Scroll to:
Primary signs of pituitary macroadenomas of diff erent hormonal activity and specialists to whom patients referred at the fi rst time
https://doi.org/10.21886/2219-8075-2022-13-1-65-71
Abstract
Purpose: evaluate the fi rst complaints of patients with pituitary macroadenomas, as well as the specialization of doctors, to whom they referred at the fi rst time.
Material and methods: data of medical records of 343 patients with pituitary macroadenomas (at least one tumor size >10 mm) were analyzed: non-functioning pituitary adenomas (NFPA, n=143), prolactinomas (n=67), somatotropinomas (n =133). Patients were examined prior to any treatment.
Results: In total, the most common fi rst complaints of patients with pituitary macroadenomas were: headache - 137/343 (40%), visual impairment - 86/343 (25%), general weakness and fatigue - 69/343 (20.1%), in female patients of reproductive age - menstrual irregularities. Headache did not depend on tumor size and volume, while visual disturbances were more common in patients with larger tumor volume and MR signs of chiasm compression. Th e most oft en patients with pituitary macroadenomas referred to: a neurologist 91/343 (26.5%), an ophtalmologist 44/343 (12.8%), 44/265 (16.6%) a gynecologist and a general practitioner – according to 41/343 (12%).
Conclusions: A neurologist, ophthalmologist, gynecologist, and general practitioner should be aware of a pituitary macroadenoma in patients with headaches, visual disturbances, menstrual disorders (in women of reproductive age) and non-specific general complaints that may be a marker of the presence of a pituitary tumor macroadenoma.
Keywords
For citations:
Krivosheeva Y.G., Ilovayskaya I.A. Primary signs of pituitary macroadenomas of diff erent hormonal activity and specialists to whom patients referred at the fi rst time. Medical Herald of the South of Russia. 2022;13(1):65-71. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-1-65-71
Introduction
Pituitary macroadenomas manifest various symptoms because of the compression of surrounding structures of the brain, including the pituitary gland stalk and chiasm, and hormonal dysfunction of the anterior pituitary [1][2]. This can lead to the development of numerous complications associated with progressing disability, shortening of life expectancy, and increased lethality risk in comparison with the general population [2–4].
During the past years, researchers focused on the early diagnostics of pituitary tumors to shorten the period from the appearance of first symptoms to the final diagnosis. For example, in patients with acromegaly, this parameter varies from 5 to 14 years, according to some studies [6][7]. Patients experience the active stage of the disease for too long, and by the time of diagnosis, they accumulate a wide spectrum of comorbid diseases that complicate the patient’s condition management [3][5][8]. A recent comparative two-center study on the examination of patients with acromegaly showed significant variability in the description of complaints and symptoms (> 20%). These differences did not depend on the elevation of somatotropin levels and/or insulin-like growth factor 1 (IGF-1) [9]. This indicates a need for additional studies on the evaluation of primary complaints and medical specialists who patients refer to for medical help.
The study aimed to evaluate the primary complaints of patients with pituitary macroadenomas and primary specialists the patients referred to for medical help.
Materials and Methods
Medical data and records of 343 patients with pituitary macroadenomas (at least one tumor with a size of >10 mm) with different hormonal activities were analyzed: non-functioning pituitary adenomas (NFPAs, n=143), prolactinomas (n=67), and somatotropinomas (n =133). Patients were examined prior to any treatment.
NFPAs were revealed in patients with normal IGF-1 levels and elevated prolactin levels (less than two-fold upper threshold reference values) and functioning adenomas were diagnosed in patients who had clinical symptoms and hormonal impairments. Diagnostic criteria for somatotropinoma included a significant elevation of IGF-1 and a lack of STH inhibition of less than 1 ng/ml during the glucose tolerance test. Diagnostic criteria for prolactinoma included a significant elevation of prolactin levels (over four-fold upper threshold reference values.
The criteria for study entry included pituitary tumors with at least one tumor with a size of >10 mm, diagnosed somatotropinoma, prolactinoma, or NFPA after the examination and tests for hormonal status.
The criteria of study exclusion included the lack of cortisol levels inhibition during a low-dose dexamethasone suppression test (cortisol level > 50 nmol/l), and the impossibility of differential diagnostics between NFPA with hyperprolactinemia and prolactinoma.
The characteristics of patients included in the study are presented in Table 1.
The characteristics of macroadenoma sizes are presented in Table 2.
Таблица / Table 1
Характеристика пациентов с макроаденомами гипофиза различной гормональной активности
Characteristics of patients with pituitary macroadenomas with different hormonal activity
|
Группы Groups
Характеристики Characteristics |
Гормонально неактивные аденомы гипофиза (ГНАГ) Non-functioning pituitary adenomas (NFPA) n=143 |
Пролактиномы Prolactinomas n=67 |
Соматотропиномы Somatotropinomas n=133 |
|
Возраст пациентов (годы) Patietns’ age (years) Ме [ 25;75] |
63,5 [ 54;71,3] |
49,5 [ 41;64,8] |
60 [ 48; 69] |
|
Соотношение женщин/мужчин Rate Female/Male (%) |
69,9 / 30,1 |
67,2 / 32,8 |
79,5 / 20,5 |
Таблица / Table 2
Характеристика размеров макроаденом гипофиза различной гормональной активности
Characteristics of pituitary macroadenomas of different hormonal activity
|
Параметр Parameters |
ГНАГ NFPA n=143
|
ПРЛ Prolactinomas n=67 |
СТГ Somatotropinomas n=133 |
р |
|
Сагиттальный размер (мм) Sagittal size (mm) |
20 [ 16; 28] |
21 [ 15; 30,5] |
18 [ 14; 23] |
0,022 |
|
Вертикальный размер (мм) Vertical size (mm) |
22 [ 15; 27,5] |
20 [ 14,5; 24,5] |
17 [ 12; 22] |
0,001 |
|
Фронтальный размер (мм) Frontal size (mm) |
23[ 16,5; 28] |
21 [ 15,5; 30] |
18 [ 13,5; 22] |
0,005 |
|
Объём опухоли (мм3) Tumor volume (mm3) |
5417 [ 2213; 11 916] |
5365 [ 1482; 10 566] |
2803 [ 1231; 4723] |
0,001 |
Brain and pituitary magnetic resonance imaging (MRI) was performed with a high-field MRI scanner Intera Achieva (PHILIPS) in a mode of high magnetic field intensity 3.0 T with intravenous injection of extracellular gadolinium contrast agent (Gd-CA). The authors evaluated a linear size in the vertical, sagittal (anterior-posterior), and frontal (transversal) planes; the unit of measurement was the millimeter. The tumor volume was estimated by the formula ABC*π*4/3, where ABC are semi-axis dimensions (sagittal, vertical, and frontal) of the tumor. Besides, the rate and character of the tumor spread beyond the Turkish saddle were described.
The patients were examined by an ophthalmologist. The ocular fundus was checked with an ophthalmoscope (HeineBeta 200), the perimetrium was checked with a perimeter (OculusCenterfieldplus No. SN 0801 8960). Signs of chiasmatic syndrome included three clinical signs: optic nerve atrophy, narrowing of fields of vision, and visual impairment.
The study was performed and described in the dissertation “Hormonal disturbances in patients with pituitary macroadenomas”. It was approved by an independent ethical committee No. 1 dated January 22, 2015. All patients signed a form of informed consent for participation in the study.
Statistical analysis was performed in the software Statistica 13.2 (Dellinc., USA). The normality of distribution of quantitative variables was checked using the Shapiro-Wilk test. The normality of the distribution and dispersion tests were not used to study the variables. For this reason, tests for non-parametric data were used. Medians and quartiles were calculated for quantitative variables. A comparison of three groups was made with the Kruskal-Wallis test with further posttest analysis adjusted for multiple comparisons. The analysis of qualitative data was performed with a precise Bonferroni-adjusted Fisher’s test for multiple paired comparisons.
Results
Complaints of patients with pituitary macroadenomas of various hormone functional activities are presented in Fig. 1.
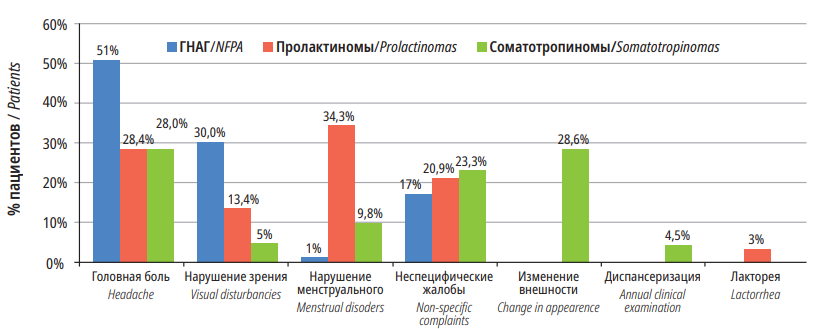
Figure 1. Первичные жалобы пациентов с макроаденомами гипофиза различной гормональной активности.
In general, patients with pituitary macroadenoma often complained about headache (137/343 (40%)), visual impairments (86/343 (25%)), general weakness and fatigue that were combined into a group “non-specific complaints” 69/343 (20.1%). Complaints were classified depending on the tumor type. In the NFPA group, headaches prevailed among complaints. In the prolactinomas group, menstrual irregularities prevailed. In the somatotropinomas group, acromegaly prevailed. Besides, only in patients with somatotropinomas, the pathology was revealed during the annual medical examination.
Considering the fact that the most often complaints were headache and visual impairment, the authors performed a comparative analysis of certain clinical-morphological parameters in patients with pituitary macroadenoma depending on the presence or lack of these symptoms (Tables 3–4).
Таблица / Table 3
Характеристики макроаденом гипофиза различной гормональной активности в зависимости от наличия/отсутствия головной боли
Characteristics of pituitary macroadenomas of different hormonal activity in subgroups with and without headache
|
Показатель Parameter |
Головная боль есть Headache YES (n=137)
|
Головная боль нет Headache NO (n=204) |
Значение Р |
|
Соотношение ж/м (%) Rate F/M (%) |
64,2/35,8 |
77,5/22,5 |
0,008 |
|
Возраст постановки диагноза Age at diagnosis (years) |
53 [ 37,5; 61,5] |
51 [ 38,3; 60,8] |
0,654 |
|
Сагиттальный размер (мм) Sagittal size (мм) |
18,2 [ 15,3; 27,5] |
19,7 [ 14; 26,8] |
0,690 |
|
Вертикальный размер (мм) Vertical size (mm) |
20 [ 14; 25,5] |
19 [ 13,2; 26] |
0,750 |
|
Фронтальный размер (мм) Frontal size (mm) |
20 [ 15; 24,5] |
20 [ 14; 26] |
0,603 |
|
Объём (мм3) Tumor volume (mm3) |
3567 [ 1578,2; 7719] |
3697 [ 1296,8; 8094,3] |
0,804 |
|
Компрессия хиазмы (%) MR-sign of chiasma compression (%) |
39,7 |
37,3 |
0,664 |
|
Хиазмальный синдром (%) Chiasmal syndrome (%) |
31,1 |
31,6 |
0,929 |
Таблица / Table 4
Характеристики макроаденом гипофиза различной гормональной активности в зависимости от наличия/отсутствия нарушений зрения
Characteristics of pituitary macroadenomas of different hormonal activity depending on the presence/absence of visual impairment
|
Показатель Parameter |
Нарушение зрения Есть Visual impairment YES (n=80) |
Нарушение зрения Нет Visual impairment NO (n=262) |
Значение Р |
|
Соотношение ж/м (%) Rate F/M (%) |
61,3/38,8 |
75,2/24,8 |
0,015 |
|
Возраст постановки диагноза Age at diagnosis (years) |
55 [ 41; 61] |
51 [ 35; 61] |
0,323 |
|
Сагиттальный размер (мм) Sagittal size (мм) |
25 [ 19,6; 31] |
18 [ 14; 23,5] |
0,001 |
|
Вертикальный размер (мм) Vertical size (mm) |
25 [ 18,6; 32] |
18 [ 13; 24] |
0,001 |
|
Фронтальный размер (мм) Frontal size (mm) |
25 [ 20; 35] |
18 [ 14; 23] |
0,001 |
|
Объём (мм3) Tumor volume (mm3) |
7793,8 [ 3982,5; 18 527,3] |
2911,5 [ 1248,0; 5939,8] |
0,001 |
|
Компрессия хиазмы (%) MR-sign of chiasma compression (%) |
68,8 |
28,6 |
0,001 |
|
Хиазмальный синдром (%) Chiasmal syndrome (%) |
66,2 |
20,9 |
0,001 |
Headache did not depend on the size and volume of the tumor. However, it was observed more often in men.
The evaluation of the presence/lack of visual impairments in the NFPA group showed that the tumor sizes were significantly larger in the group of patients that complained about visual impairments. In patients with complaints about visual impairments, signs of chiasma compression and chiasmic syndrome were observed more often than in patients without visual impairments. It should be noted that, in the group of patients with prolactinomas, complaints about visual impairments were primarily observed in men. In the group of prolactinomas, there were no significant differences in tumor sizes. However, chiasma compression was met more often in the group of patients with complaints about visual impairments and chiasmatic syndrome was observed significantly rarer. In the group of patients with somatotropin, there were no differences revealed in tumor sizes. However, chiasma compression was revealed more often in patients with visual impairments.
Most frequently, patients with pituitary macroadenoma referred to a neurologist 91/343 (26.5%), an ophthalmologist 44/343 (12.8%), a gynecologist 44/265 (16.6%), and a general physician 41/343 (12%).
Таблица / Table 5
Первичный специалист пациентов с макроаденомами гипофиза различной гормональной активности
The first specialist to whom patients with pituitary macroadenomas with different hormonal activity referred
|
Первичный специалист First specialist |
Распространённость/Prevalence |
||
|
ГНАГ (NFPA) n (%) |
Пролактиномы Prolactinomas n (%) |
Соматотропиномы Somatotropinomas n n (%) |
|
|
Невролог/neurologist |
56 (35,4%) |
18 (26,9%) |
17 (12,8%) |
|
Офтальмолог/ophthalmologist |
34 (21,5%) |
10 (14,9%) |
- |
|
Гинеколог/gynecologist |
- |
27 (57,4%) |
17 (14,9%) |
|
Эндокринолог/endocrinologist |
10 (6,3%) |
2 (3,0%) |
36 (27,1%) |
|
Терапевт/general practitioner |
14 (8,9%) |
3 (4,5%) |
31 (23,3%) |
|
СМП/ambulance |
5 (3,2%) |
2 (3,0%) |
1 (0,75%) |
|
Самостоятельно/on one's own |
5 (3,2%) |
1 (1,5%) |
9 (6,8%) |
|
Нейрохирург/neurosurger |
2 (1,3%) |
1 (1,5%) |
- |
|
Лор/otolaryngologist |
2 (1,3%) |
- |
3 (2,5%) |
|
Стоматолог/stomatologist |
- |
- |
1 (0,75%) |
|
Хирург- эндокринолог/Endocrine-surger |
- |
- |
1 (0,75%) |
|
Торакальный хирург/thoracic surger |
- |
- |
1 (0,75%) |
|
Уролог/urologist |
- |
1 (1,5%) |
- |
|
Травматолог/traumatologist |
- |
1 (1,5%) |
1 (0,75%) |
Discussion
The study aimed to evaluate the incidence of primary complaints in patients with pituitary macroadenoma with various functional hormonal activities. The evaluation of the primary complaints is very important in choosing the tactics of examination and any delays at this stage can elongate the time of final diagnosis. In the present study, the most frequent primary complaints from patients with pituitary tumors included headache (40%) and visual impairment (25%). In some patients, headache and visual impairments manifested or were revealed during active inquiry and examination of the patient. In general, in this cohort of patients, headache was observed in 88.3% of patients (NFPA – 86.9%, prolactinomas – 81%, somatotropinomas – 93%), visual impairments – in 75.7% of patients (NFPA – 82.6%, prolactinomas – 70.3%, somatotropinomas – 71.2%), which agreed with other research data [10][11]. Thus, most frequently, patients referred to a neurologist or an ophthalmologist. LalRehmanetall [10] evaluated the incidence rate of headache in 63 patients with primarily NFPA that included macroadenomas. The incidence rate of headache and visual impairment was 87.3% and 88.8%, respectively. The evaluation of only primary complaints why patients referred to a medical specialist showed that the incidence rate of these clinical symptoms was lower.
There were some differences revealed in the range of complaints and primary specialists in patients with pituitary tumors depending on the type of functional hormonal activity. Thus, patients with NFPA were a senior age group and complaints about reproductive impairments were not typical for them. The most frequent complaints were associated with the effects of the tumor mass. The first specialists they referred to were a neurologist and an ophthalmologist. Prolactinomas prevailed in patients of reproductive age who primarily complained of menstrual irregularities and there were fewer patients in this group who complained about headaches. Thus, patients from this subgroup primarily referred to a gynecologist. Patients with acromegaly had somatic complaints and primarily referred to a general physician and an endocrinologist. A small part of reproductive age patients with somatotropinoma also referred to a gynecologist because there were mixed pituitary macroadenomas (STH and prolactin-releasing). In such cases, patients primarily complained about menstrual irregularities.
It should be mentioned that the incidence rate of headache did not depend on the sizes and properties of the pituitary tumor, while visual impairments were observed rarer in patients with functioning pituitary adenomas than in patients with NFPAs. On the one hand, this can be explained by the fact that hormonal impairments “motivate” patients to refer to doctors before they develop neurologic and ophthalmologic impairments. On the other hand, this can be associated with the growth peculiarities of pituitary macroadenomas with different functional activities. These peculiarities were described in detail in the authors’ previous article [12]: NFPAs primarily demonstrate supracellular growth and manifest MR signs of chiasma compression. It is suggested that complaints about visual impairments in patients with somatotropinomas did not prevail because of infracellular growth direction.
Thus, patients with NFPA did not refer to a gynecologist, patients with prolactinomas did not refer to a general physician, and patients with somatotropinomas did not refer to an ophthalmologist.
Conclusion
In general, headache and visual impairments were the most frequent complaints in this cohort of patients with pituitary macroadenomas. Cephalgic syndrome and/or visual field impairments are absolute indications for pituitary-hypothalamic MRI with targeted imaging of the pituitary. Neurologists and ophthalmologists should be aware of the necessity of this study to exclude pituitary macroadenoma.
Menstrual irregularities in reproductive-age women can also be a marker of a functional pituitary tumor and gynecologists should be aware of it.
General physicians should know the main clinical signs of acromegaly for early diagnostics of somatotropinomas.
The awareness of related medical specialists of the clinical manifestations of pituitary tumors with different functional activities could contribute to the shortening of routing time for patients to further stages of diagnostics.
Timely diagnostics, a proper examination plan, and early prescription of the required hormone substitutive therapy will allow the doctors to provide correct diagnostics, choose the treatment, and avoid life-threatening complications in the management of patients with pituitary tumors.
References
1. Arafah BM, Prunty D, Ybarra J, Hlavin ML, Selman WR. Th e dominant role of increased intrasellar pressure in the pathogenesis of hypopituitarism, hyperprolactinemia, and headaches in patients with pituitary adenomas. J Clin Endocrinol Metab. 2000;85(5):1789-93. DOI: 10.1210/jcem.85.5.6611.
2. Mercado M, Melgar V, Salame L, Cuenca D. Clinically nonfunctioning pituitary adenomas: Pathogenic, diagnostic and therapeutic aspects. Endocrinol Diabetes Nutr. 2017;64(7):384395. (In English, Spanish). DOI: 10.1016/j.endinu.2017.05.009.
3. Esposito D, Ragnarsson O, Johannsson G, Olsson DS. Prolonged diagnostic delay in acromegaly is associated with increased morbidity and mortality. Eur J Endocrinol. 2020;182(6):523-531. DOI: 10.1530/EJE-20-0019
4. Tampourlou M, Fountas A, Ntali G, Karavitaki N. Mortality in patients with non-functioning pituitary adenoma. Pituitary. 2018;21(2):203-207. DOI: 10.1007/s11102-018-0863-9
5. Caron P, Brue T, Raverot G, Tabarin A, Cailleux A, et al. Signs and symptoms of acromegaly at diagnosis: the physician’s and the patient’s perspectives in the ACRO-POLIS study. Endocrine. 2019;63(1):120-129. DOI: 10.1007/s12020-018-1764-4.
6. Belaya Z.E., Golounina O.O., Rozhinskaya L.Y., Melnichenko G.A., Isakov M.А., et al. Epidemiology, clinical manifestations and efficiency of diff erent methods of treatment of acromegaly according to the United Russian Registry of Patients with Pituitary Tumors. Problems of Endocrinology. 2020;66(1):93-103. (In Russ.) DOI: 10.14341/probl10333
7. Maione L, Chanson P. National acromegaly registries. Best Pract Res Clin Endocrinol Metab. 2019;33(2):101264. DOI: 10.1016/j.beem.2019.02.001.
8. Wang K, Guo X, Yu S, Gao L, Wang Z, et al. Patient-Identifi ed Problems and Infl uences Associated With Diagnostic Delay of Acromegaly: A Nationwide Cross-Sectional Study. Front Endocrinol (Lausanne). 2021;12:704496. DOI: 10.3389/fendo.2021.704496.
9. Varlamov EV, Niculescu DA, Banskota S, Galoiu SA, Poiana C, Fleseriu M. Clinical features and complications of acromegaly at diagnosis are not all the same: data from two large referral centers. Endocr Connect. 2021;10(7):731-741. DOI: 10.1530/EC-21-0035
10. Rehman L, Rehman UL, Jabeen R, Rizvi R. Endoscopic Trans-Sphenoidal surgery; Efficacy and response in Pituitary Adenoma. Pak J Med Sci. 2018;34(2):412-417. DOI: 10.12669/pjms.342.14002.
11. Al Dahmani K, Afandi B, Elhouni A, Dinwal D, Philip J, et al. Clinical Presentation, Treatment, and Outcome of Acromegaly in the United Arab Emirates. Oman Med J. 2020;35(5):e172. DOI: 10.5001/omj.2020.114.
12. Ilovayskaya IA, Dreval’ AV, Krivosheeva YG, Astaf’eva LI, Stashuk GA. Growth particulars of pituitary macroadenomas with various hormonal activities. Almanac of Clinical Medicine. 2016;44(4):451456. DOI: 10.18786/2072-0505-2016-44-4-451-456
About the Authors
Y. G. KrivosheevaRussian Federation
Yulia G. Krivosheeva - Research Fellow of Neuroendocrine Unit, Department of Endocrinology.
Moscow
Competing Interests:
none
I. A. Ilovayskaya
Russian Federation
Irena A. Ilovayskaya - Dr. Sci. (Med.), Head of Neuroendocrine Unit, Department of Endocrinology, Professor of Endocrinology, Faculty of Postgraduate Medical Education.
Schepkin St. 61/2, Moscow, 129110
Competing Interests:
none
Review
For citations:
Krivosheeva Y.G., Ilovayskaya I.A. Primary signs of pituitary macroadenomas of diff erent hormonal activity and specialists to whom patients referred at the fi rst time. Medical Herald of the South of Russia. 2022;13(1):65-71. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-1-65-71
JATS XML







































