Scroll to:
Features of stereoisomerism of uterine contraction in pregnant women with isthmic-cervical insufficiency and its clinical significance
https://doi.org/10.21886/2219-8075-2025-16-2-21-28
Abstract
Objective: to study the features of contractile activity of the right and left sides of the uterus in patients with isthmiccervical insufficiency and uncomplicated pregnancy and to assess the nature of the gestational processes and labor outcomes depending on the sex of the fetus. Materials and Methods: a total of 146 patients with the functional form of isthmic-cervical insufficiency and 138 with uncomplicated pregnancy were examined. To study the nature of uterine activity of the right and left sides of the uterus, mechanohysterography was performed in the II and III trimesters of pregnancy. Results: in isthmic-cervical insufficiency in pregnant women with male fetuses with a higher incidence of preterm labor, bilateral uterine contractions predominated, whereas in uncomplicated pregnancy (dominated in pregnant women with female fetuses), unilateral (mainly right-sided) uterine contractions were detected. Conclusion: isthmic-cervical insufficiency is characterized by the predominance of functional symmetry in the myometrium, predominant in the case of the male fetus and leading to an increase in intraamniotic pressure and to dynamics from the length of the cervix, whereas physiological pregnancy is characterized by functional asymmetry, causing the preservation of the lower segment and the length of the cervix and more pronounced when bearing female fetuses.
Keywords
For citations:
Botasheva T.L., Keller O.V., Deriglazova O.I., Rymashevsky A.N., Lebedenko E.Yu., Ermolova N.V., Grigoryan A.K., Zavodnov O.P. Features of stereoisomerism of uterine contraction in pregnant women with isthmic-cervical insufficiency and its clinical significance. Medical Herald of the South of Russia. 2025;16(2):21-28. (In Russ.) https://doi.org/10.21886/2219-8075-2025-16-2-21-28
Introduction
Disappointing statistics on pregnancy loss indicate that the incidence of preterm birth (PTB) remains high [1–4] worldwide. Every year, 15.6 million children are born prematurely [5–12], and about one million children die from complications caused by prematurity [13][14]. One of the most common causes of PTB is isthmic-cervical insufficiency (ICI) (prevalence in the population – 3–16%), which accounts for about 30.4% of pregnancy terminations. Up to 41% of them are spontaneous abortions, and up to 32% are PTB [15][16]. The relevance of the problem is obvious from both medical-biological and social perspectives [17][18]. The pathogenesis of the functional form of ICI is based on two main mechanisms: inflammatory processes in the cervix and genetically determined connective tissue insufficiency, which trigger the processes of cervical shortening, cervical canal dilation, and increased uterine contractile activity (UCA) [19–20].
Numerous studies of UCA showed that the right and left sides of the uterus are heterogeneous in terms of UCA levels, starting from the earliest stages of pregnancy [21][22]. Since the published data indicate the heterogeneity of functional processes in the uterus during the gestation of male and female fetuses [23], it is of particular interest to study UCA depending on the sex of the fetus in uncomplicated pregnancy (UCP) and ICI complicated by PTB.
The aim of the research was to study the features of contractile activity of the right and left sides of the uterus in patients with ICI and UCP and to evaluate the nature of the gestational processes and labor outcomes depending on the sex of the fetus.
Materials and Methods
A total of 146 patients with functional ICI (Clinical group I) and 138 patients with UCP (Clinical group II) were examined. To assess the morphofunctional state of the uteroplacental complex and the sex of the fetus in the second and third trimesters of pregnancy, ultrasound examination was used (Siemens Sonoline G 50 (Germany), 3.5 MHz (registration certificate FS No. 2009/1686)). Mechanohysterography (as a component of cardiotocography) was performed using two Sonomed-200 cardiotocographs (Russia, according to the register of the medical device certification center VNIIMP TU No. 9442-042-31322051-2006) to study the nature of the contractile activity of the right and left sections of the uterus. Since the technical implementation of UCA registration in pregnant women using external mechanohystrogramming is only possible in the second and third trimesters of pregnancy, when the uterus has already grown large enough to project contractions onto the muscle layers of the anterior abdominal wall, this study was not conducted in the first trimester. Mechanohystrograms were recorded in parallel from symmetrical areas of the anterior abdominal wall of pregnant women on the right and left at the level of the umbilical ring for 20 minutes. Uterine contractions (C) were coded as absent (C0), right-sided (Cr), left-sided (Cl), and bilateral (C2). Mechanohystrograms were recorded at the same time of day (between 10 a.m. and 12 p.m.).
When processing the data, the statistical significance of the results was calculated at a confidence level of 95%. Significant differences were revealed by a posteriori analysis performed using Wilcoxon’s test with Bonferroni correction. Relative indicators (frequencies, proportions, percentages) between the groups were also compared using the chi-square test or Fisher’s exact test. Statistical data processing was performed using the Statistica version 10.01, EXCEL 2010, and IBM SPSS 24.0 software packages.
Results
A comparison of UCA indicators in patients with UCP and with ICI depending on the sex of the fetus showed that in UCP, the share of C0 was significantly higher, with this form of uterine activity predominating in pregnant women carrying male fetuses (PWCMF) in both second and third trimesters, while in women with ICI, C2 indicators were significantly higher, with a predominance of these indicators also in PWCMF pregnant women at the same stages.
In UCP, the highest number of women with no uterine activity was found in the PWCMF group (Fig. 1). Their number was significantly higher than the number of pregnant women carrying female fetuses (PWCFF) both in the second trimester (175/239 (73%) in PWCFF compared to PWCMF (151/323 (47%), p=0.0001) and in the third trimester: (86/150 (57%) in PWCMF and 97/228 (43%) in PWCFF, p=0.0078). Cr was significantly more common in female fetuses (151/323 (47%) in PWCFF compared to 54/239 (23%) in PWCMF, (p=0.0001)), both in the second and third trimesters (117/228 (51%) in PWCFF compared to 54/150 (36%) in PWCMF, p=0.0042). Left-sided uterine activity in pregnant women with male and female fetuses did not differ significantly in either the second or third trimesters (p>0.05). C2 was not recorded in pregnant women with UCP in the second and third trimesters.
On the contrary, in the case of ICI, an extremely small number of patients had a percentage of C0 (absence of UCA) and lateralized Cr and Cl forms, whereas the generalized C2 form prevailed in both PWCMF and PWCFF, with a numerical predominance of this form of uterine activity in PWCMF (Fig. 2).
In the second trimester of pregnancy, bilateral contractions were recorded significantly more often in PWCMF (137/138 (99%) compared to PWCFF (19/24 (79%), p=0.0001); Cl were recorded in only 1% of PWCMF.
In the third trimester, the titer of bilateral generalized UCA was significantly lower by 20% in PWCMF compared to PWCFF and amounted to 72% (p=0.014). The C2 level was still higher in PWCMF (137/142 (96%) compared to PWCFF 23/32 (72%) ˂0.0001). Accordingly, the number of women with left-sided UCA was higher in PWCFF (9/32 (28%) compared to PWCMF (5/142 (4%), p˂0.0001). In PWCMF, no significant differences in C2 and Cl levels were found compared to UCA levels in the second trimester (p>0.05). In PWCFF, there was a significant increase in the number of patients with left-sided UCA compared to the same form of UCA in the second trimester of pregnancy.
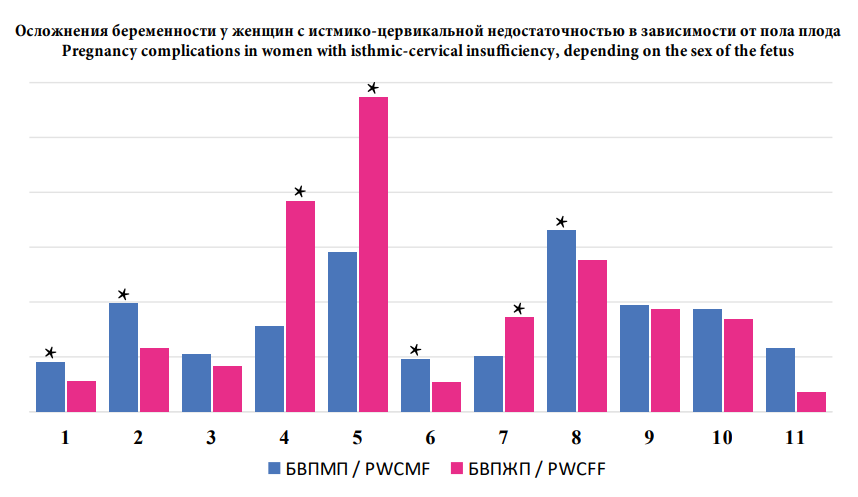
The next stage of the study involved the analysis of the occurrence rate of pregnancy complications. It was found that placental insufficiency was more common in PWCMF (567/1765 (32.1%) compared to 341/1777 (19.2%) in PWCFF p<0.0001). In women with PWCFF, gestation was more often complicated by mild anemia (494/1777 (27.8%) compared to 256/1765 (14.5%) in women with PWCMF, p<0.0001) (Fig. 3). Vaginal delivery did not differ significantly depending on the sex of the fetus (1281/1777 (72.1%) in PWCFF and 1280/1765 (72.5%) in PWCMF, p=0.7903); the rate of delivery by cesarean section did not differ significantly either in the subgroups with female and male fetuses (498/1777 (28.0%) in PWCFF and 492/1765 (27.9%) in PWCMF, p=0.9471).
Analysis of delivery dates showed that the incidence of preterm delivery in women with ICI was higher in women with PWCMF (517/1765 (29.3%) compared to 226/1777 (12.7%) in women with PWCFF, p<0.0001). In PWCFF, an immature cervix was significantly more common (316/1777 (17.8%) compared to 129/1765 (7.3%) in women with PWCMF, p˂0.0001) and labor abnormalities (300/1777 (16.9%) compared to 127/1765 (7.2%) in women with PWCMF, p˂0.0001).
The analysis of complications during the postpartum and early postpartum periods in PWCMF showed more frequent cases of placental adhesion, retention of placental tissue in the uterine cavity and postpartum hypotonic hemorrhages were observed, which led to a higher (1.6-fold) frequency of non-radical hemostasis methods. An analysis of soft tissue injuries of the birth canal revealed that postpartum PWCFF had significantly more cervical tears (279/1777 (15.7%) compared to 86/1765 (4.9%) in women with PWCMF, p˂0.0001). First and second degree perineal tears were more common in women with PWCMF (184/1765 (10.4%) compared to 52/1777 (2.9%) in PWCFF, p˂0.0001), which is apparently associated with larger fetuses in PWCMF compared to PWCFF (fetal macrosomia: 695/1765 (39.4%) in PWCMF versus 250/1777 (26.8%) in PWCFF, p˂0.0001).
The condition of newborns on the Apgar scale at birth in women with ICI, depending on the sex of the fetus, also showed lower scores (7 and below) at 1 minute after birth, mainly in male newborns (385/1765 (21.8%) vs. 167/1777 (9.4%), p˂0.0001).
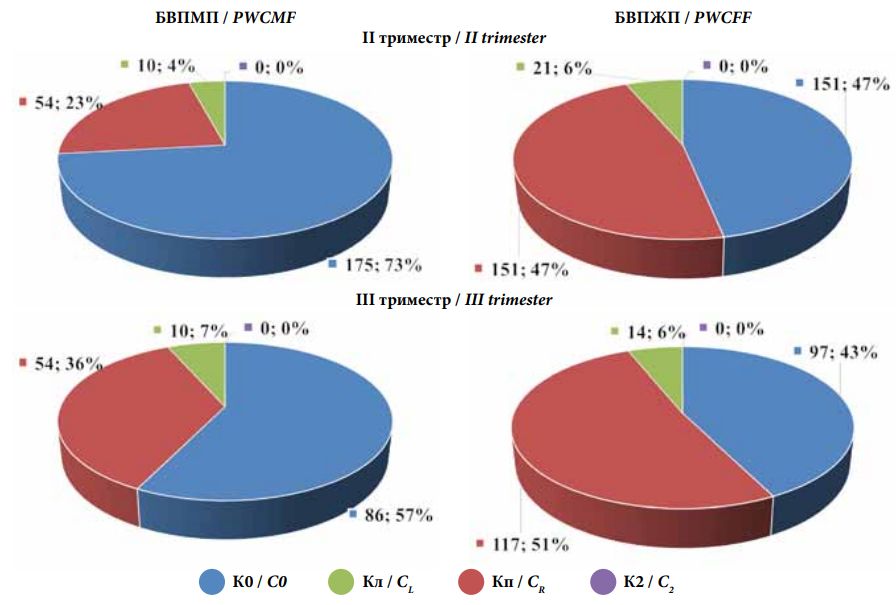
Рисунок 1. Особенности сократительной активности правых и левых отделов матки у пациенток во II–III триместрах неосложненной беременности в зависимости от пола плода.
Figure 1. Features of contractile activity of the right and left parts of the uterus in patients in the II–III trimesters of uncomplicated pregnancy, depending on the sex of the fetus.
Примечания: БВПЖП — беременные, вынашивающие плоды женского пола; БВПМП — беременные, вынашивающие плоды мужского пола; К0 — отсутствующие маточные контракции; Кп — правосторонние маточные контракции; Кл — левосторонние маточные контракции; К2 — двусторонние маточные контракции.
Notes: PWCFF — pregnant women carrying female fetuses; PWCMF — pregnant women carrying male fetuses; C0 — missing uterine contractions; CR — right-sided uterine contractions; CL — left-sided uterine contractions; C2 — bilateral uterine contractions.
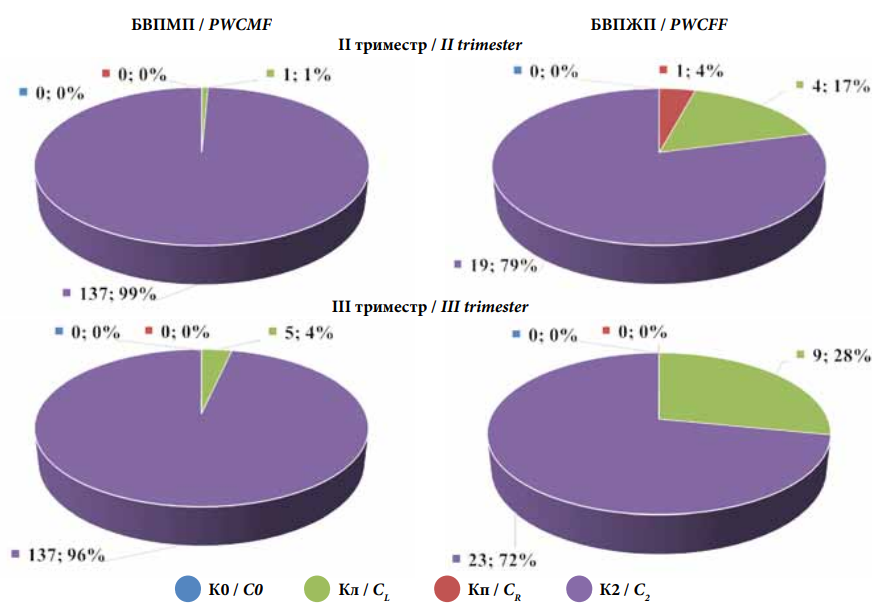
Рисунок 2. Особенности сократительной активности правых и левых отделов матки во II–III триместрах беременности у пациенток с истмико-цервикальной недостаточностью в зависимости от пола плода
Figure 2. Features of contractile activity of the right and left parts of the uterus in the II–III trimesters of pregnancy in patients with isthmic-cervical insufficiency, depending on the sex of the fetus
Примечания: БВПЖП — беременные, вынашивающие плоды женского пола; БВПМП — беременные, вынашивающие плоды мужского пола; К0 — отсутствующие маточные контракции; Кп — правосторонние маточные контракции; Кл — левосторонние маточные контракции; К2 — двусторонние маточные контракции.
Notes: PWCFF — pregnant women carrying female fetuses; PWCMF — pregnant women carrying male fetuses; C0 — missing uterine contractions; CR — right-sided uterine contractions; CL — left-sided uterine contractions; C2 — bilateral uterine contractions.
 |
|
Рисунок 3. Структура акушерских осложнений в зависимости от пола плода Figure 3. The structure of obstetric complications depending on the sex of the fetus Примечание: БВПЖП— беременные, вынашивающие плодов женского пола; БВПМП — беременные, вынашивающие плодов мужского пола; 1 — плацентарная недостаточность; 2 — истмико-цервикальная недостаточность; 3 — многоводие; 4 — маловодие; 5 — анемия беременных; 6 – преэклампсия; 7 — задержка роста плода; 8 — отёки беременных; 9 — изосенсибилизация по Rh; 10 — изосенсибилизация по АВО; 11 - предлежание плаценты. Notes: PWCFF — pregnant women carrying female fetuses; PWCMF — pregnant women carrying male fetuses; 1 — placental insufficiency; 2 — isthmic-cervical insufficiency; 3 — polyhydramnios; 4 — oligohydramnios; 5 — anemia of pregnant women; 6 — preeclampsia; 7 — fetal growth retardation; 8 — swelling of pregnant women; 9 — Rh isosensitization; 10 — ABO isosensitization; 11 — placenta previa. |
Discussion
The studies showed a higher incidence of lateralized uterine contractions and absence of UCA in women with uncomplicated pregnancies, while patients with ICI had a predominance of bilateral generalized UCA, which was more pronounced in PWCMF compared to PWCFF. The predominance of functional symmetry processes in the uterus in PWCMF is associated with the greater need for nutrients and oxygen when carrying boys. That is the reason why this subgroup has an ambilaterally located placenta more often, which uses the hemodynamic resources of both the right and left uterine arteries [21][22]. Since contractions in the smooth muscle substrate of the uterus are mediated by the degree of stretching and hypoxia [24–27], contractions are more often recorded subplacentally. In cases of ambilaterally located placenta, located simultaneously in both the right and left sections of the uterus, the highest level of bilateral generalized forms of uterine contractions is recorded [20][21]. It is C2 that, according to their biomechanism, are isometric contractions that contribute to an increase in intra-amniotic pressure and cervical dilation, while lateralized (Cr and Cl) forms of UCA are isotonic and are not accompanied by changes in intra-amniotic pressure parameters, but are a component of the uteroplacental “pump”, which contributes to the optimization of blood circulation and transplacental exchange in the uteroplacental complex.
Conclusion
The functional pairing of the uterus determines the formation of localized and generalized forms of uterine activity, the study of which allows the identification of contractile predictors of preterm birth. Normally, uterine contractions first occur in the second and third trimesters of pregnancy and are aimed at ensuring optimal blood flow and transplacental exchange in the uteroplacental complex within the uteroplacental “pump”. It is necessary to search for those forms of uterine contractions that accompany premature labor, taking into account the area of the placenta’s predominant location.
References
1. Beglov D.E., Artymuk N.V., Novikova O.N., Marochko K.V., Parfenova Ya.A. Risk factors for extremely preterm and very preterm birth. Fundamental and Clinical Medicine. 2022;7(4):8-17. (In Russ.) https://doi.org/10.23946/2500-0764-2022-7-4-8-17
2. Berghella V, Ciardulli A, Rust OA, To M, Otsuki K, et al. Cerclage for sonographic short cervix in singleton gestations without prior spontaneous preterm birth: systematic review and meta-analysis of randomized controlled trials using individual patient-level data. Ultrasound Obstet Gynecol. 2017;50(5):569-577. https://doi.org/10.1002/uog.17457
3. Tetruashvili N.K., Agadzhanova A.A. Management of single and multiple pregnancy in women with habitual abortion. Obstetrics and Gynecology: News, Opinions, Training. 2018;(2):52–57. (In Russ.) https://doi.org/10.24411/2303-9698-2018-00015
4. Matei A, Saccone G, Vogel JP, Armson AB. Primary and secondary prevention of preterm birth: a review of systematic reviews and ongoing randomized controlled trials. Eur J Obstet Gynecol Reprod Biol. 2019;236:224-239. https://doi.org/10.1016/j.ejogrb.2018.12.022
5. Radzinsky V.E., Botasheva T.L., Kotaysh G.A., eds. Fatness. Diabetes. Pregnancy. Versions and contraversions. Clinical practices. The prospects. Moscwo: GEOTAR-Media; 2020. (in Russ.)
6. Cataño Sabogal CP, Fonseca J, García-Perdomo HA. Validation of diagnostic tests for histologic chorioamnionitis: Systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2018;228:13-26. https://doi.org/10.1016/j.ejogrb.2018.05.043
7. Grabovac M, Karim JN, Isayama T, Liyanage SK, McDonald SD. What is the safest mode of birth for extremely preterm breech singleton infants who are actively resuscitated? A systematic review and meta-analyses. BJOG. 2018;125(6):652-663. https://doi.org/10.1016/j.jogc.2018.03.059
8. Alyokhina A.G., Blesmanovich A.E., Petrov Yu.I. Increasing pregnancy after the isthmic-cervical insufficiency. Synergy of Sciences. 2018;19:900−998. (in Russ.). eLIBRARY ID: 32330409 EDN: YMTELK
9. Mönckeberg M, Valdés R, Kusanovic JP, Schepeler M, Nien JK, et al. Patients with acute cervical insufficiency without intraamniotic infection/inflammation treated with cerclage have a good prognosis. J Perinat Med. 2019;47(5):500-509. https://doi.org/10.1515/jpm-2018-0388
10. Radzinsky V.E., Orazmuradov A.A., Savenkova I.V., Damirova K.F., Haddad H. Preterm labour: an open problem in XXI century. Kuban Scientific Medical Bulletin. 2020;27(4):27-37. (In Russ.) https://doi.org/10.25207/1608-6228-2020-27-4-27-37
11. Anzhoeva P.G., Shamanova A.I., Sunsheva B.A., Bairamukova A.A., Vandisheva A. P. et al. An analysis of pregnancy and labour outcomes in cervical incompetence. International Research Journal. 2024;6(144). (in Russ.) https://doi.org/10.60797/IRJ.2024.144.165
12. Quenby S, Gallos ID, Dhillon-Smith RK, Podesek M, Stephenson MD, et al. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet. 2021;397(10285):1658-1667. https://doi.org/10.1016/S0140-6736(21)00682-6
13. Dobrokhotova Yu.E., Kuznetsov P.A., Dzhokhadze L.S. Current discourse on recurrent pregnancy loss (EshRE Protocol 2023, National clinical guidelines "Recurrent Pregnancy Loss" 2021, materials of the World congress of EshRE 2023). RMJ. Mother and child. 2023;6(3):219-225. (in Russ.) https://doi.org/10.32364/2618-8430-2023-6-3-1
14. Perin J, Mulick A, Yeung D, Villavicencio F, Lopez G, et al. Global, regional, and national causes of under-5 mortality in 2000-19: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet Child Adolesc Health. 2022;6(2):106-115. Erratum in: Lancet Child Adolesc Health. 2022;6(1):e4. https://doi.org/10.1016/S2352-4642(21)00311-4.
15. Medley N, Poljak B, Mammarella S, Alfirevic Z. Clinical guidelines for prevention and management of preterm birth: a systematic review. BJOG. 2018;125(11):1361-1369. https://doi.org/10.1111/1471-0528.15173
16. FIGO Working Group on Good Clinical Practice in Maternal-Fetal Medicine. Good clinical practice advice: Prediction of preterm labor and preterm premature rupture of membranes. Int J Gynaecol Obstet. 2019;144(3):340-346. https://doi.org/10.1002/ijgo.12744
17. Gondarenko A.S., Galina T.V., Smirnova T.V., Kuznetsova O.A., Markaryan N.M., Obukang A. Scale for Assessing Risk of Extremely Preterm Birth. Doctor.ru. 2016;(7):53–56. (in Russ.) eLIBRARY ID: 26697332 EDN: WMFQYP
18. Dolgushina V.F., Alikhanova E.S., Kurnosenko I.V., Astashkina M.V., Smolnikova L.A. Immunological predictors of premature birth in isthmic-cervical insufficiency. Doctor.Ru. 2024;23(2):12–18. (in Russ.) https://doi.org/10.31550/1727-2378-2024-23-2-12-18
19. Keller O.V., Botasheva T.L., Rymashevsky A.N., Lebedenko E.Yu., Palieva N.V., et al. The role of some indicators of the antioxidant system and adipose tissue metabolism in predicting isthmic-cervical insufficiency. Medical Herald of the South of Russia. 2024;15(2):7-15. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-2-7-15
20. Kozlov L.A., Khanova A.M., Talipova R.R., Khasanova A.M., Galyaveeva A.R. Works by Professor V.S. Gruzdev and his disciples on uterine contractions (for the 150th anniversary of Professor V.S. Gruzdev). Practical Medicine. 2018;16(6):141- 150. (in Russ.) https://doi.org/10.32000/2072-1757-2018-16-6-141-150
21. Botasheva T.L., Kotieva I.M., Grigoryan A.K., Kudrin R.A., Klaucek S.V., et al. The principle of morpho-functional symmetry-asymmetry in the formation of contractile activity of the uterus during physiological and complicated pregnancy. Journal of Volgograd State Medical University. 2024;21(4):117- 124. (In Russ.) https://doi.org/10.19163/1994-9480-2024-21-4-117-124
22. Fabrikant A.D., Botasheva T.I., Rymashevsky A.N., Petrov Yu.A., Palieva N.V., et al. The fetus gender value in the structure of obstetric pathology in pregnant women with gestational diabetes mellitus. Medical Herald of the South of Russia. 2021;12(4):20-26. (In Russ.) https://doi.org/10.21886/2219-8075-2021-12-4-20-26
23. Lorente-Pozo S, Parra-Llorca A, Torres B, Torres-Cuevas I, Nuñez-Ramiro A, Cernada M, et al. Influence of Sex on Gestational Complications, Fetal-to-Neonatal Transition, and Postnatal Adaptation. Front Pediatr. 2018;6:63. https://doi.org/10.3389/fped.2018.00063
24. Bezirova L.H., Malyshkina А.I., Nazarova А.О., Loginova V.S., Nazarov S.B. Bioelectric parameters of contractile activity of the uterus in the III trimester of pregnancy. Bulletin of the Ivanovo Medical Academy. 2023;28(2):23-26.(in Russ.) eLIBRARY ID: 54893279 EDN: LAMTYS
25. Orlov R.S. Fundamentals of modern myometrial electrophysiology. Obstetrics and Gynecology. 1969;(1):3–10.(in Russ.).
26. Kovalev V.V., Tsyvyan P.B., Milyaeva N.M., Lukin O.N., Protsenko Yu.L. The degree of stretching of the myometrium is an important regulator of contractile activity of the uterus. Obstetrics and Gynecology. 2013;(2):62-67. (in Russ.). eLIBRARY ID: 18897228 EDN: PXNSUP
27. Teodorescu-Exarchu I., Dumitru I. Physiology and pathophysiology of human reproduction. Bucharest: Medical Publishing House; 1998. (In Russ.)
About the Authors
T. L. BotashevaRussian Federation
Tatyana L Botasheva, Dr. Sci. (Med.), Professor, Professor of the Chair of obstetrics and gynecology №3
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
O. V. Keller
Russian Federation
Oksana V. Keller, Deputy Chief Physician for Obstetrics and Gynecology, Research Institute of Obstetrics and Pediatrics, Head of the Gynecological Department of the Research Institute of Obstetrics and Pediatrics Rostov State Medical University, Assistant of the Department of Obstetrics and Gynecology No. 1
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
O. I. Deriglazova
Russian Federation
Olga. I. Deriglazova, doctor endocrinologist
Competing Interests:
Authors declare no conflict of interest
A. N. Rymashevsky
Russian Federation
Alexander N. Rymashevsky, Dr. Sci. (Med.), Professor, Head of the Department of Obstetrics and Gynecology No. 1
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
E. Yu. Lebedenko
Russian Federation
Elizaveta Yu. Lebedenko, Dr. Sci. (Med.), Professor of the Chair of obstetrics and gynecology №3
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
N. V. Ermolova
Russian Federation
Natalia V. Ermolova, Dr. Sci. (Med.), Professor, Professor of the Chair of obstetrics and gynecology №1
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
A. K. Grigoryan
Russian Federation
Anait K. Grigoryan, Head of the Neurological Department
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
O. P. Zavodnov
Russian Federation
Oleg P. Zavodnov, Cand. Sci. (Bio.), Researcher, Scientific Department of the NIIAP Clinic
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
Review
For citations:
Botasheva T.L., Keller O.V., Deriglazova O.I., Rymashevsky A.N., Lebedenko E.Yu., Ermolova N.V., Grigoryan A.K., Zavodnov O.P. Features of stereoisomerism of uterine contraction in pregnant women with isthmic-cervical insufficiency and its clinical significance. Medical Herald of the South of Russia. 2025;16(2):21-28. (In Russ.) https://doi.org/10.21886/2219-8075-2025-16-2-21-28







































