Scroll to:
Clinical and experimental parallels in the substantiation of the method of hernioplasty of postoperative ventral hernias of median localization
https://doi.org/10.21886/2219-8075-2024-15-1-108-114
Abstract
Objective: development, clinical application of a new original method of hernioplasty of median postoperative ventral hernias and biomechanical experimental substantiation of the effectiveness of this method.
Materials and methods: the method of hernioplasty of median postoperative ventral hernias with strengthening of fascial-aponeurotic structures of the anterior abdominal wall was developed and clinically tested on 63 patients. An anatomical experiment was performed in which the biomechanical parameters of the reinforced scar-altered structures of the median parts of the anterior abdominal wall were studied according to the method developed by us.
Results: an increase in the biomechanical parameters of the median structures reinforced by the original method with a frame thread was found: the strength limit of the fascia — by 59.4%, and the modulus of elasticity — by 40.2%, compared with the scar-altered fascia in herniators. These results suggest a confident prevention of recurrence of herniation when using this technique. This assumption was confirmed after the introduction of the technique into clinical practice. In all 63 observed patients, there is no recurrence of herniation for 1-5 years. There were no significant complications of the course of the early postoperative period associated with the applied method of plastic surgery. The method is characterized by material and financial accessibility, the absence of complex technical manipulations that increase the duration of hernioplasty.
Conclusions: the effectiveness in preventing recurrence of herniation, accessibility and simplicity of the proposed method of surgical treatment of postoperative and recurrent ventral hernias allows us to recommend it for wide clinical use.
For citations:
Korobka V.L., Tatyanchenko V.K., Dabliz R.O., Tolstopyatov S.V., Gonchar M.V., Kletz I.S. Clinical and experimental parallels in the substantiation of the method of hernioplasty of postoperative ventral hernias of median localization. Medical Herald of the South of Russia. 2024;15(1):108-114. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-1-108-114
Introduction
A ventral incisional hernia is an abdominal wall hernia that occurs after a previous laparotomy. It occurs when the internal organs protrude through a defect covered by the parietal peritoneum, in the musculoaponeurotic layer at the site of the postoperative scar1,2. It is a common complication of abdominal surgery with an estimated incidence ranging from 2% to 28% [1][2][3].
Ventral incisional hernias are commonly caused by inadequate wound closure and a poor surgical approach. This includes performing excessively large incisions without considering the topography and anatomy of the anterior abdominal wall, as well as transecting muscles, main vessels, and nerves [4][5]. It is important to note that postoperative hernias can often cause more distress to patients than the primary disease that necessitated laparotomy, resulting in the need for repeated surgical interventions [6][7].
Current guidelines recommend using mesh-based tension-free repairs as the first choice for managing ventral incisional hernias, particularly large ones [2][7]. Proper mesh placement and fixation are crucial in tension-free hernia repair as they determine the effectiveness of the created structure and prevent the risk of recurrence [7][8].
The aim of the study is to develop and implement a new original repair technique for median ventral incisional hernias and to evaluate its effectiveness through biomechanical testing.
Materials and Methods
This study is based on experimental results [9] obtained from anatomical and morphological examinations of the fascial structures of the median abdominal wall using Tatianchenko's technique3[10]. The authors have previously tested the biomechanical properties of native specimens of rectus abdominis fascial structures and specimens of hernial fascial scars using the ISS-500 Test Station (National Register of Measuring Equipment No. 16540-97) and Scaima ZF-500 Force Sensor (France). The tensile strength (Ϭ) and elasticity modulus (E) were measured. These values were calculated by formulas:
Ϭ=P/F, E=Ϭ/e, e=∆L/L,
where P is the load on the specimen; F is the cross-sectional area of the specimen; L is the specimen length; ∆L is the absolute elongation; and e is the longitudinal strain. It was found that the tensile strength and elasticity modulus of the hernial scar specimens in the anterior abdominal wall decreased by 1.5–1.9 times and 1.9–2.5 times, respectively, compared to the native specimens. Therefore, the previous study identified the necessity of enhancing the strength of scar tissue in hernia patients during hernial repair to prevent recurrences.
The authors of this study have developed and clinically tested a repair technique for median ventral incisional hernias. The technique involves reinforcing fascial aponeurotic structures of the anterior abdominal wall (Russian Patent No. 2685682)4.
The proposed technique involves several stages, including excision of the postoperative scar, separation and management of the hernial sac, peritoneal suturing, and mesh repair of the hernial defect. U-shaped sutures are used to fix a surgical mesh, and a thick loop-shaped synthetic nonabsorbable suture (referred to as a “core suture”) is delivered preperitoneally at 1.5–2 cm from the edge of the hernial orifice. The suture ends are then removed from the edges. Both sides of the hernial orifice are closed with U-shaped sutures, capturing the core suture under the muscles. The suture distance should be between 1.5 cm and 2.5 cm. A surgical mesh, with the same longitudinal size as the hernial defect and a lateral size exceeding 0.5 cm of the U-shaped suture line, is used to cover the muscles. The mesh is secured using the pre-formed U-shaped sutures. As the sutures are tied, the core suture loop is pulled up and tightened. Once the mesh is fixed in place, the core suture loop is tied off.
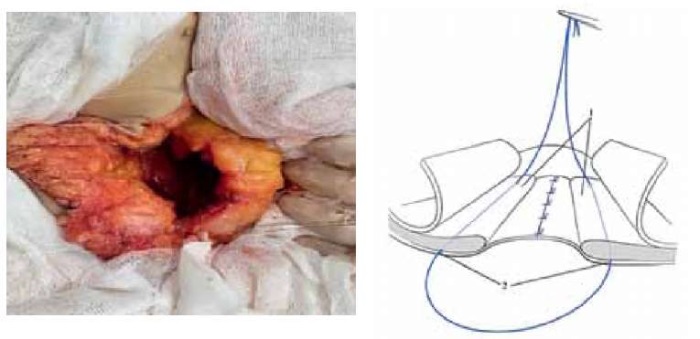
Figure 1. Anatomical experiment and diagram.
Carrying out a non-absorbable frame thread
and creating a loop around the circumference of the hernial gate.
Рисунок 1. Анатомический эксперимент и схема.
Проведение нерассасывающейся каркасной нити
и создание петли по окружности грыжевых ворот.
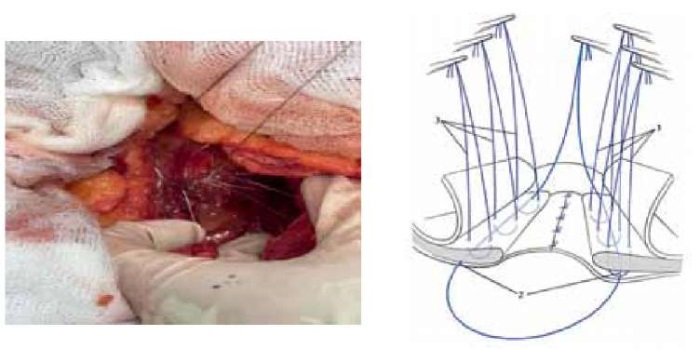
Figure 2. Anatomical experiment and diagram.
Carrying out threads of U-shaped seams with the capture of the frame thread.
Рисунок 2. Анатомический эксперимент и схема.
Проведение нитей П-образных швов с захватом каркасной нити.
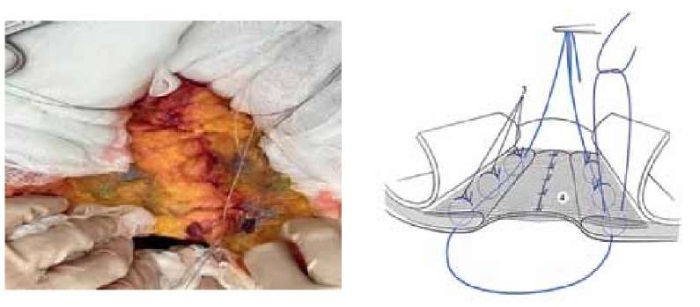
Figure 3. Anatomical experiment and diagram.
Fixation of the mesh endoprosthesis with U-shaped sutures.
Рисунок 3. Анатомический эксперимент и схема.
Фиксация сетчатого эндопротеза П-образными швами.
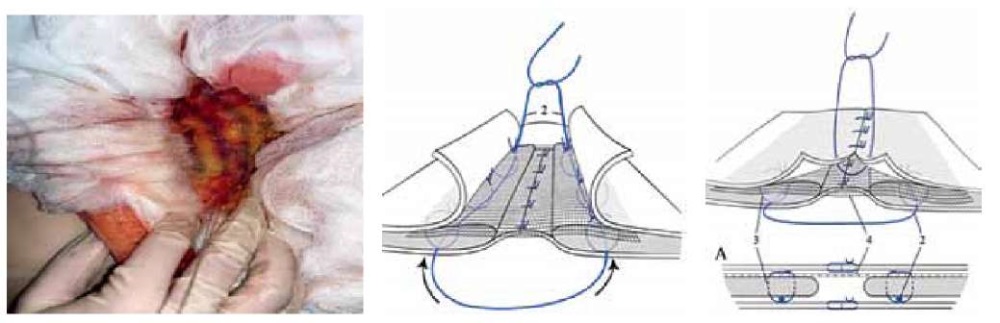
Figure 4. Anatomical experiment and diagram.
Tightening of the frame thread and its fixation. The final type of operation.
A: cross section of the anterior abdominal wall.
Рисунок 4. Анатомический эксперимент и схема.
Подтягивание каркасной нити и её фиксация. Окончательный вид операции.
А: поперечный срез передней брюшной стенки.
Figure 4 displays the final view of the structure that was created. The mesh is fixed in place by passing the core suture through the U-shaped sutures. This prevents the sutures from erupting and distributes intra-abdominal pressure evenly along the suture line. As with the original method, this technique ensures greater elasticity and strength of the repaired structure.
During the final stage of the anatomical experiment, the tensile strength and elasticity modulus of the median anterior abdominal wall scars reinforced using the proposed ISS-500 Test Station technique were compared to those of native and scar specimens (Table 1).
Таблица / Table 1
Сравнительная оценка биомеханических параметров
различных видов фасциальных структур передней брюшной стенки
Comparative evaluation of biomechanical parameters
of various types of fascial structures of the anterior abdominal wall
|
Вид ткани Type of tissue |
Биомеханический параметр Biomechanical parameter |
|
|
Предел прочности, кгс/см² Tensile strength, kgf/cm² |
Модуль упругости, кгс/см² Modulus of elasticity, kgf/cm² |
|
|
Нативная фасция Native fascia |
3,04±0,35 |
5,83±0,61 |
|
Рубцовая фасция* Scar fascia* |
1,31±0,12 |
2,01±0,32 |
|
Фасция с каркасной нитью Fascia with a skeleton thread |
6,86±0,40 |
8,21±0,54 |
Примечание: * — изменённая задняя стенка фасциального футляра
прямой мышцы живота грыженосителей (МI, RII, WIV),
р < 0,05 при сравнении исследуемых групп.
Note: * — modified posterior wall of the fascial sheath
of the rectus abdominis of herniators (МI, RII, WIV),
p < 0.05 when comparing the studied groups.
The comparative analysis of the test results showed an increase in the biomechanical parameters of the core suture-reinforced specimens. The tensile strength exceeded that of the fascial scars and native fascias by 59.4% and 22.6%, respectively. The specimens reinforced according to the original method had a higher elasticity modulus than the fascial scars and native fascias by 40.2% and 14.1%, respectively.
In 2018–2022, the Surgery Department of the Rostov-on-Don Regional Clinical Hospital performed hernia repair procedures on 63 patients with median ventral incisional hernias using the original method. The study included 18 (28.6%) males and 45 (71.4%) females with a mean age of 63 years (P25 51; P75 73). Of these, 19 (30.2%) were normosthenic, and 44 (69.8%) were hypersthenic.
The mean duration of the disease was 22.6 months (P25 1.8; P75 44.3), as shown in Table 2.
Thirty-four patients (54.0%) were diagnosed with the first recurrence, while 29 patients (46.0%) had ≥ second hernia recurrence. The average number of recurrences among all patients was 1.31 (95% CI 1.10 to 1.52). Fourteen patients (22.2%) underwent emergency repair for acute intestinal obstruction, while 49 (77.8%) had an elective procedure.
Таблица / Table 2
Распределение больных по длительности грыженосительства
Distribution of patients by duration of herniation
|
Грыженосительство (сроки) Herniation (terms) |
Абс. Abs. |
% |
|
До 6 месяцев Up to 6 months |
2 |
3,2 |
|
От 6 месяцев до 1 года From 6 months to 1 year |
17 |
27,0 |
|
От 1 года до 3 лет From 1 year to 3 years |
26 |
41,3 |
|
Свыше 3 лет Over 3 years |
18 |
28,6 |
Thirty-four patients (54.0%) had hernias classified as W2 according to the European Society of Herniology (EHS) Classification. The average size of the hernial orifice was 8.75 cm (P25 7.30; P75 10.13) for this group. The remaining 29 patients (46.0%) had EHS W3 hernias with an average size of 10.30 cm (P25 8.65; P75 11.40). Out of the 63 treated patients, 45 (71.4%) had single hernias, while 18 (28.6%) had multiple hernial defects.
The mean procedure time was 119 minutes (P25 114; P75 127), and the main stage of the surgery lasted for 20 minutes (P25 18; P75 22).
Five patients (7.9%) had a fever for 1 day postoperatively. The same number of patients experienced postoperative intestinal paresis for 5–6 days. Two cases (3.2%) of 2 or 3-day oliguria were also reported. Most patients (30 [ 47.6%]) experienced moderate postoperative pain. Twenty-three patients (36.5%) and 9 patients (14.3%) reported severe or mild pain, respectively. There was one case of extremely severe postoperative pain for 8 days treated with opioid analgesics. Nine patients (14.3%) had surgical site infiltration lasting for 4–12 days. All postoperative wounds healed by primary intention. In most cases, the surgical sutures were removed 14 days after the procedure (P25 13; P75 16).
The early postoperative laboratory tests showed no statistically significant abnormalities for most hematology, coagulation, and blood chemistry parameters. However, lower RBC (4.23±0.59×10⁹/L; p <0.001) and hemoglobin (125.84±11.86 g/L; p=0.040), and elevated WBC (8.12±4.15×10¹²/L; p<0.001) and ESR (25.67±14.18 mm/h; p <0.001) were reported.
All patients were discharged in satisfactory condition, and no deaths occurred. The mean duration of hospitalization was 15 days (P25 12; P75 17). The study patients did not experience any recurrences during the long-term follow-up. However, two patients developed suture sinuses within one to two years after the surgical treatment.
Discussion
The authors of this study have developed, patented, and tested a surgical technique for patients with median ventral incisional hernia with musculofascial scars having a low ability to resist an increased intra-abdominal pressure gradient after hernial repair. This technique aims to prevent mesh suture eruptions and reinforce the anterior abdominal wall tissue at the site of the hernial orifice using a core suture.
The comparative analysis of anatomical experimental data shows that the biomechanical parameters of the median structures reinforced with core sutures according to the original method increased by 59.4% for fascial tensile strength and 40.2% for elasticity modulus, compared to the scar fascia in herniated patients. Based on the obtained results, the technique appears to reliably prevent herniation recurrence.
This suggestion has been confirmed since the technique was introduced into clinical practice. Over the 1 to 5-year long-term follow-up, none of the 63 patients experienced a recurrence of herniation. During the early postoperative period, no significant complications were associated with the repair technique used. The accessibility of the method, both in terms of material and financial resources, is noteworthy. Additionally, the method does not require complex technical manipulations that could prolong the duration of the hernial repair procedure.
Thus, the original technique is an effective, affordable, and safe method for the surgical management of patients with median ventral incisional hernias.
Conclusions
The selection of the optimal hernial repair technique is crucial for achieving favorable outcomes in the treatment of any ventral incisional hernia. Median ventral incisional hernias are characterized by scar tissues at the site of the hernial orifice that have a reduced ability to resist intra-abdominal pressure, which increases in the postoperative period. The repair procedure, which includes core suture reinforcement of the mesh-fixing sutures according to the original technique, ensures an increase in the biomechanical parameters of fascial aponeurotic scars.
The surgical technique proposed for recurrent ventral incisional hernia may be widely recommended for clinical practice due to its effectiveness in preventing recurrence, accessibility, and simplicity.
1. Grigoryan, RA. (2006) Abdominal Surgery: 2 Vols. Volume 1. Meditsinskoe Informatsionnoe Agentstvo, Moscow.
2. Ivanova, T.E., Zhidkov S.A. (2007) Abdominal incisional hernias: method. Guidelines. Belarusian State Medical University, Minsk.
3. Russian Patent No. 2271740, A61B 5/103 (2006.01), Surgical Technique for Revision of Fasciad and Tissue Planes: No. 2004115696: Application filed on May 25, 2004; patent published on March 20, 2006 / Tatianchenko V.K., Sarkisyan V.A., Andreev E.V., Chubaryan K.A.; Applicants: Tatianchenko V.K., Sarkisyan V.A., Andreev E.V., Chubaryan K.A. – 4 p. – Text: hard copy.
4. Russian Patent No. 2685682, A61B 17/00 (2019.02), Method of Surgical Management of Postoperative and Recurrent Ventral Hernia: No. 2018116827: Application filed on May 04, 2018; patent published on April 22, 2019 / Korobka V.L., Korobka A.V., Dabliz R.O., Danilchuk O.Ya., Shapovalov A.M.; Applicant: Korobka V.L. – 14 p., figs. – Text: hard copy.
References
1. Popov AYu, Petrovsky AN, Gubish AV, Vagin IV, Shevchenko MS, et al. Results of anterior abdominal wall repair with mesh implants in patients with postoperative ventral hernia. Pirogov Russian Journal of Surgery = Khirurgiya. Zurnal im. N.I. Pirogova. 2020;(3):35-42. (In Russ.) https://doi.org/10.17116/hirurgia202003135
2. Parker SG, Wood CPJ, Butterworth JW, Boulton RW, Plumb AAO, et al. A systematic methodological review of reported perioperative variables, postoperative outcomes and hernia recurrence from randomised controlled trials of elective ventral hernia repair: clear definitions and standardised datasets are needed. Hernia. 2018;22(2):215-226. https://doi.org/10.1007/s10029-017-1718-4
3. Ermolov AS, Blagovestnov DA, Alekseev AK, Upyrev AV, Yartsev PA, et al. Optimized approach to the surgical treatment of patients with large and giant postoperative ventral hernia. Pirogov Russian Journal of Surgery = Khirurgiya. Zurnal im. N.I. Pirogova. 2019;(9):38-43. (In Russ.) https://doi.org/10.17116/hirurgia201909138
4. Fedoseev AV, Rybachkov VV, Trushin SN, Lebedev SN, Inyutin AS. Preventive abdominal wall repair in high-risk groups of postoperative ventral hernia. Pirogov Russian Journal of Surgery = Khirurgiya. Zurnal im. N.I. Pirogova. 2019;(1):32-36. (In Russ.) https://doi.org/10.17116/hirurgia201901132
5. Bueno-Lledó J, Torregrosa-Gallud A, Sala-Hernandez A, Carbonell-Tatay F, Pastor PG, et al. Predictors of mesh infection and explantation after abdominal wall hernia repair. Am J Surg. 2017;213(1):50-57. https://doi.org/10.1016/j.amjsurg.2016.03.007
6. Chandra R, Jacobson RA, Poirier J, Millikan K, Robinson E, Siparsky N. Successful non-operative management of intraabdominal hypertension and abdominal compartment syndrome after complex ventral hernia repair: a case series. Am J Surg. 2018;216(4):819-823. https://doi.org/10.1016/j.amjsurg.2018.07.063
7. Pawlak M, Tulloh B, de Beaux A. Current trends in hernia surgery in NHS England. Ann R Coll Surg Engl. 2020;102(1):25-27. https://doi.org/10.1308/rcsann.2019.0118
8. Dietz UA, Menzel S, Lock J, Wiegering A. The Treatment of Incisional Hernia. Dtsch Arztebl Int. 2018;115(3):31-37. Erratum in: Dtsch Arztebl Int. 2018;115(6):98. https://doi.org/10.3238/arztebl.2018.0031
9. Korobka V.L., Dabliz R.O., Shapovalov A.M., Tatyanchenko V.K., Tolstopyatov S.V. Experimental substantiation of the original hernioplasty technique forrecurrent ventral hernias of median localization. Moscow Surgical Journal. 2022;(4):49-60. (In Russ.) https://doi.org/10.17238/2072-3180-2022-4-49-60
About the Authors
V. L. KorobkaРоссия
Vyacheslav L. Korobka, Dr. Sci. (Med.), Associate Professor, Head of the Department of Reconstructive, Cardiovascular, Thoracic, Maxillofacial Surgery and Transplantology; Surgeon
Rostov-on-Don
V. K. Tatyanchenko
Россия
Vladimir K. Tatyanchenko, Dr. Sci. (Med.), Professor, Head of the Department of Operative Surgery and Clinical Anatomy and Pathological Anatomy of the FPK and PPS
Rostov-on-Don
R. O. Dabliz
Россия
Rashad O. Doubliz, Surgeon
Rostov-on-Don
S. V. Tolstopyatov
Sergey V. Tolstopyatov, Cand. Sci. (Med.), Surgeon, Assistant of the Department of Reconstructive, Cardiovascular, Thoracic, Maxillofacial Surgery and Transplantology
Rostov-on-Don
M. V. Gonchar
Россия
Mikhail V. Gonchar, Assistant of the of the Department of Reconstructive, Cardiovascular, Thoracic, Maxillofacial Surgery and Transplantology; Surgeon
Rostov-on-Don
I. S. Kletz
Ivan S. Kletz, Assistant of the of the Department of Reconstructive, Cardiovascular, Thoracic, Maxillofacial Surgery and Transplantology; Surgeon
Rostov-on-Don
Review
For citations:
Korobka V.L., Tatyanchenko V.K., Dabliz R.O., Tolstopyatov S.V., Gonchar M.V., Kletz I.S. Clinical and experimental parallels in the substantiation of the method of hernioplasty of postoperative ventral hernias of median localization. Medical Herald of the South of Russia. 2024;15(1):108-114. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-1-108-114
JATS XML







































