Scroll to:
Serum TSH level in hospitalized patients with moderate-to-severe COVID-19
https://doi.org/10.21886/2219-8075-2022-13-1-72-79
Abstract
Objective: to measure the serum TSH level in hospitalized patients with moderate-to-severe COVID-19.
Material and methods: this was a retrospective study at Almazov National Medical Research Centre enrolled 133 hospitalized COVID-19 patients without known thyroid disorders. Clinical data, biochemical parameters (TSH, 25(OH)D, C-reactive protein, Lactate dehydrogenase and Ferritin), fi ndings of chest computed tomography (CT) imaging as well as obtained corticosteroids therapy were analyzed.
Results: the median TSH level at the 1st-2nd day of hospitalization and at the 9-10th day was 1,15 mIU/L [0, 76; 1, 8] and 1,04 mIU/L [0,7; 1,78] respectively. Th e initial level of TSH <0,4 mIU/L was found in four patients, while by the 9-10th day of hospitalization their number doubled and reached 9 (11,7%). Furthermore, by the 9-10th day of hospitalization the TSH level more than 4,5 mIU/L was detected in four patients (4,2%). Th us, 13 out of 77 patients had the serum TSH level outside the reference range by the 9-10th day of hospitalization.
Conclusions: in case of alteration in the serum TSH level it is necessary to take into account the personal history of thyroid disorders. Th e level of thyroid hormones and autoimmune markers as well as thyroid ultrasound results may be useful in clinical interpretation of thyroidal insults during and aft er COVID-19. Th e hypothalamic-pituitary-thyroid axis may also be aff ected by drugs used to treat COVID-19.
For citations:
Mikhailova A.A., Lagutina D.I., Golovatuk K.A., Karonova T.L., Andreeva A.T., Vasilieva E.Yu., Grineva E.N. Serum TSH level in hospitalized patients with moderate-to-severe COVID-19. Medical Herald of the South of Russia. 2022;13(1):72-79. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-1-72-79
Introduction
Nowadays, SARS-CoV-2 (COVID-19) infection is a serious problem for global health. COVID-19 causes significant damage to many organ systems, especially the respiratory system [1]. At the same time, SARS-CoV-2 may provoke a negative effect on the endocrine system, in particular on the hypothalamic-pituitary-thyroid axis, but the pathogenetic aspects remain unclear [2]. A number of authors describe immuno-mediated thyroid gland (thyroid gland) damage due to the development of hyperinflammatory syndrome associated with an increase in cytokine levels and the formation of the phenomena of multiple organ failure [3][4]. To date, it has not been possible to determine the presence of SARS-CoV-2 in the thyroid and pituitary gland by means of using studies concerning light microscopy, immunohistochemistry, electron microscopy, and quantitative RT-PCR [5]. However, in academic literature, there are indications of the possibility of the direct cytotoxic effect of SARS-CoV-2 on thyrocytes and thyrotrophs through interaction with the receptor apparatus: angiotensin-converting enzyme 2 (ACE-2), transmembrane protease serine-2 (TMPRSS2), integrin avß3, and neuropilin-1 [6-10].
The results of previous studies have shown that at different time intervals after a new coronavirus infection, the incidence of thyroid pathology increases, including Graves' disease, Hashimoto's thyroiditis, subacute, pain-free and postpartum thyroiditis associated with the development of both hypothyroidism and thyrotoxic syndrome [11]. There are also data in academic literature on an isolated decrease in thyroid-stimulating hormone (TSH) and low T3 syndrome (euthyroid pathology syndrome) during the outbreak of SARS-CoV in 2002 [12][13].
Taking into account the well-known role of thyroid dysfunction in worsening the course of major diseases, for example, cardiovascular pathology, the relevance of studying thyroid pathology associated with COVID-19 is beyond doubt.
The aim of this particular study was to assess the level of TSH in dynamics in patients with moderate and severe course of new coronavirus infection in the acute period of the disease.
Materials and methods
A retrospective analysis of the data obtained from the qMS medical information system on the basis of the Almazov National Medical Research Centre of the Ministry of Health of the Russian Federation (St. Petersburg) was performed. The study included patients who were on inpatient treatment for a new coronavirus infection in the period from December 2020 to February 2021. The inclusion criteria were the patient's age (18 years and older) and the diagnosis of moderate and severe COVID-19 confirmed by the polymerase chain reaction test (PCR) test. The exclusion criterion was the presence of a history of thyroid diseases. While analyzing the data, clinical data were taken into account (age, gender, body mass index, concomitant diseases, the day of illness on which hospitalization was performed and the duration of hospitalization, as well as the outcome); laboratory results (TSH level on the 1st-2nd and 9th-10th days of hospitalization, 25(OH)D, C-reactive protein (CRP), ferritin, lactate dehydrogenase (LDH) at the time of hospitalization); results of instrumental studies (volume and degree of lung damage according to the results of multislice spiral computed tomography), as well as therapy with glucocorticosteroids.
The level of TSH, CRP, and LDH was measured on an automatic biochemical analyzer Cobas C411 Roche (Switzerland), reference ranges – 0.27–4.2 mMU/l, 0–6 mg/l, 133–225 units/l, respectively. The levels of 25(OH)D and ferritin in blood serum were determined by means of an Abbott Architect c8000 analyzer (USA) using calibrators and control serums from the manufacturer; the reference range was 9.4–52.4 ng/ml and 30.00–400.00 ng/ml, respectively.
The degree of lung tissue damage was established in accordance with the temporary methodological recommendations of the Ministry of Health of the Russian Federation version 13.1 of 17.11.2021: CT-1 (minimum) – lesion volume < 25%; CT-2 (average) – lesion volume 25–50%; CT-3 (significant) – lesion volume 50–75%, CT-4 (subtotal) – lesion volume > 75%.
Statistical analysis was performed in the Jamovi program, version 1.6.23 (Jamovi project, 2021). The data are represented by the median and interquartile range (25; 75 percentiles). In order to assess the statistical significance of the differences between the two independent groups, the Mann-Whitney T-test was used, and the Wilcoxon W-test was used for paired measurements. Fisher's criterion was used for the analysis of variance, and Spearman's correlation criterion was taken for correlation analysis. In order to assess the statistical significance of the results obtained, the probability of a random error of less than 5% (p <0.05) was chosen.
Results
The study included 133 patients with a confirmed diagnosis of COVID-19 in the above-mentioned period. Among these patients, 63 were women (47.7%) and 69 were men (52.3%). The median age of women was 62 years [ 55, 69] (from 29 to 86 years); the median age of men was 58 years [ 48, 68] (from 32 to 81 years). The general characteristics of the patients included in the study are presented in Table 1.
Таблица / Table 1
Общая характеристика включенных в исследование пациентов (n=133)
Patients baseline characteristics (n=133)
|
Показатель Characteristics |
Медиана Median |
25;75 персентиль 25;75 percentile
|
|
Возраст, лет Age, years |
59 |
[ 52; 68] |
|
ИМТ, кг/м2 BMI, kg/m2 |
29,6 |
[ 25,7;32,9] |
|
Ожирение, n (%) Obesity, n (%) |
55 (41,7) |
- |
|
ГБ, n (%) AH, n (%) |
96 (72,2) |
- |
|
ИБС, n (%) IHD, n (%) |
31 (23,3) |
- |
|
СД 2 типа, n (%) DM type 2 |
43 (32,6) |
- |
|
День госпитализации от момента появления первых симптомов, день Days from symptoms onset to hospitalization, days |
8 |
[ 6;10] |
|
Койко-день, дни Bed days, days |
17 |
[ 14;22] |
|
Исход: Выписано, n (%) летальный исход, n (%) Outcome: Discharged, n (%) Fatal outcome, n (%) |
132 (99,2) 1 (0,8) |
- |
|
ТТГ (1-2 день), мМЕ/л TSH (1st-2nd day), mIU/L |
1,15 |
[ 0,760; 1,80] |
|
ТТГ (9-10 день), мМЕ/л TSH (9-10th day), mIU/L |
1,04 |
[ 0,700; 1,78] |
|
25(OH)D(исходно), нг/мл 25(OH)D (baseline), ng/mL |
17,2 |
[ 11,7; 26,6] |
|
СРБ (исходно), мг/л CRP (baseline), mg/L |
50,14 |
[ 19,27; 107,73] |
|
Ферритин (исходно), нг/мл Ferritin (baseline), ng/mL |
530,6 |
[ 237,5; 940,6] |
|
ЛДГ (исходно), Ед/л LDH (baseline), u/L |
342 |
[ 265; 493] |
|
Объем поражения легочной ткани, % CT lung involvement, % |
35 |
[ 25;45] |
|
Степень поражения легочной ткани по КТ CT lung involvement degree 0, n (%) 1, n (%) 2, n (%) 3, n (%) 4, n (%) |
7 (5,3) 29 (22) 75 (56,8) 16 (12,1) 5 (38) |
|
Примечание: ИМТ — индекс массы тела, ГБ — гипертоническая болезнь, ИБС — ишемическая болезнь сердца, СД — сахарный диабет, ТТГ — тиреотропный гормон; СРБ — С-реактивный белок; ЛДГ — лактатдегидрогеназа.
Note: BMI – body mass index, AH – arterial hypertension, IHD – ischemic heart disease, DM – diabetes mellitus, TSH – thyroid stimulating hormone, CRP – C-reactive protein, LDH – Lactate dehydrogenase
As can be seen from the presented data, the average age of patients was 59 [ 52; 68] years, the median body mass index of patients was 29.6 kg/m2 [ 25.7, 32.9] (from 18.2 and up to 48.1 kg/m2). It was found that obesity was characteristic of 55 patients (41.7%), and type 2 diabetes mellitus – for 43 (32.6%) patients. As for cardiovascular diseases, hypertension was present in 96 (72.2%) patients, and coronary heart disease – in 31 (23.3%) patients.
Additionally, the authors of this study assessed the day of illness on which hospitalization occurred, on average it was 8 days [ 6.10], and the number of bed days spent by patients on inpatient treatment was 17 days [ 14.22]. Except for one case, the hospitalization of the remaining 132 (99.2%) patients ended with discharge.
The TSH level on Days 1–2 was assessed in all 133 patients, and its median was 1.15 mme/ml [ 0.760; 1.80] (reference value – from 0.05 to 4.49 mme/ml). Comparative characteristics of patients according to the TSH level on the 1st–2nd day of hospitalization (1 point) are presented in Table 2. It was found that seven patients had TSH levels <0.4. The authors of this study did not find statistically significant differences in the studied parameters between patients with TSH levels <0.4 mcME/ml (n=7) and patients with TSH = 0.4–4.5 microns/ml (n=125).
Repeated analysis of TSH on the 9th–10th day of hospitalization (2nd point) was performed in 77 patients; its median was 1.04 mme/ml [ 0.70; 1.78] (from 0.25 to 7.14 mme/ml). The comparative characteristics of patients in accordance with the TSH level on the 9th–10th day of hospitalization (2nd point) are shown in Table 3.
Таблица / Table 2
Сравнительная характеристика пациентов в соответствии с уровнем ТТГ на 1–2-й день госпитализации (n=133)
Patients baseline characteristics depending on serum TSH level at the 1st-2nd day of hospitalization (n=133)
|
Характеристика Characteristics |
ТТГ <0,4 мМЕ/л (n=7) TSH <0,4 mIU/L (n=7)
|
ТТГ 0,4 – 4,5 мМЕ/л (n= 125) TSH 0,4 – 4,5 mIU/L (n= 125) |
Значение P P-value |
|
Возраст, лет Age, years |
64 [ 57; 68] |
59 [ 55; 70] |
0,37 |
|
ИМТ, кг/м2 BMI, kg/m2 |
26,1 [ 25,3; 29,8] |
29.7 [ 25,8; 33,1] |
0,35 |
|
Ожирение, n (%) Obesity, n (%) |
2 (28,6) |
53 (42,4) |
0,48 |
|
СД, n (%) DM type 2 |
0 (0) |
42 (33,6) |
0,065 |
|
ГБ, n (%) AH, n (%) |
4 (57,1) |
92 (73,6) |
0,37 |
|
ИБС, n (%) IHD, n (%) |
1 (14,3) |
30 (24) |
0,57 |
|
25(OH)D(исходно), нг/мл 25(OH)D (baseline), ng/mL |
26,5 [ 17,2; 29,4] |
17 [ 11,6; 26,1] |
0,27 |
|
СРБ (исходно), мг/л CRP (baseline), mg/L |
88,3 [ 56,8; 160,9] |
48.2 [ 18,8; 105,6] |
0,15 |
|
Ферритин (исходно), нг/мл Ferritin (baseline), ng/mL |
940,6 [ 530,7; 1523,8] |
513 [ 237, 4; 879, 4] |
0,17 |
|
ЛДГ (исходно), Ед/л LDH (baseline), u/L |
413 [ 341,5; 453] |
336 [ 262,8; 494, 5] |
0,58 |
|
Объем поражения легочной ткани, % CT lung involvement, % |
40 [ 29; 46,5] |
35 [ 25, 45] |
0,72 |
|
Исход: Выписано, n (%) летальный исход, n (%) Outcome: Discharged, n (%) Fatal outcome, n (%)
|
7 (100) 0 |
124 (99,2) 1 |
0,84 |
Note: BMI – body mass index, AH – arterial hypertension, IHD – ischemic heart disease, DM – diabetes mellitus, TSH – thyroid stimulating hormone, CRP – C-reactive protein, LDH – Lactate dehydrogenase
Таблица 3 / Table 3
Сравнительная характеристика пациентов в соответствии с уровнем ТТГ на 9-10 день госпитализации (n=77)
Patients dynamic characteristics depending on serum TSH level at the 9-10th day of hospitalization (n=77)
|
Характеристика Characteristics |
ТТГ <0.4 мМЕ/л (n=9) TSH <0,4 mIU/L (n=9)
|
ТТГ 0.4 – 4.5 мМЕ/л (n= 64) TSH 0,4 – 4,5 mIU/L (n= 64) |
ТТГ >4.5 мМЕ/л (n=4) TSH >4.5 mIU/L (n=4) |
Значение P P-value |
|
Возраст, лет Age, years |
59 [ 55; 68] |
61 [ 54; 70] |
57 [ 53; 62] |
0,9 |
|
ИМТ, кг/м2 BMI, kg/m2 |
28,4 [ 27; 32,7] |
30,1 [ 25,5; 33,8] |
35,4 [ 32; 38,2] |
0,17 |
|
Ожирение, n (%) Obesity, n (%) |
3 (33,3) |
32 (50) |
2 (50) |
0,62 |
|
СД, n (%) DM type 2 |
3 (33,3) |
19 (29,7) |
1 (25) |
0,95 |
|
ГБ, n (%) AH, n (%) |
8 (88,9 ) |
48 (75) |
2 (50) |
0,33 |
|
ИБС, n (%) IHD, n (%) |
4 (44,4 ) |
15 (23,4) |
0 (0 ) |
0,2 |
|
25(OH)D, нг/мл 25(OH)D, ng/mL |
13,7 [ 7,1; 29,4] |
16,8 [ 12,3; 26,1] |
24,2 [ 20,9; 26,1] |
0,57 |
|
СРБ, мг/л CRP, mg/L |
33,0 [ 5,1; 88,3] |
49,9 [ 20,9; 100] |
59, 2 [ 29; 108,3] |
0,77 |
|
Ферритин, нг/мл Ferritin, ng/mL |
634,5 [ 348,4; 1096,7] |
522,3 [ 257,5; 1183] |
536,3 [ 430,9; 618,7] |
0,63 |
|
ЛДГ, Ед/л LDH, u/L |
458 [ 323; 496] |
379 [ 288; 547] |
287 [ 250,2; 387] |
0,59 |
|
Объем поражения легочной ткани, % CT lung involvement, % |
45 [ 28; 45] |
40 [ 25, 46] |
30 [ 30, 44] |
0,73 |
|
Исход: Выписано, n (%) летальный исход, n (%) Outcome: Discharged, n (%) Fatal outcome, n (%)
|
7 (100) 0 |
124 (99.2) 1 |
124 (99.2) 0 |
0,9 |
Note: BMI – body mass index, AH – arterial hypertension, IHD – ischemic heart disease, DM – diabetes mellitus, TSH – thyroid stimulating hormone, CRP – C-reactive protein, LDH – Lactate dehydrogenase
Depending on the TSH level, the patients were divided into three groups: I – TSH was less than 0.4 mme/ml; II – TSH was 0.4–4.5 mme/ml; III – TSH was more than 4.5 mme/ml. Four patients initially had a TSH level <0.4 mme/m, and then their number doubled by the 9th–10th day of hospitalization and amounted to 9 (11.7%) people. Also, by the 9th–10th day of hospitalization, an increase in TSH of more than 4.5 microns/ml was detected in four patients (4.2%). Thus, 13 out of 77 patients on the 9th–10th day of hospitalization had deviations in TSH values. In the present study, there was no association of the outcome of hospitalization with the level of TSH on the 1st–2nd or 9th–10th day.
While assessing markers of systemic inflammation identified in the first days of hospitalization, it was noted: CRP – 50.14 mg/l [ 19.27;107.73]; ferritin – 530.6 mcg/l [ 237.5;940.6]; LDH – 342 units/l [ 265;493]. The values of markers of systemic inflammation were compared with the values of TSH on the 1st–2nd day of hospitalization; however, no statistically significant correlation was obtained (r <0.1, p >0.05).
The median volume of lung tissue lesion averaged 35% [25;45] (from 0 to 85%). Lung tissue damage according to the results of CT of the 0th degree was noted in 5.3% of patients, 1st degree — in 22%, 2nd degree – in 56.8%, 3rd degree – 12.1%, 4th degree – in 3.8%. There was no statistically significant correlation between the level of TSH on Days 1–2/9–10 and the severity of lung tissue damage (r=0.059, p=0.499); (r=–0.110, p=0.348).
Therefore, 104 patients received glucocorticoids in the form of dexamethasone, 25 patients – prednisone, 10 – methylprednisolone (some patients received different glucocorticoid preparations during hospitalization) of the 133 patients included in the study. The average TSH level on the 9th–10th day of hospitalization when prescribing dexamethasone was statistically lower than when using other drugs of the glucocorticosteroid group (p=0.001). No statistically significant differences were obtained for prednisolone and methylprednisolone (p = 0.962, p = 0.898).
Discussion
Currently, data are accumulating indicating a thyroid lesion associated with a previous infection caused by SARS-CoV-2 (COVID-19). The aim of this study was to assess the level of TSH in dynamics in patients without previously known thyroid diseases in the acute period of COVID-19.
Speaking about the time frame of the occurrence of thyroid diseases after a new coronavirus infection (Fig. 1), the literature review by Inaba et al. focuses readers' attention on the possibility of delayed (in 4–8 weeks) occurrence of thyroid diseases after confirmation of COVID-19 [11].
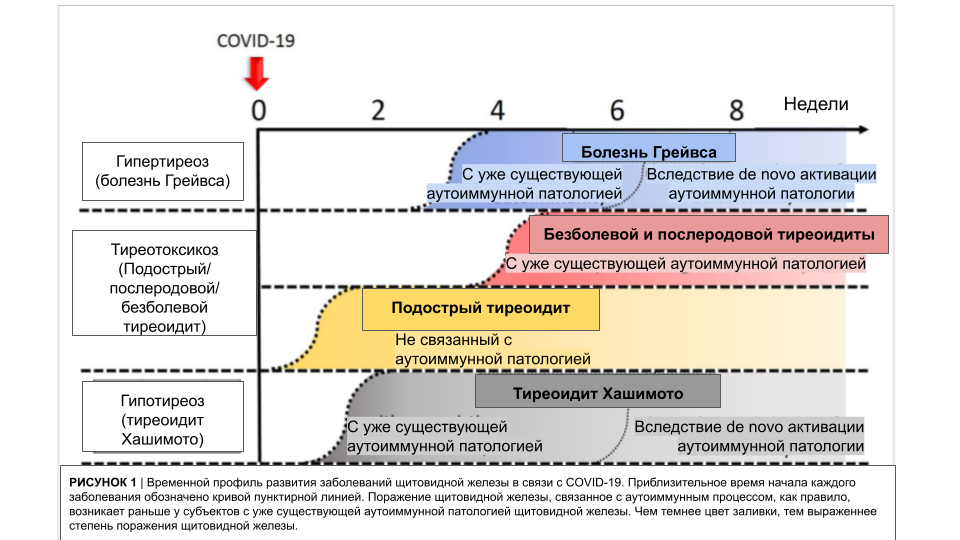
Рисунок 1. Временной профиль развития заболеваний щитовидной железы на фоне COVID-19. Адаптировано из [Inaba H, Aizawa T. Coronavirus Disease 2019 and the Thyroid - Progress and Perspectives. Front Endocrinol (Lausanne). 2021 Jun 24;12:708333. doi: 10.3389/fendo.2021.708333.]
Figure 1. Temporal profile of development of thyroid diseases in relation to COVID-19. Adapted from an article [Inaba H, Aizawa T. Coronavirus Disease 2019 and the Thyroid - Progress and Perspectives. Front Endocrinol (Lausanne). 2021 Jun 24;12:708333. doi: 10.3389/fendo.2021.708333.]
Considering the fact that patients were hospitalized on the 8th day on average from the moment of the first symptoms of the disease and were in the hospital for about 17 days, it can be assumed that the change in TSH levels detected during hospitalization in 13 patients (16.9%) is associated with the presence or development of Hashimoto's thyroiditis. However, a longer follow-up period is required to more accurately determine the function of the thyroid gland in patients who have undergone COVID-19. Also, the detected changes in TSH levels both above and below the reference range without peripheral hormone data and antibody levels do not allow talking about the primary or secondary nature of the lesion, and also to attribute these changes with confidence to the influence of COVID-19. The lack of information about the values of TSH and the state of the thyroid gland prior to hospitalization, the level of thyroid hormones, markers of autoimmune thyroid damage, as well as the results of ultrasound of the thyroid gland, are the limitation of this analysis and require a further study of the problem and long-term examination of patients in the post-COVID period.
It is important to note that the literature describes the possibility of the effect of drugs used to treat COVID-19 on thyroid function, in particular glucocorticosteroid drugs. These data are to some extent confirmed by the results obtained, which showed a lower value of the average TSH level on the 9th–10th day of hospitalization with dexamethasone compared with the value of TSH against the background of the use of other glucocorticosteroids. It is important to take into account that the use of glucocorticosteroid medicines, as well as medicines of other groups, for example, low molecular weight heparins, can lead to changes in the level of TSH and thyroid hormones1.
Conclusion
In patients with moderate and severe COVID-19 in the acute period of the disease, the TSH level can be both lower and higher than the reference. However, these changes cannot be unambiguously attributed to the influence of SARS-CoV-2 on the thyroid tissue or the hypolamo-pituitary system. In order to understand the etiopathogenesis of thyroid dysfunction, it is necessary to take into account the relevant anamnesis, conduct clarifying studies, and monitor thyroid function in the post-COVID period. For the correct interpretation of laboratory parameters, it is also important to remember the possibility of the influence of medicines used to treat COVID-19 on the hypothalamic-pituitary-thyroid axis. Additionally, the probability of delayed thyroid pathology development at the outpatient stage of treatment and rehabilitation should be taken into account.
Thus, the relevance of the problem of thyroid lesions associated with COVID-19 is beyond doubt and requires further research in this area.
1. Temporary guidelines: prevention, diagnosis and treatment of new coronavirus infection (COVID-19). Ministry of Health of the Russian Federation. Version 13.1 (17.11.2021). Access mode: https://static0.minzdrav.gov.ru/system/attachments/attaches/000/058/392/original/%D0%92%D0%9C%D0%A0-13.1-from-17-11-2021.pdf
References
1. Zhu N, Zhang D, Wang W, Li X, Yang B, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727-733. DOI: 10.1056/NEJMoa2001017.
2. Troshina E.A., Melnichenko G.A., Senyushkina E.S., Mokrysheva N.G. Adaptation of the hypothalamo-pituitary-thyroid and hypothalamo-pituitary-adrenal systems to a new infectious disease - COVID-19 in the development of COVID-19 pneumonia and/or cytokine storm. Clinical and experimental thyroidology. 2020;16(1):21-27. (In Russ.) DOI: 10.14341/ket12461
3. Huang C, Wang Y, Li X, Ren L, Zhao J, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. DOI: 10.1016/S0140-6736(20)30183-5.
4. Tee LY, Harjanto S, Rosario BH. COVID-19 complicated by Hashimoto’s thyroiditis. Singapore Med J. 2021;62(5):265. DOI: 10.11622/smedj.2020106.
5. Bradley BT, Maioli H, Johnston R, Chaudhry I, Fink SL, et al. Histopathology and ultrastructural fi ndings of fatal COVID-19 infections in Washington State: a case series. Lancet. 2020;396(10247):320-332. DOI: 10.1016/S0140-6736(20)31305-2.
6. Rotondi M, Coperchini F, Ricci G, Denegri M, Croce L, et al. Detection of SARS-COV-2 receptor ACE-2 mRNA in thyroid cells: a clue for COVID-19-related subacute thyroiditis. J Endocrinol Invest. 2021;44(5):1085-1090. DOI: 10.1007/s40618-020-01436-w.
7. Lazartigues E, Qadir MMF, Mauvais-Jarvis F. Endocrine Signifi cance of SARS-CoV-2’s Reliance on ACE2. Endocrinology. 2020;161(9):bqaa108. DOI: 10.1210/endocr/bqaa108.
8. Lam SD, Bordin N, Waman VP, Scholes HM, Ashford P, et al. SARS-CoV-2 spike protein predicted to form complexes with host receptor protein orthologues from a broad range of mammals. Sci Rep. 2020;10(1):16471. DOI: 10.1038/s41598-020-71936-5.
9. Luan J, Lu Y, Gao S, Zhang L. A potential inhibitory role for integrin in the receptor targeting of SARS-CoV-2. J Infect. 2020;81(2):318-356. DOI: 10.1016/j.jinf.2020.03.046.
10. Daly JL, Simonetti B, Klein K, Chen KE, Williamson MK, et al. Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science. 2020;370(6518):861-865. DOI: 10.1126/science.abd3072.
11. Inaba H, Aizawa T. Coronavirus Disease 2019 and the Th yroid - Progress and Perspectives. Front Endocrinol (Lausanne). 2021;12:708333. DOI: 10.3389/fendo.2021.708333.
12. Leow MK, Kwek DS, Ng AW, Ong KC, Kaw GJ, Lee LS. Hypocortisolism in survivors of severe acute respiratory syndrome (SARS). Clin Endocrinol (Oxf). 2005;63(2):197-202. DOI: 10.1111/j.1365-2265.2005.02325.x.
13. Fliers E, Bianco AC, Langouche L, Boelen A. Th yroid function in critically ill patients. Lancet Diabetes Endocrinol. 2015;3(10):81625. DOI: 10.1016/S2213-8587(15)00225-9.
About the Authors
A. A. MikhailovaRussian Federation
Arina A. Mikhailova - resident of the Department of Endocrinology, specialty «Endocrinology».
SaintPetersburg, eLibrary SPIN: 8835-5931.
Competing Interests:
Authors declares no confl ict of interest
D. I. Lagutina
Russian Federation
Daria I. Lagutina - resident of the Department of Endocrinology, specialty «Endocrinology».
Saint-Petersburg
Competing Interests:
Authors declares no confl ict of interest
K. A. Golovatuk
Russian Federation
Ksenia A. Golovatuk - doctor in endocrine department.
SaintPetersburg, eLibrary SPIN: 1199-1978
Competing Interests:
Authors declares no confl ict of interest
T. L. Karonova
Russian Federation
Tatiana L. Karonova - Dr. Sci. (Med.), Professor, chief researcher, head of Clinical Endocrinology Laboratory, professor of the Department of internal medicine.
SaintPetersburg, eLibrary SPIN: 3337-4071.
Competing Interests:
Authors declares no confl ict of interest
A. T. Andreeva
Russian Federation
Alyona T. Andreeva - junior researcher of Clinical Endocrinology Laboratory of the Institute of Endocrinology.
SaintPetersburg, eLibrary SPIN: 6051-7214
Competing Interests:
Authors declares no confl ict of interest
E. Yu Vasilieva
Russian Federation
Elena Yu. Vasilieva - Head of Central Clinical Diagnostics Laboratory.
Saint-Petersburg, eLibrary SPIN: 8546-5546
Competing Interests:
Authors declares no confl ict of interest
E. N. Grineva
Russian Federation
Elena N. Grineva - Dr. Sci. (Med.), Professor, Director of the Endocrinology Institute.
Saint-Petersburg, eLibrary SPIN: 2703-0841
Competing Interests:
Authors declares no confl ict of interest
Review
For citations:
Mikhailova A.A., Lagutina D.I., Golovatuk K.A., Karonova T.L., Andreeva A.T., Vasilieva E.Yu., Grineva E.N. Serum TSH level in hospitalized patients with moderate-to-severe COVID-19. Medical Herald of the South of Russia. 2022;13(1):72-79. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-1-72-79
JATS XML







































