Scroll to:
Endothelial Dysfunction Diagnostic “Platform” in patients with diabetes mellitus
https://doi.org/10.21886/2219-8075-2022-13-1-109-116
Abstract
Objective: to determine the diagnostic signifi cance of endothelial dysfunction (ED) laboratory markers.
Material and methods: we examined 276 men with type 2 diabetes mellitus (age 54.0[49;60] years). Patients underwent general clinical studies, analysis of carbohydrate and lipid metabolism parameters, adipohormones: leptin, resistin, adiponectin. Endothelial function was assessed by ultrasound examination of endothelium-dependent vasodilation (EDVD) of the brachial artery during a test with reactive hyperemia and determination of biochemical parameters of endothelial function — nitric oxide (NO), endothelial synthase NO type3, endothelin, ICAM-1, VCAM-1, p- and e-selectins, cadherin, PAI-1, VEGF-1, homocysteine B, C-reactive protein (CRP), osteoprotegerin. To assess the diagnostic signifi cance of the methods and to determine the cut-off , ROC analysis was used.
Results: independent signifi cance in the diagnosis of ED was demonstrated by NO, ICAM-1, resistin (p<0.001), CRP (p=0.006). Th e odds ratio of ED for resistin was 6.97, which is 1.9 times higher than NO and ICAM-1 and 3.7 times higher than CRP. Th e cut-off for diagnostic of ED are: NO — 97.3 μmol/L, ICAM-1 — 309.4 ng/ml, resistin — 6.32 ng/ml, CRP — 6.25 mg/L.
Conclusion: the diagnostic platform for determining ED, along with the ultrasound assessment of EDVD, should include the analysis of its biochemical markers: NO, ICAM-1, resistin, CRP. Resistin is an independent, high-precision marker of ED, which is the pathogenetic link between endothelial dysfunction and adipose tissue dysmetabolism.
Keywords
For citations:
Khripun I.A., Khripun A.V. Endothelial Dysfunction Diagnostic “Platform” in patients with diabetes mellitus. Medical Herald of the South of Russia. 2022;13(1):109-116. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-1-109-116
Introduction
Vascular endothelial function is a keystone in the pathogenesis of all cardiovascular lesions, inflammatory reactions, diabetes mellitus (DM), vascular thrombosis, and even the growth of malignant tumors, which makes it a common object for various studies. The issue of late diagnosis of these conditions encourages researchers to look for early diagnostic markers based on pathogenetic mechanisms of their formation [1][2]. It has been established that endothelial dysfunction (ED) is a universal starting mechanism in any vascular pathology, starting with a preclinical stage [3, 4]. However, despite the generally acknowledged significance of ED and understanding of the feasibility of its early diagnostics, a wide-scale clinical evaluation of the endothelial function is not performed because of the lack of precise criteria and unification of the diagnostic platform.
Vascular endothelium functions not only as a structural barrier, which separates the vascular walls and blood but also as a potent endocrine organ, which secrets numerous vasoactive agents, including nitrogen oxide (NO), endothelin-1, adhesion molecules, etc. [1][5]. Healthy endothelium acts as a “door keeper”, which controls the vascular homeostasis regulating instant equilibrium between the dilatation and constriction of vessels, anti-platelet and pro-platelet activity, anti-inflammatory and pro-inflammatory effect, antioxidant and pro-oxidant effect, as well as inhibition and stimulation of the vascular smooth muscle cell growth [5].
One of the conditions associated with ED is DM, which is related to systemic glucotoxicity and lipotoxicity [6]. For this reason, DM was chosen as a universal model of ED formation. Diabetes-induced ED is a critically initiating factor in the genesis of diabetic macro and microvascular complications [7]. ED pathogenesis of DM2 macrovascular complications is characterized by a reduction of bioavailability of NO, increased production of prostacyclin, endothelium-dependent hyperpolarization, as well as an enhancement of the synthesis of vasoconstrictors in the endothelium. In patients with microvascular complications of DM, ED is characterized by a reduction of NO release, and angiogenesis and endothelium regeneration impairments [7]. Some authors believe that endothelium is one of the priority targets for the prevention of the development of DM complications [5][6][7].
At the same time, it should be mentioned that most patients with DM have obesity, which provides a pathogenetic basis for the development of insulin resistance, and as a result, carbohydrate metabolism disorders. Adipose tissue, along with endothelium, is considered an endocrine organ with a potent secretory activity [8]. The substances released by the adipose tissue (adipokines) exert autocrine and paracrine effects that determine not only metabolic homeostasis but also the regulation of oxidative stress, inflammation, thrombosis, and atherogenesis, which impairs endothelial function and leads to cardiovascular diseases [9]. Along with this, there are numerous biologically active substances produced beyond endothelium that have a significant effect on its function and act as important factors for cardiovascular risk (C-reactive protein (CRP), homocysteine B, osteoprotegerin, etc.).
Many authors believe that disturbances in the secretory activity of endothelial cells are the starting mechanism of ED [10]. However, currently, the generally accepted instrumental method for ED diagnostics is the Doppler examination of flow-dependent vasodilation of the brachial arteries (BAs) [11]. On the one hand, this study is non-invasive, which is an advantage. On the other hand, it requires expensive equipment, which has low availability because of the long duration of the test. This provides a rationale for the development of available and easily-reproducible methods in clinical practice that would expand the diagnostic platform for the diagnostics of ED.
The study aimed to evaluate the diagnostic significance of laboratory markers of ED.
Materials and Methods
The authors conducted a prospective cross-sectional cohort comparative study, which included 276 men with DM2 who received oral antihyperglycemic therapy. The choice of the male sex of participants was determined by the differences in sex-dependent levels of markers of the endothelial lesion, especially in women in the period of peri- and post-menopause. The study design, forms of informed consent, and forms of primary documentation were approved by the local ethical committee of RostSMU of the Ministry of the Russian Federation No. 13/14 dated September 11, 2014. Before the study, all patients signed a form of informed consent.
The authors collected complaints, studied medical histories, and made anthropometric measurements (body weight, height, body mass index (BMI), waist circumference (WC), and hip circumference (HC)). Venous blood probes (10 ml) were taken after 12-hour fasting. Fresh blood serum was used for biochemical assays. Serum frozen at -20 °C was used for immune enzyme assays. The status of carbohydrate and lipid metabolisms was evaluated using the following parameters: fasting glucose, glycated hemoglobin (HbA1c), and lipid profile. Besides, the authors studied the content of biochemical indicators of endothelial (NO, eNOS3, endothelin, ICAM-1, VCAM-1, p- and e-selectins, cadherin, PAI-1, VEGF-1, homocysteine B, CRP, osteoprotegerin) and secretory function of the adipose tissue (leptin, resistin, adiponectin). The instrumental study included an ultrasound examination of endothelium-dependent vasodilation (EDVD) of the BA by Celermajer’s method.
Biochemical parameters of the serum were studied with the analyzer Bayer ADVIA 1650, immune enzyme assays – analyzer Zenyth 340, and HbA1c – analyzer Siemens Healthcare Diagnostics DCA 2000+. The levels of ICAM-1, VCAM-1, VEGF-1, p- and e-selectins, and cadherin were measured with Bender Medsystems GbmH kits (Austria), eNOS3 – BCM Diagnostics (USA), homocysteine B – Axis-Shield Diagnostics Ltd. (Great Britain), endothelin and osteoprotegerin – Biomedica Medizinproduckte GmbH & Co KG (Austria), CRP – Biometrica Ink (USA), leptin – Mediagnost (Germany), resistin – Biovender Labopratorni (Check Republic), adiponectin – eBioscience (Austria). The content of NO in the blood serum was calculated by the deduction of nitrites and nitrates as the products of NO metabolism according to the recommendations of the manufacturer R&D (USA). An ultrasound examination of EDVD of the BA was performed. To obtain the images and measure the diameter of the brachial artery, an ultrasonic system Philips HD 11 was used. It was equipped with a liner sensor with a phased array (frequency 7.0 MHz). EDVD BA was calculated by the formula:
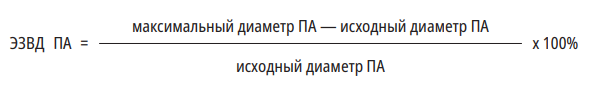
ЭЗВД ПА - EDVD BA
Максимальный диаметр ПА – Maximum DA diameter
Исходный диаметр ПА – Initial PA diameter
ED was detected based on the results of the ultrasound investigation of EDVD BA.
The statistical analysis of the obtained data was performed with the software package Statistica 10.0 (StatSoft Inc., USA). The variables were checked for normality of the distribution using the Kolmogorov-Smirnov test. The data were presented as median and interquartile range Me [Q1; Q3]. The analysis and evaluation of the associations between the quantitative features were performed with a non-parametric method of rank correlation by Spearman. To evaluate the diagnostic effectiveness of the methods and determine cut-off points, ROC analysis was used with the calculation of diagnostic sensitivity and specificity, OR, as well as ROC curves design and evaluation of the area under the ROC curve. The differences were statistically significant at p <0.05.
Results
The general characteristics of patients in the study are presented in Table 1.
Таблица / Table 1
Общая характеристика пациентов в исследовании.
General patient characteristics in the study.
|
Параметр |
Me [LQ; UQ] |
|
Возраст, лет |
54,0 [ 49; 60] |
|
Длительность сахарного диабета 2 типа, лет |
6,0 [ 2,0; 10,0] |
|
Масса тела, кг |
98 [ 90; 108] |
|
Индекс массы тела, кг/м2 |
32,1 [ 29,6; 35] |
|
Окружность талии, см |
109 [ 102; 117] |
|
Окружность бедер, см |
107 [ 102; 114] |
|
Гликемия натощак, ммоль/л |
7,9 [ 6,4; 10] |
|
HbA1c, % |
7,8 [ 6,7; 9,0] |
|
Систолическое артериальное давление, мм рт. ст. |
140 [ 130;160] |
|
Диастолическое артериальное давление, мм рт. ст. |
87 [ 80; 95] |
|
Частота сердечных сокращений, удары/минуту |
75 [ 69; 81] |
The patients’ age was 54.0 [ 49; 60] years old; the duration of DM2 was 6.0 [ 2.0; 10.0] years. Obesity was diagnosed in 116 (42%) patients, and excessive body weight – in 105 (38%) patients. The BMI median was 32.1 [ 29,6; 35] kg/m2, and WC was 109 [ 102; 117] cm. The level of fasting glycemia was 7.9 [ 6.4; 10] mmol/L, HbA1c – 7.8 [ 6.7; 9.0]%. Arterial hypertension was revealed in 190 men (68.8%). The medians of systolic and diastolic blood pressure were 140 [ 130;160] and 87 [ 80; 95] mmHg, respectively. Ischemic heart disease was diagnosed in 71 (25.7%) patients, and dyslipidemia – in 81.7% of patients. The incidence rate of ED, diagnosed by the results of an EDVD BA ultrasound examination, was 44.9%.
The correlational analysis revealed statistically significant (p <0.05) associations between EDVD BA and the levels of ED markers (CRP (r=-0.397), NO (r=0.577), ICAM-1 (r=-0.424)), and adipohormone resistin (r=-0.396), which provided grounds for a detailed study of these parameters.
The evaluation of the diagnostic significance of laboratory parameters in the verification of ED was made with ROC analysis (Table 2). High statistical significance for the verification of ED showed not only generally accepted markers of ED dysfunction (NO, ICAM-1) but also CRP, which demonstrated their independent diagnostic significance. Besides, there was a statistically significant tendency in the diagnostic significance of osteoprotegerin (p=0.07) and cadherin (p=0.06). There were no statistically significant tendencies in the diagnostic significance of eNOS3, endothelin, VCAM-1, p-selectin and e-selectin, PAI-1, VEGF, and homocysteine B.
Таблица / Table 2
Диагностическая значимость биохимических показателей для верификации и определения отношения шансов риска эндотелиальной дисфункции
Diagnostic significance of biochemical parameters for verification and determination of the odds ratio of the endothelial dysfunction risk
|
|
Cut-off |
ДЧ |
ДС |
ОШ |
ДИ ОШ |
AUC |
р |
|
NO |
<=97,28 * |
73,21 |
80,30 |
3,72 |
3,0 - 4,5 |
0,735±0,048 |
<0,001 |
|
еNOS3 |
>306,8 * |
40,00 |
75,44 |
1,63 |
1,1 - 2,4 |
0,547±0,06 |
0,437 |
|
Эндотелин |
>1,13 * |
40,91 |
50,00 |
0,82 |
0,5 - 1,3 |
0,505±0,057 |
0,937 |
|
VCAM-1 |
>508 * |
93,88 |
19,12 |
1,16 |
0,7 - 1,9 |
0,518±0,054 |
0,734 |
|
ICAM-1 |
>309,4 * |
72,58 |
80,68 |
3,76 |
3,1 - 4,5 |
0,762±0,041 |
<0,001 |
|
р-селектин |
>416,5 * |
83,67 |
30,88 |
1,21 |
0,8 - 1,8 |
0,55±0,054 |
0,352 |
|
е-селектин |
<=44,29 * |
57,14 |
58,82 |
1,39 |
1,0 - 1,9 |
0,524±0,055 |
0,667 |
|
Кадгерин |
>0,9045 * |
38,78 |
82,09 |
2,16 |
1,5 - 3,1 |
0,600±0,054 |
0,062 |
|
PAI 1 |
<=26,67 * |
13,89 |
100,0 |
1,12 |
0,6-1,7 |
0,510±0,068 |
0,885 |
|
VEGF-А |
>43,57 * |
69,39 |
50,00 |
1,39 |
1,0 - 1,9 |
0,577±0,054 |
0,151 |
|
Гомоцистеин В |
>3,568 * |
92,31 |
23,08 |
1,20 |
0,7 - 2,0 |
0,579±0,060 |
0,189 |
|
Остеопро-тегерин |
>4,69 * |
61,22 |
60,32 |
1,54 |
1,1 - 2,1 |
0,598±0,055 |
0,070 |
|
СРБ |
>6,25 * |
69,39 |
62,90 |
1,87 |
1,4 - 2,4 |
0,647±0,053 |
0,006 |
Примечание: ДИ — доверительный интервал, ДС — диагностическая специфичность, ДЧ — диагностическая чувствительность, ОШ — отношение шансов, СРБ — С-реактивный белок, AUC — площадь под ROC-кривой, Cut-off — разделительная точка, eNOS3 — эндотелиальная синтаза оксида азота 3 типа, NO — оксид азота, р — уровень значимости.
Since these molecules were not used for the diagnostic of ED independently, the authors evaluated differential cut-off values for their concentrations that corresponded to EDVD impairments during flow-dependent dilation of BA. NO plays an important role in the functioning of the endothelium. The area under the ROC curve of the ratio of sensitivity and specificity of the diagnostics of ED by the concentration of NO was 0.735±0.0048, p <0.0001. The cut-off point for NO was 97.3 µmol/L, the diagnostic significance 73.2%, and specificity 80.3%. The ED OR was 3.72 (CI 3.0-4.5).
High diagnostic significance for the verification of ED was shown by the cellular adhesion molecule 1 (ICAM-1). The area under the ROC curve of the ratio of sensitivity and specificity by the level of ICAM-1 was 0.762±0.041 (p <0.0001). The ED OR was 3.76, and the cut-off point was 309.4 ng/ml with a diagnostic sensitivity of 72.6%, and diagnostic specificity of 80.7%.
The ROC curve, which characterizes the ratio of the sensitivity and specificity of ED verification by the level of CRP in the blood serum, had the area under the curve (AUC) 0.65±0.05 (p=0.006), which indicated the acceptable test informative value. The cut-off point for CRP was 6.25 mg/L at a diagnostic sensitivity of 69.4% and specificity of 62.9%. It should be noted that the ED OR was 1.87 CI 1.4–2.4 (p=0.006).
Molecules eNOS3, endothelin, VCAM-1, p- and e-selectins, cadherin, PAI-1, VEGF-1, homocysteine B, and osteoprotegerin did not have independent significance for the diagnostics of ED.
Thus, the ED OR was the highest in the evaluation of the level of ICAM-1 (3.76, CI 3.1–4.5, p<0.0001) and NO (3.72, CI 3.0–4.5; p<0.0001) in comparison with the diagnostics by the concentration of CRP.
There is a close association between the content of hormones in the adipose tissue and ED development in patients with metabolic syndrome. Thus, for the evaluation of the independent diagnostic significance of these indicators in the verification of ED, ROC analysis was performed (Table 3). The table shows the high diagnostic significance of resistin for the verification of ED, while leptin and adiponectin were not statistically significant for ED diagnostics. Being a hormone of adipose tissue, resistin demonstrated independent significance in ED diagnostics. The diagnostic cut-off point for resistin was 6.32 ng/ml (sensitivity – 72.9%, specificity – 89.5%); the area under the ROC curve was 0.808±0.032 (p<0.0001). It should be mentioned that ED OR for resistin was 6.97 (CI 6.1–8.0), which is 1.9 higher than in NO and ICAM-1, and 3.7 times higher than in CRP. This allows the researchers to use resistin as an independent and highly sensitive marker of ED. It could be a connecting pathogenetic link between ED and adipose tissue metabolism.
Таблица / Table 3
Диагностическая значимость гормонов жировой ткани для верификации и определения отношения шансов риска эндотелиальной дисфункции
Diagnostic significance of adipose tissue hormones for verification and determination of the odds ratio of the endothelial dysfunction risk
|
|
Cut-off |
ДЧ |
ДС |
ОШ |
ДИ ОШ |
AUC |
Р |
|
Адипонектин |
>8,43 * |
22,45 |
91,04 |
2,51 |
1,5 - 4,2 |
0,544±0,054 |
0,431 |
|
Лептин |
>23,5 * |
18,37 |
91,18 |
2,08 |
1,1 - 3,8 |
0,521±0,055 |
0,708 |
|
Резистин |
>6,317 * |
72,90 |
89,53 |
6,97 |
6,1 - 8,0 |
0,808±0,032 |
<0,001 |
Discussion
Currently, the generally accepted method of ED diagnostics is an ultrasound examination of EDVD of the BA. However, this test requires equipment for ultrasonic diagnostic and lasts for 45-60 minutes, which significantly limits its application in clinical practice and encourages researchers to search for alternative diagnostic methods for ED. The spectrum of biologically active substances expressed by the endothelium and beyond its cells (that affect endothelial functioning) is quite wide and is controlled by numerous genetic factors [12][13].
One of the most important and most studied substances expressed by the endothelium is NO, which exerts a potent vasodilating, vasoprotective, antiplatelet, and anti-inflammatory effect, maintaining the tonus and non-adhesiveness of the internal vascular surface [14]. NO synthesis includes NO enzyme synthase (NOS), represented by eNOS3 at the endothelial level. The status of endothelium depends on the activity of eNOS3, the rate and amount of the synthesized NO [14][15]. One of the most important vasoconstrictor substances expressed by the endothelium (NO antagonist) is endothelin-1. An increase in its levels indicates functional stress of the endothelium and is typical for cardiovascular diseases [16]. Early signs of the endothelial lesion include increased adhesiveness of the vascular wall because of hyperproduction of serum adhesive molecules (VCAM-1, ICAM-1, e- and p-selectins, and cadherin) [16]. Enhancement of their expression on the endotheliocyte surface at the early stages of atherogenesis contributes to the adhesion of leukocytes and subendothelial penetration of lipoproteins that form an atherosclerosis plaque [17][18]. Apart from this, the function of the endothelium is evaluated by the content of biologically active molecules that damage endotheliocytes (CRP, homocysteine B, osteoprotegerin, etc.).
The studied ED biochemical markers were associated with the generally accepted EDVD parameter, which is evaluated by the results of the instrumental study. ROC analysis was performed, which revealed an independent diagnostic significance of ED markers (NO, ICAM-1, and CRP).
A large number of studies showed the association between cardiovascular risk and the levels of adipokines circulating in the blood serum (leptin, adiponectin, resistin) [9]. Thus, in patients with obesity and DM2, leptin stimulates oxidative stress, inflammation, thrombosis, and atherogenesis impairing endothelial function and being a link to cardiovascular diseases [19, 20]. At the same time, it is known that there is a decrease in the level of adiponectin in patients with visceral obesity, DM2, and an inverse dependence of its content and the number of components of the metabolic syndrome. Hypoadiponectinemia indicates not only insulin resistance, glucotoxicity, and lipotoxicity but also ED [20][21]. Another important adipohormone is resistin, which reduces glucose utilization by tissues, stimulates the production of adhesion molecules by endotheliocytes, activates endothelium, and exerts an anti-inflammatory effect, which makes it a marker of cardiovascular diseases [22][23][24].
A close association between the content of adipokines and the endothelial function provided grounds for ROC analysis for the adipose tissue hormones. A high independent diagnostic significance was established for resistin for the verification of ED. It is known that the hormone of adipose tissue resistin decreases the expression of eNOS3 and NO synthesis and enhances the expression of adhesion molecules VCAM-1 and ICAM-1 on the surface of endotheiocytes, which contributes to the aggravation of ED [24][25]. Thus, it is suggested that resistin is a factor that pathogenetically links dysfunctions of the adipose tissue and the endothelium. Earlier, it was discussed that resistin could be a factor in cardiovascular risk. However, diagnostic values of its levels, which indicate ED, were not determined [22][23]. In the present study, it was shown that adipohormone resistin not only played an important role in endothelial function but could also be an independent laboratory marker for ED diagnostics.
The authors defined diagnostic cut-off points for four biochemical markers of ED that had independent diagnostic values: NO – 97.3 µmol/L (ED OR 3.72); ICAM-1 – 309.4 ng/ml (ED OR 3.76); CRP – 6.25 mg/L (ED OR 1.87); resistin – 6.32 ng/ml (ED OR 6.97).
Laboratory evaluation of any of these markers of ED can be used in clinical practice as an alternative to ultrasound examination of EDVD of the BA. The timely application of laboratory methods expands diagnostic possibilities for the detection of ED, which is strategically important for the prevention of cardiovascular diseases.
Conclusion
Independent significance in ED diagnostics in men with DM2 was demonstrated by NO, ICAM-1, resistin, and CRP. Diagnostic cut-off points for ED were as follows: NO – 97.3 µmol/L, ICAM-1 – 309.4 ng/ml, resistin – 6.32 ng/ml, and CRP – 6.25 mg/L.
References
1. Vanhoutte PM, Shimokawa H, Feletou M, Tang EH. Endothelial dysfunction and vascular disease - a 30th anniversary update. Acta Physiol (Oxf). 2017;219(1):22-96. DOI: 10.1111/apha.12646.
2. Khripun I.A., Morgunov M.N., Vorobyov S.V., Terentiev V.P., Kogan M.I. Endothelial dysfuncton and 2 type diabetes: novel markers for earlier diagnostics. Cardiovascular Th erapy and Prevention. 2016;15(5):59-63. (In Russ.) DOI: 10.15829/1728-8800-2016-5-59-63
3. Spartalis M, Spartalis E, Athanasiou A, Paschou SA, Kontogiannis C, et al. Th e Role of the Endothelium in Premature Atherosclerosis: Molecular Mechanisms. Curr Med Chem. 2020;27(7):1041-1051. DOI: 10.2174/0929867326666190911141951.
4. Khripun I.A., Vorobyev S.V., Morgunov M.N., Kogan M.I. Endothelial function in men with type 2 diabetes without clinical signs of cardiovascular disease. Diabetes mellitus. 2016;19(5):383-387. (In Russ.) DOI: 10.14341/DM8017
5. Godo S, Shimokawa H. Endothelial Functions. Arterioscler Th romb Vasc Biol. 2017;37(9):e108-e114. DOI: 10.1161/ATVBAHA.117.309813.
6. Vecchié A, Montecucco F, Carbone F, Dallegri F, Bonaventura A. Diabetes and Vascular Disease: Is It All About Glycemia? Curr Pharm Des. 2019;25(29):3112-3127. DOI: 10.2174/13816 12825666190830181944.
7. Shi Y, Vanhoutte PM. Macro- and microvascular endothelial dysfunction in diabetes. J Diabetes. 2017;9(5):434-449. DOI: 10.1111/1753-0407.12521.
8. Matafome P, Seiça R. Function and Dysfunction of Adipose Tissue. Adv Neurobiol. 2017;19:3-31. DOI: 10.1007/978-3-319-63260-5_1.
9. Ametov A.S., Rubcov YU.E., Saluhov V.V., Khalimov Yu.Sh., Agafonov P.V. Elimination of adipose tissue dysfunction as a major factor in reducing cardiometabolic risks in obesity. Th erapy. 2019;(6):66-72. (In Russ.) DOI: 10.18565/therapy.2019.6.66-74
10. Daiber A, Steven S, Weber A, Shuvaev VV, Muzykantov VR, et al. Targeting vascular (endothelial) dysfunction. Br J Pharmacol. 2017;174(12):1591-1619. DOI: 10.1111/bph.13517.
11. Chia PY, Teo A, Yeo TW. Overview of the Assessment of Endothelial Function in Humans. Front Med (Lausanne). 2020;7:542567. DOI: 10.3389/fmed.2020.542567.
12. Khripun I. A., Vorobyev S. V., Morgunov M. N., Belousov I. I., Dzantieva E. O., et al. Th e genetic aspects of endothelial dysfunction in Patients With type 2 diabetes mellitus. Medical news of north Caucasus. 2015;10(4):339-343. (In Russ.). DOI: 10.14300/mnnc.2015.10083.
13. Khripun I.A., Vorobyev S.V., Kogan M.I. Association of the polymorphism in the androgen receptor gene and endothelial function in men with type 2 diabetes. Diabetes mellitus. 2015;18(4):35-40. (In Russ.) DOi: 10.14341/DM7622
14. Cyr AR, Huckaby LV, Shiva SS, Zuckerbraun BS. Nitric Oxide and Endothelial Dysfunction. Crit Care Clin. 2020;36(2):307321. DOI: 10.1016/j.ccc.2019.12.009.
15. Farah C, Michel LYM, Balligand JL. Nitric oxide signalling in cardiovascular health and disease. Nat Rev Cardiol. 2018;15(5):292-316. DOI: 10.1038/nrcardio.2017.224.
16. Miyauchi T, Sakai S. Endothelin and the heart in health and diseases. Peptides. 2019;111:77-88. DOI: 10.1016/j.peptides.2018.10.002.
17. Stepanova TV, Ivanov AN, Tereshkina NE, Popyhova EB, Lagutina DD. [Markers of endothelial dysfunction: pathogenetic role and diagnostic signifi cance.]. Klin Lab Diagn. 2019;64(1):34-41. DOI: 10.18821/0869-2084-2018-63-34-41.
18. Yin M, Li C, Jiang J, Le J, Luo B, уе фд. Cell adhesion molecule-mediated therapeutic strategies in atherosclerosis: From a biological basis and molecular mechanism to drug delivery nanosystems. Biochem Pharmacol. 2021;186:114471. DOI: 10.1016/j.bcp.2021.114471.
19. Katsiki N, Mikhailidis DP, Banach M. Leptin, cardiovascular diseases and type 2 diabetes mellitus. Acta Pharmacol Sin. 2018;39(7):1176-1188. DOI: 10.1038/aps.2018.40.
20. Landecho MF, Tuero C, Valentí V, Bilbao I, de la Higuera M, Frühbeck G. Relevance of Leptin and Other Adipokines in Obesity-Associated Cardiovascular Risk. Nutrients. 2019;11(11):2664. DOI: 10.3390/nu11112664.
21. Ametov A.S., Kamynina L.L., Litvinenko V.M. Th e hypoadiponectinemia as the marker of the glucotoxicity and the lipotoxicity at the patients with the type 2 diabetes mellitus and the visceral obesity. Endocrinology: News, Opinions, Education. 2018;7(2):35-45 (In Russ.). DOI: 10.24411/2304-9529-2018-12003
22. Verbovoy A.F., Tsanava I.A., Verbovaya N.I., Rudolf G.A. Resistin – a marker of cardiovascular diseases. Obesity and metabolism. 2017;14(4):5-9. (In Russ.) DOI: 10.14341/omet201745-9
23. Acquarone E, Monacelli F, Borghi R, Nencioni A, Odetti P. Resistin: A reappraisal. Mech Ageing Dev. 2019;178:46-63. DOI: 10.1016/j.mad.2019.01.004.
24. Park HK, Kwak MK, Kim HJ, Ahima RS. Linking resistin, infl ammation, and cardiometabolic diseases. Korean J Intern Med. 2017;32(2):239-247. DOI: 10.3904/kjim.2016.229.
25. Zhou L, Li JY, He PP, Yu XH, Tang CK. Resistin: Potential biomarker and therapeutic target in atherosclerosis. Clin Chim Acta. 2021;512:84-91. DOI: 10.1016/j.cca.2020.11.010.
About the Authors
I. A. KhripunRussian Federation
Irina А. Khripun - Dr. Sci. (Med.), assistant professor, department of endocrinology.
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
A. V. Khripun
Russian Federation
Alexey V. Khripun - Cand. Sci. (Med.), assistant professor, department of internal medicine #1.
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
Review
For citations:
Khripun I.A., Khripun A.V. Endothelial Dysfunction Diagnostic “Platform” in patients with diabetes mellitus. Medical Herald of the South of Russia. 2022;13(1):109-116. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-1-109-116
JATS XML







































