination provided absolute diagnostic accuracy.
Discussion
The results of this study indicate that cesarean scar endometriosis remains a hidden and insufficiently studied condition. The underlying mechanisms of its development are still unclear and require further investigation.
In all patients diagnosed with scar endometriosis, there were no identifiable causal relationships with postoperative complications following a CS. This finding supports the polyetiological nature of endometriosis pathogenesis and makes it impossible to predict its development.
Our study confirmed a significant association between AUB — one of the key clinical complaints — and histologically verified cesarean scar endometriosis. This association suggests that the presence of AUB may serve as an indirect diagnostic indicator of this pathology. However, the observed correlation between the absence of symptoms and histologically confirmed endometriosis further emphasizes that cesarean scar endometriosis can also occur asymptomatically, regardless of its location or extent.
It was found that patients with three CSs were diagnosed with scar endometriosis more frequently than those with one or two cesarean deliveries, supporting the implantation theory of disease development.
A significant correlation between hysteroscopic and histological findings was also demonstrated, confirming that hysteroscopy is a valuable component of preconceptional evaluation in women with uterine scars for the diagnosis of scar dehiscence and possible endometriotic involvement.
The present analysis shows that ultrasound alone is not sufficient for diagnosing cesarean scar endometriosis due to its low sensitivity and limited diagnostic value. However, combining ultrasound with diagnostic hysteroscopy substantially improves detection rates. Therefore, a comprehensive diagnostic approach incorporating noninvasive imaging modalities (MRI and ultrasound) together with hysteroscopy is strongly recommended.
Statistical analysis revealed the high accuracy and specificity of the diagnostic methods employed, indicating that current tools can identify only the most evident cases of scar endometriosis. Nevertheless, their sensitivity did not exceed 47%, highlighting the limitations of imaging techniques. Histological examination remains the only method providing absolute diagnostic certainty.
A review of both domestic and international literature revealed a lack of studies addressing the diagnostic challenges of cesarean scar endometriosis, which precluded a comparative analysis of our findings with those of other researchers.
Conclusion
Cesarean scar endometriosis warrants particular clinical attention, as its diagnosis remains a challenging and unresolved task.
According to the Clinical Guidelines “Postoperative Uterine Scar Requiring Medical Care During Pregnancy, Delivery, and the Postpartum Period”, approved by the Ministry of Health of the Russian Federation on September 6, 2024, ultrasound examination on days 7–9 of the menstrual cycle is recommended for women at risk of developing a clinically significant uterine scar niche. Despite the high resolution of modern ultrasound devices, this method has demonstrated low sensitivity in detecting cesarean scar endometriosis. As additional diagnostic tools, MRI and diagnostic hysteroscopy should be employed.
A combination of diagnostic modalities used during preconception assessment can enhance the detection rate of cesarean scar endometriosis and enable timely surgical management of the identified pathology.
The mainstay of diagnosis remains histopathological examination. Histological evaluation of excised scar tissue should be mandatory as histological confirmation of endometriosis allows clinicians to initiate targeted therapy aimed at reducing the risk of recurrence.
In conclusion, further clinical and morphological research is necessary to establish clear diagnostic criteria and to elucidate the etiopathogenic mechanisms underlying this rare but clinically significant condition.
1. Clinical Guidelines: Endometriosis. Russian Society of Obstetricians and Gynecologists, 2024; 60.
References
1. Szafarowska M, Biela M, Wichowska J, Sobociński K, Segiet-Święcicka A, et al. Symptoms and quality of life changes aſter hysteroscopic treatment in patients with symptomatic isthmocele-preliminary results. J Clin Med. 2021;10(13):2928. https://doi.org/10.3390/jcm10132928
2. Donnez O. Cesarean scar defects: management of an iatrogenic pathology whose prevalence has dramatically increased. FertilSteril. 2020;113(4):704-716. https://doi.org/10.1016/j.fertnstert.2020.01.037
3. Shao MJ, Hu M. A growing concern: cesarean scar defect and massive uterine bleeding. Journal of Clinical Case Reports. 2015;5(9):599-600.
4. Lisitsyna O.I., Shmakov R.G. Niches of the uterine scar aſter cesarean section: diagnosis, treatment, and outcomes. Akusherstvo i Ginekologiya/ Obstetrics and gynecology. 2019;(9):24-31. (In Russ.) https://doi.org/10.18565/aig.2019.9.24-31
5. Antila-Långsjö RM, Mäenpää JU, Huhtala HS, Tomás EI, Staff SM. Cesarean scar defect: a prospective study on risk factors. Am J Obstet Gynecol. 2018;219(5):458.e1-458.e8. https://doi.org/10.1016/j.ajog.2018.09.004
6. Zheng X, Yan J, Liu Z, Wang X, Xu R, et al. Safety and feasibility of trial of labor in pregnant women with cesarean scar diverticulum. J Int Med Res. 2020;48(9):300060520954993. https://doi.org/10.1177/0300060520954993
7. Buyanova S.N., Schukina N.A., Chechneva M.A., Puchkova N.V., Zemskova N.Yu., Torobaeva M.T. Pregnancy in the scar aſter cesarean section: the possibility of surgical correction. Russian Bulletin of Obstetrician-Gynecologist. 2020;20(6):65-70. (In Russ.) https://doi.org/10.17116/rosakush20202006165
8. Warshafsky C, Kirubarajan A, Chaikof M, Stere A, Chudawala U, et al. Preventing Isthmocele Aſter Cesarean Section (PICS): A Pilot Randomized Controlled Trial. J Obstet Gynaecol Can. 2022;44(11):1134-1135. https://doi.org/10.1016/j.jogc.2022.08.003
9. Torre A, Verspyck E, Hamamah S, Thomassin I, Thornton J, et al. Isthmocèle: définition, diagnostic, facteurs de risque, prévention, symptômes, complications, et traitements [Cesarean scare niche: Definition, diagnosis, risk factors, prevention, symptoms, adverse effects, and treatments]. Gynecol Obstet Fertil Senol. 2021;49(11):858-868. (In French) https://doi.org/10.1016/j.gofs.2021.06.003
10. Torobaeva M.T., Buyanova S.N., Puchkova N.V. Incompetent uterine scar aſter caesarean section as a separate nosology. Russian Bulletin of Obstetrician-Gynecologist. 2023;23(3):19-28. (In Russ.) https://doi.org/10.17116/rosakush20232303119
11. Telyakova M.I., Mikhelson A.A., Okulova E.O., Pogorelko D.V., Lazukina M.V. Clinical and anamnestic features of patients with endometriosis of an incompetent uterine scar after cesarian section. Russian Journal of Human Reproduction. 2022;28(5):100-106. (In Russ.) https://doi.org/10.17116/repro202228051100
12. Galimov O.V., Ziangirov R.A., Alimov V.A., Safin I.N., Khanov V.O., et al. Endometriosis of postoperative scar. Medical & Pharmaceutical Journal «Pulse». 2021;21(9):56-60. (In Russ.) https://doi.org/10.26787/nydha-2686-6838-2019-21-9-56-60
13. Buyanova S.N., Glebov T.A., Babunashvili E.L., Gukasyan S.A., Yudina N.V. Endometriosis of the anterior abdominal wall, perineum and vagina. Russian Bulletin of Obstetrician-Gynecologist. 2022;22(5):43-48. (In Russ.) https://doi.org/10.17116/rosakush20222205143
14. Li XY, Chao XP, Leng JH, Zhang W, Zhang JJ, et al. Risk factors for postoperative recurrence of ovarian endometriosis: longterm follow-up of 358 women. J Ovarian Res. 2019;12(1):79. https://doi.org/10.1186/s13048-019-0552-y
15. Grigoriants A.A., Krukier I.I., Avrutskaya V.V., Ermolova N.V., Levkovich M.A., Kuznetsova I.V. External genital endometriosis: current concepts about the development, diagnosis, therapy. Women’s clinic. 2023;(3):6-14. (In Russ.) eLIBRARY ID: 59337495 EDN: JXGEYM
16. Grigoryants A.A., Avrutskaya V.V., Krukier I.I., Aksenenko D.V. The effectiveness of surgical and conservative treatment of patients with endometriosis of the uterine scar after cesarean section. Medical alphabet. 2024;(19):28-32. (In Russ.) https://doi.org/10.33667/2078-5631-2024-19-28-32
17. Youssef AT. The ultrasound of subcutaneous extrapelvic endometriosis. J Ultrason. 2020;20(82):e176-e180. https://doi.org/10.15557/jou.2020.0029
18. Khasanov A.A., Zhuravleva V.I., Galautdinova D.I. Longterm outcomes of reconstructive plasty of incompetent uterine scar by vaginal access. Practical medicine. 2017;(8):168-170. (In Russ.). eLIBRARY ID: 30060643 EDN: ZHVGBT
19. Nozhnitseva O.N., Semenov I.A., Bezhenar V.F. The scar on the uterus aſter cesarean section and the optimal algorithm for diagnostics. Diagnostic radiology and radiotherapy. 2019;(2):85-90. (In Russ.) https://doi.org/10.22328/2079-5343-2019-10-2-85-90
20. Mishina A.E., Gladun S.E., Zastavnitsky G.M., Mishin I.V. Endometriosis in postoperative scar. Novosti Khirurgii. 2013;21(3):116-119. (In Russ.) eLIBRARY ID: 19078916 EDN: OLTPGD
About the Authors
A. A. GrigoryantsRussian Federation
Armen A. Grigoryants, Cand. Sci. (Med.), Аssociate Рrofessor at the Department of Obstetrics and Gynecology No. 2
Stavropol
Competing Interests:
Authors declares no conflict of interest
V. V. Avrutskaya
Russian Federation
Valeriya V. Avrutskaya, Dr. Sci. (Med.), Professor, Professor of the Department of Obstetrics and Gynecology No. 2
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest
I. I. Krukier
Russian Federation
Irina I. Krukier, Dr. Sci. (Bio.), Professor of the Department of General and Clinical Biochemistry No. 1
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest
M. A. Levkovich
Russian Federation
Marina A. Levkovich, Dr. Sci. (Med.), Associate Professor, Leading Researcher of the Scientific Department «NIAP»
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest
M. V. Ermolova
Russian Federation
Natalia V. Ermolova, Dr. Sci. (Med.), Professor, Professor of the Department of Obstetrics and Gynecology No. 1
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest
Review
For citations:
Grigoryants A.A., Avrutskaya V.V., Krukier I.I., Levkovich M.A., Ermolova M.V. Endometriosis of the uterine scar after cesarean section is like an invisible disease. Difficulties in diagnosis. Medical Herald of the South of Russia. 2025;16(3):5-15. (In Russ.) https://doi.org/10.21886/2219-8075-2025-16-3-5-15







































