Scroll to:
Past and present of portal hypertension surgery (about the Rostov school of surgeons)
https://doi.org/10.21886/2219-8075-2025-16-2-128-135
Abstract
Objective: to analyze the accumulated experience of the Rostov surgical school in providing care to patients with complicated portal hypertension, to discuss and present the author's view on the facts presented. Materials and methods: the surgical clinic of Rostov State Medical University has experience in treating more than 500 patients with cirrhosis of the liver since 1993. The stages of mastering surgical interventions began with the work of N.A. Bogoraz, who moved from the University of Warsaw to Rostov-on-Don. By 2007, 79 operations of proximal splenorenal (splenotesticular) venous bypass surgery (group I) were performed, from 2007 to 2024 315 operations of transjugular intrahepatic portosystemic bypass surgery (group II). Results: analysis of intra- and postoperative complications revealed that intra-abdominal bleeding was registered in 5,06% in group I versus 0.31% in group II; varicose esophageal and gastric bleeding in the first 24 hours after surgery in 2,53% versus the absence of such a complication in group II, anemia after surgery requiring hemotransfusion in 34.17% against 0%, the development of hepatorenal syndrome in 7,59%, which led to death in group I versus 2,53% in group II. Conclusions: the Rostov Surgical School, which is one of the five centers in the Russian Federation that widely use TIPS/TIPS surgery in their arsenal, makes a definite contribution to improving the technique. But the issue of providing high-tech medical care to patients with cirrhosis of the liver remains open in its knowledge and development.
Keywords
For citations:
Sapronova N.G., Khoronko Yu.V., Balandin A.F., Malitsky N.A., Oganesian M.G., Balyasnikova D.A., Kantsurova M.R. Past and present of portal hypertension surgery (about the Rostov school of surgeons). Medical Herald of the South of Russia. 2025;16(2):128-135. (In Russ.) https://doi.org/10.21886/2219-8075-2025-16-2-128-135
Introduction
Portal hypertension (PH) is a syndrome manifested in various liver diseases, and also in conditions other than liver diseases. Increased blood pressure in the portal vein (PV) leads to a number of such manifestations as dilation of the esophagus and stomach veins, ascites, hydrothorax, etc. An increase in pressure portosystemic gradient (PSG) in complicated PH can cause a dangerous and unpredictable complication – esophagogastric varicose bleeding. Mortality at its first episode reaches 30–50%, and the frequency of recurrent bleeding in the first three years of the disease is 50–90% [1].
The main predictor of bleeding is an increase in PSG pressure. Most medical and endoscopic measures used in the treatment of PH do not restrain the increase in PSG pressure, but reduce the level of this indicator only to a small extent [2].
Surgical interventions used in the treatment of varicose esophagogastric bleeding can be divided into two groups: separation of portocaval collaterals (azygoportal separation) and portosystemic bypass interventions. These surgical interventions are able to significantly reduce PSG pressure.
The purpose of the study is an analysis of the accumulated experience of the Rostov surgical school in assisting patients with complicated PH, a discussion, and presentation of the author’s view.
In February 2024, in the Russian Federation, the 150th anniversary of Professor Nikolai Alekseevich Bogoraz, our fellow countryman, an innovative surgeon and original experimenter, was celebrated. In scientific periodicals and on the pages of the Internet, there were publications dedicated to this significant date; a documentary film was made about the events of his life. The Rostov surgical school, the road of which was opened by the work of N.A. Bogoraz “On transplantation of the superior mesenteric vein into the inferior vena cava in cirrhosis”, published in 1913 in the journal Russian Doctor [3], began its journey in 1915, when Nikolai Alekseevich, being the head of the department of hospital surgery, moved from Warsaw to Don University (now Rostov State Medical University). Proficiency in the vascular suturing technique allowed him to perform the most complex surgical interventions not only in PH but also in transplantation of endocrine organs (thyroid gland, pituitary gland). The prophetic selection of such surgery sections as reconstructive and restorative currently determines the development of PH surgery.
A.Yu. Anisimov (2022), in a monograph on the history of PH surgery development, described this event as the formation of a mesenterico-caval anastomosis (“Bogoraz’s operation”) in a patient with ascites of cirrhotic genesis, performed in 1913. The difficulties of providing the surgical guidance with adequate surgical suture material and the imperfection of the anesthesiological component did not allow it to become the preferred surgical intervention [4].
Yu.V. Khoronko et al. in 2014 published the article on portosystemic bypass surgery, which describes in detail the trends in PG surgery of the 19th, 20th, and early 21st centuries. A return to mesenteric-caval and portosystemic bypass surgery occurred in the 1970s [5]. It affected the work of Rostov Medical University surgeons. In 1973, a young surgeon and later professor, Ivan Ivanovich Katelnitsky, came to the Department of Hospital Surgery, first to the thoracic surgery department, and then to the vascular surgery department. Being a student of Professor Petr Petrovich Kovalenko, who headed the department at that time, he made it a priority to help patients with PH.
Materials and methods
From 1993 to 2024, more than 500 patients with PH syndrome were treated at the RostSMU surgical clinic. These years can be divided into two periods: before and after 2007. Before 2007, for 14 years, 77 patients with intrahepatic PH underwent proximal splenorenal venous bypass surgery (SVBS) after splenectomy, and after 2007, splenic-testicular venous bypass surgery after splenectomy, who made up observation group I. In 2007, Professor Yuri Vladilenovich Khoronko began intensive implementation of the endovascular operation of transjugular intrahepatic portosystemic shunt (TIPS) at the university hospital. During this 17-year period, 315 operations of bypass surgery were performed, which made up observation group II. The inclusion criteria in both observation groups were cirrhotic PH in the form of varicose veins of the esophagus and stomach, with the threat of hemorrhage or bleeding, as well as ascites, uncomplicated or refractory to drug therapy. Patients with compensated, sub- and decompensated hepatocellular insufficiency according to Child-Turcotte-Pugh with a score of ≥ 11 were included in the groups. The exclusion criteria were hepatic insufficiency decompensation at the sum of points ≥ 11, high-risk patients according to the MELD scale ≥ 20 points, severe hepatorenal syndrome with creatinine > 133 μmol/L or daily creatinine clearance ≥ 40 ml/min, sodium ≥ 130 mmol/L, and patients with stage III-IV encephalopathy.
The age of patients in group I was from 8 to 67 years, on average 41.50 ± 15.13 years, in group II – from 14 to 83 years, on average 51.04 ± 12.52 years (p > 0.05). In group I, there were 36/79 (45.57%) men and 43/79 (54.43%) women, in group II – 161/315 (51.11%) men and 154/315 (48.89%) women (p>0.05).
Hepatocellular insufficiency was established according to the Child-Turcotte-Pugh classification: insufficiency of class A was found in 19/79 (24.05%) patients, class B – in 48/79 (60.76%) patients, class C – in 12/79 (15.19%) patients in group I. In group II, there were no patients with hepatocellular insufficiency of class A – 0/315 (0%), insufficiency of class B was found in 191/315 (60.63%) patients, and class C – in 124/315 (39.37%) patients, respectively. Depending on the severity according to the MELD score, group I included 54/79 (68.35%) patients with a score of less than 11, from 11 to 15 points – 22/79 (27.85%), and from 16 to 20 points – 3/79 (3.80%) patients. Group II included 151/315 (47.94%) patients with less than 11 points, from 11 to 15 points – 143/315 (45.39%), and from 16 to 20 points – 21/315 (6.67%), respectively. There were no patients with more than 20 points in both groups.
The TIPS surgical operation was performed in an X-ray surgical operating room, until 2017 using a C-arc angiographic complex Siemens (Germany) Arcadis Avantic, and after 2017 using an angiographic complex General Electric.
Processing of the data obtained was carried out using descriptive statistics and the Statistica SPSS 26.0 application package.
Results
The essence of SVBS after splenectomy is as follows: after laparotomy and revision of the abdominal cavity, the spleen was mobilized, the spleen vein and artery in its gates were isolated, the artery was ligated and transected. To form an anastomosis between the spleen and renal veins, a sufficient length of the isolated section of the spleen vein is required. Therefore, the spleen vein was transected so as to preserve the vein division site at the spleen gate. After opening the retroperitoneal space, the left renal vein was visualized, on which the Satinsky clamp was applied, preserving blood flow, and a splenorenal venous anastomosis of up to 10 mm in diameter in the “end-to-side” type was formed using the “parachute” application technique (Fig. 1).
The anastomosis zone was covered with fiber and peritoneum, restoring its integrity1. A feature of this operation is a large laparotomic approach and blood loss due to the removal of the spleen. Refractory ascites and severe liver failure are relative contraindications.
The analysis of complications and the effectiveness of this surgery type was carried out. Among early postoperative complications, there were intra-abdominal bleeding, which was found in 7/79 (8.86%), accumulation of fluid in the pleural cavity and/or pericardium – in 7/79 (8,86%), subcutaneous eventeration – in 1/79 (1.26%), esophagogastric varices in the first 24 hours after surgery – in 2/79 (2.53%), anemia after surgery requiring transfusion – in 27/79 (34.17%), development of hepatorenal syndrome – in 6/79 (7.59%), which resulted in death of all 6/79 (7.59%) patients of group I and was due to the high risk of surgery, the volume of surgery and blood loss.
The objective assessment of the portal system decompression effectiveness was monitoring of the patency of portosystem anastomoses and detecting their dysfunction, since the main diagnosis of patients with intrahepatic PH remained the same after surgery. The frequency of bleeding episodes in patients of group I was 14/73 (19.18%), with the exception of those who died from 31 days to 36 months after surgery. The risk of bleeding was increased from the second year after the operation. The cause of shunt thrombosis could be technical errors in its application, hypercoagulation syndrome, a decrease in pressure in the PV, or a decrease in the speed of blood flow through the shunt.
The mortality rate of group I patients was 6/79 (7.59%) in the early postoperative period. The cause of the lethal outcome was hepatorenal syndrome.
A favorable outcome of proximal SVBS surgery is demonstrated using the clinical example of 22-year-old patient L. with viral liver cirrhosis, grade III esophageal and gastric varices (with a history of bleeding), class A hepatocellular insufficiency (4 points according to Child-Turcotte-Pugh) 7 years after surgery (Fig. 2). Analysis of the results and efficacy of the treatment established the absence of recurrent bleeding, reduction of esophageal varices, complete resorption of ascites, encephalopathy.
The essence of TIPS surgery is as follows: patients underwent mesenterico-portography by puncture of the radial artery. The superior mesenteric artery or (less commonly) the celiac trunk was catheterized. After administration of the contrast agent, an image of the PV was obtained in the venous phase. Simultaneously, the right transjugular venous access through the superior vena cava and atrial sinus catheter was passed into the inferior vena cava to the mouth of the hepatic veins. The middle or right hepatic vein was catheterized using a 5F catheter. The wall of the hepatic vein was punctured in the direction of the right branch of the PV or its bifurcation, forming a canal in the parenchyma, which was dilated by inserting a special balloon. A self-expanding hepatic-biliary PTFE-coated stent-graft up to 10 mm in diameter (Hanarostent) has been used for stenting since 2016, before which a biliary partially uncovered stent (Shim Hanarostent) was used in the clinic (Fig. 3). To increase the effectiveness of TIPS surgery, the bypass step was supplemented with embolization of the left, posterior, and (if necessary) short gastric veins with Gianturco spirals.
The peculiarity of the operation is the low surgical aggression and, as a result, good tolerance by patients with cirrhosis. This fact is especially relevant if intervention is necessary for patients with hepatic insufficiency belonging to classes B and C according to Child-Turcotte-Pugh criteria [6].
Analysis of early postoperative complications draws attention to the absence of complications associated with laparotomy, splenectomy, and suppuration of the postoperative wound. Also, no esophagogastric bleeding was observed in the first 24 hours after surgery. In the only case 1/315 (0.31%), there was intra-abdominal bleeding due to damage to the extrahepatic part of the PV during puncture, which ended in a lethal outcome, despite suturing the damaged vessel and replenishing blood loss. This complication occurred in 2007 at the initial stage of the development of this surgical intervention. In the period from 2007 to 2010, due to the technical features of TIPS surgery, 8/315 (2.53%) patients had an intraoperative complication in the form of a bile duct puncture accompanied by short-term hemobilia. In the period from 2007 to 2011, 30/315 (9.52%) patients experienced slight distal or proximal stent displacement during gastric vein embolization. Distal displacement was reported in 9/30 (30%) and proximal displacement – in 21/30 (70%) patients, respectively. The mortality rate during TIPS surgery was 8/315 (2.53%), which corresponded to the world experience in performing such interventions (0.6–2.8% with a total experience of more than 150 operations) [7].
The favorable outcome of TIPS surgery with embolization of gastric veins is demonstrated by the example of patient K., 72 years old, with cirrhosis of the liver of viral etiology, varicose veins of the esophagus and stomach of stage III (in the history of 2 episodes of bleeding, acute myocardial infarction 12 years ago), posthemorrhagic anemia, ascites, chronic hepatocellular insufficiency class C (8 points according to Child-Turcotte-Pugh), stage I hepatic encephalopathy (Fig. 4). Analysis of the results and effectiveness of the treatment 5 years after surgery established the absence of recurrent bleeding, regression of esophageal varices and ascites, and the absence of progression of hepatic failure. At the 79th year of life, patient K. died of bilateral pneumonia, which was a complication of ARVI.
Clinical criteria for assessing the results of treatment of patients during the first year after surgery in both groups was as follows: a “good” result – the absence of episodes of varicose bleeding, a decrease in the degree of dilation of esophagus and stomach veins, resorption of ascites, the absence of postoperative (p/o) encephalopathy; a “satisfactory” result – no episodes of varicose bleeding, the degree of dilation of esophagus and stomach veins remains unchanged, ascites is corrected by medication, p/o encephalopathy is corrected by medication; an “unsatisfactory” result – recurrence of varicose bleeding, a lethal outcome. Thus, “good” results in group I were obtained in 18/73 (24.66%) versus 102/307 (33.22%) in group II, “satisfactory” – in 29/73 (39.73%) in group I versus 181/307 (58.96%) in group II, and “unsatisfactory” – in 26/73 (35.61%) in group I versus 24/307 (7.82%) in group II.
It was established by a comparative assessment of complications (varicose haemorrhage) over 36 months according to Kaplan-Meier that the proportion of patients without bleeding in group I was 79.27% and in group II – 87.98% (p=0.1264). The proportion of survivors at 36 months in group I was 78.48%, in group II – 83.16% (p=0.5525).
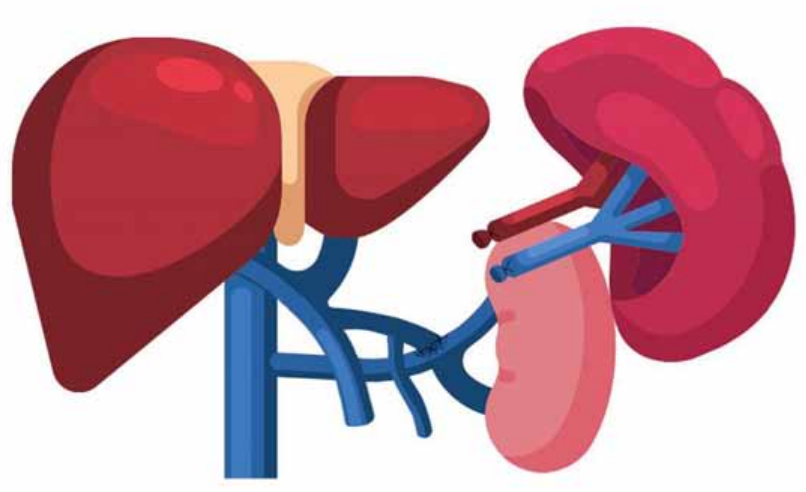
Рисунок 1. Схематическое изображение спленоренального венозного шунтирования после спленэктомии (рисунок автора)
Figure 1. Schematic representation of splenorenal venous bypass surgery after splenectomy (author's drawing)

Рисунок 2. Спиральная компьютерная томограмма пациентки Л., 29 л., через 7 лет после операции спленоренального венозного шунтирования. КТ признаки множественных сосудистых анастомозов вокруг головки поджелудочной железы с ветвями брыжеечной вены и левой почечной веной, расширение яичниковой вены
Figure 2. Spiral computed tomography of patient L., 29 years old, 7 years after splenorenal venous bypass surgery. CT scan shows signs of multiple vascular anastomoses around the head of the pancreas with branches of the mesenteric vein and the left renal vein, dilation of the ovarian vein
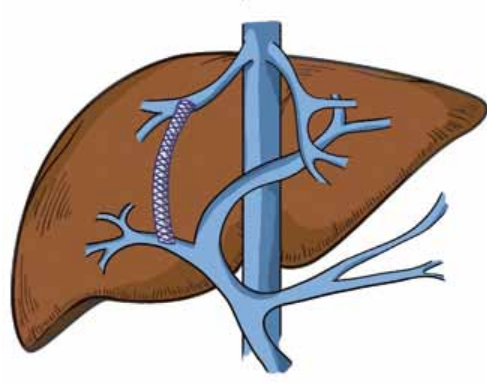
Рисунок 3. Схематическое изображение трансъюгулярного внутрипеченочного портосистемного шунтирования (рисунок автора)
Figure 3. Schematic representation of transjugular intrahepatic portosystemic shunt (author's drawing)
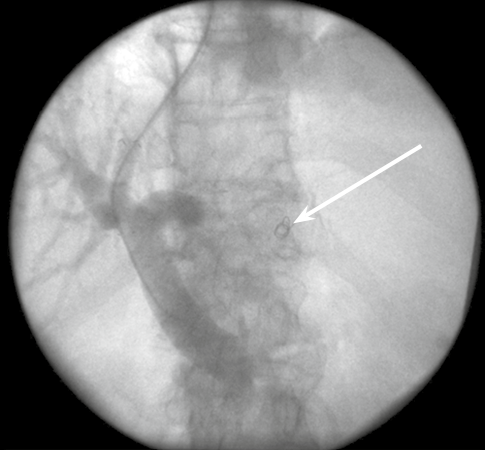
Рисунок 4. Ангиограмма больного К., 72 г. (контрольная портограмма после выполнения эмболизации спиралями Gianturco левой желудочной вены через сформированный внутрипеченочный канал). Стрелкой указана спираль Gianturco.
Figure 4. Angiogram of patient K., 72 L. (control portogram after Gianturco spiral embolization of the left gastric vein through the formed intrahepatic duct). The arrow indicates the Gianturco spiral
The Rostov surgical school, possessing a very serious experience in performing endovascular interventions for PH in the Russian Federation, made a certain contribution to the improvement of the TIPS operation methodology. This is evidenced by 10 inventions of RostGMU patented in the Russian Federation. One doctoral and thirteen candidate theses under the guidance of professors I.I. Katelnitsky, Yu.V. Khoronko, N.G. Sapronova, and V.L. Korobka were defended on the topical issue of surgical treatment of PH complications.
At the origins of the TIPS operation at the university hospital, there were X-ray endovascular surgeons Mark Iosifovich Polyak and Evgeny Valerievich Kosovtsev. Currently, the huge experience, golden hands, and an inquisitive mind of the candidate of medical sciences, assistant professor E.V. Kosovtseva, under the guidance of Yu.V. Khoronko, determine the further vector of PH surgery development in Rostov-on-Don. After analyzing the course and outcome of treatment in 172 patients with intrahepatic PH, E.V. Kosovtsev substantiated the need for surgical blocking of the inflow paths to esophageal and gastric varices in addition to the shunt stage of TIPS surgery, and also found that the risk of complication in the form of stent displacement increased when stenting the intrahepatic canal as the first stage. Therefore, it is necessary to carry out a stage of selective embolization of the inflow pathways to esophageal and gastric varices before the stage of stenting the intrahepatic portosystemic channel2. Conclusions and practical recommendations have become a postulate for specialists involved in PH surgery.
The results of the Rostov school of surgeons were published by I.I. Katelnitsky and N.G. Sapronova in the form of lectures on PH in the collections 50 Lectures on Surgery (edited by V.S. Savelyev) (2005) and 80 Lectures on Surgery (under the general editorship of V.S. Savelyev) (2008) [8]. Yu.V. Khoronko et al. published 3 monographs on the problems of modern surgery, dedicated to TIPS surgery and the treatment of varicose esophageal-gastric bleeding (2013) [9], encephalopathy in PH and after portosystemic bypass interventions (2020) [10], a multidisciplinary approach to the surgical treatment of liver cirrhosis (2021) [1], which have become desktop books for students and young surgeons.
Not long ago, Yu.V. Khoronko in a monograph (2013) noted that portal vein thrombosis (PVT) or its post-thrombotic transformation is a relative contraindication to this shunt intervention [9], and there were reasons for this. Opponents of the operation regarded a thrombus or cavernous transformation as an insurmountable obstacle that prevents a full bypass of the PV system [11]. Nonetheless, from 2017 to 2024 at the RostSMU clinic, 26 successful TIPS operations were performed at complicated PH in patients with LC under conditions of thrombosis in the PV system. The operation was performed according to a generally accepted method; its feature was the preoperative design of the puncture trajectory in the direction of PV, previously calculated using a three-dimensional reconstruction of computer images of MSCT with intravenous contrast enhancement and mechanical or drug-induced destruction of the thrombus with simultaneous aspiration or rotational thrombus extraction. In this situation, a non-occlusive thrombus was pushed back to the vascular wall with a stent. The obtained results of achieving portal decompression determined that in a situation with PVT, the only saving solution is TIPS surgery performed in a specialized medical institution by a surgeon with wide experience in such interventions.
Discussion
We did not dwell in our thematic review on routine surgical interventions that are performed everywhere, saving the lives of patients with complications of PH. Rethinking the indications for portosystem bypass operations is a new approach recognized by the world community. Most medical hospitals in the Russian Federation have the capabilities and use the methods of surgical treatment (endoscopic, azygoportal separation operations), along with conservative methods of treating complications of PH (bleeding, ascites). The largest centers have in their arsenal X-ray endovascular methods of treating patients with PH. X-ray operating room equipment and supplies for TIPS are a high-tech and expensive component. The ongoing modernization of the health care system, aimed at improving the accessibility of high-tech medical care for the population, will allow patients to receive it absolutely free of charge without leaving their region. If ten years ago, the operation was perceived as a “bridge to transplantation”, now it has reached an independent level and occupies a leading place in terms of the effectiveness of reducing PSG pressure. So far, in the Russian Federation, there are only a few centers where this surgical intervention is performed (Moscow, St. Petersburg, Rostov-on-Don, Krasnodar, and Surgut). The development of PH surgery in a single region of the South of Russia has come in a truly unique way: from Bogoraz surgery, performed so far in individual institutions, to TIPS surgery. This would not have happened if there were no team of like-minded people who know that all attempts to save the lives of patients with severe complications have a prospect. The purpose of our review was not to conduct a detailed analysis of the complications of PSG pressure reduction techniques and a comparative analysis of patient life expectancy. It should be noted that monitoring of patients of group I showed the following: at present, communication has been lost with 12/73 patients (16.43%), 60/73 (82.19%) have been diagnosed with a lethal outcome at different times after surgery from 5 to 16 years, and the only one patient 1/73 (1.37%) has been in touch for 19 years after surgery. The development of a scientific platform in the South of Russia, mutual work with specialists from the Krasnodar Region, will make it possible to bring the TIPS methodology to the level of routine practice performed for emergency indications.
Conclusions
Despite the wide experience of the Rostov school of surgeons involved in the treatment of patients with complicated PH and a large number of experimental and clinical studies, the section of surgery devoted to the treatment of liver cirrhosis complications remains open in its knowledge and development. Science is moving forward along with world achievements and discoveries; attention to the problem of patients with liver cirrhosis is quite large. In 2010, V. N. Shipovsky mentioned 200 TIPS operations [7] performed in the centers of the Russian Federation. To date, 315 operations have been performed in the clinic of Rostov State Medical University alone. The era of effective treatment of PH, which began in the 1970s, has undergone many changes for the better due to the development of technologies and equipment of medical institutions, but one must not stop there. New difficulties await us, and overcoming them from a scientific and practical point of view determines our further path along the winding historical road of PH surgery.
1. Sapronova N.G. Rationale for choosing a treatment method for patients with portal hypertension: dis. doc. medic. sciences. Rostov-on-Don, 2014. 260 p.
2. Kosovtsev E.V. Optimization of portosystemic shunting aids (operations of transjugular intrahepatic portosystemic stent shunting) in patients with complicated portal hypertension of cirrhotic genesis: dis. cand. medic. sciences. Rostov-on-Don, 2020. 194 pp.
References
1. ДDurleshter V.M., Korochanskaya N.V., Gabriel S.A., Krushelnitsky V.S., Khoronko Yu.V., et al. Surgical treatment of liver cirrhosis: a multidisciplinary approach: monograph. Moscow: Practical Medicine, 2021. (In Russ.).
2. Korobka R.V., Gautier S.V., Khoronko Yu.S., Pasechnikov V.D., Sapronova N.G., et al. Transjugular intrahepatic portosystemic shunt or a combination of nonselective beta blockers and endoscopic variceal ligation for prophylaxis of bleeding in waitlisted cirrhotic patients. Russian Journal of Transplantology and Artificial Organs. 2024;26(2):16-27. (In Russ.). https://doi.org/10.15825/1995-1191-2024-2-16-27.
3. Bogoraz N.A. About transplantation of the superior mesenteric vein into the inferior vena cava for cirrhosis of the liver. Russian doctor. 1913;12(2):48-50.. (In Russ.).
4. Anisimov A.Yu. Ego videre a longe. Historical outline of the development of portal hypertension surgery. Moscow – Kazan: Medicine, 2022. (In Russ.).
5. Khoronko Yu.V., Dmitriev A.V., Sarkisov A.E., Mikryukov V.A. Рortosystemic shunt operations in the surgery of portal hypertension: from Еck’s fistula to tips procedure (dedicated to 100 years’ jubilee of mesentericocaval shunt – Вogoraz’s operation). Medical Herald of the South of Russia. 2014;(1):28-34. (In Russ.) https://doi.org/10.21886/2219-8075-2014-1-28-34.
6. Khoronko Yu.V., Kosovtsev E.V., Korobka R.V., Sarkisov A.E., Khoronko E.Yu., Ashimov I.A., Tadieva E.V. Portosystemic shunt for variceal esophagogastric bleeding and risk of early relapse. Rationale for involuntary intervention: А single-center observational controlled study. Kuban Scientific Medical Bulletin. 2024;31(3):57–72. (In Russ.). https://doi.org/10.25207/1608-6228-2024-31-3-57-72.
7. Shipovsky V.N. Technique of TIPS operation. Practical guide. Moscow: Publisher I.V. Balabanov, 2010. (In Russ.).
8. 80 lectures on surgery. Under the general editorship. Moscow: Litterra, 2008. (In Russ.)
9. Khoronko Yu.V., Cherkasov M.F., Polyak M.I., Baranov Yu.E. TIPS/TIPS (transjugular intrahepatic portosystemic shunting) and treatment of variceal esophageal-gastric bleeding. Moscow: JSC «Pharm-Sintez», 2013. (In Russ.).
10. Khoronko Yu.V., Groshilin V.S., Sidorov R.V., Kochubeynik N.V., Prostov I.I., et al. Encephalopathy in portal hypertension and after bypass surgery: prevention and treatment. Rostov-on-Don: Synthesis of Technologies LLC, 2020. (In Russ.).
11. Khoronko Yu.V., Sapronova N.G., Vetshev P.S., Korobka R.V., Kosovtsev E.V., et al. Transjugular intrahepatic portosystemic shunt for portal vein thrombosis in the context of complicated portal hypertension of cirrhotic origin. Annaly khirurgicheskoy gepatologii = Annals of HPB surgery. 2024; 29 (4): 53–65. (In Russ.) https://doi.org/10.16931/1995-5464.2024-4-53-65.
About the Authors
N. G. SapronovaРоссия
Natalia G. Sapronova, Dr. Sci. (Med.), Professor, Head of the Department of surgical diseases №1
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
Yu. V. Khoronko
Россия
Yury V. Khoronko, Dr. Sci. (Med.), Professor, Head of the Department of Operative Surgery and Topographic Anatomy
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
A. F. Balandin
Россия
Artem F. Balandin, 6th year student, Rostov State Medical University
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
N. A. Malitsky
Россия
Nikita A. Malitsky, 6th year student
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
M. G. Oganesian
Россия
Mariam G. Oganesian, 6th year student
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
D. A. Balyasnikova
Россия
Daria A. Balyasnikova, 6th year student
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
M. R. Kantsurova
Россия
Maria R. Kantsurova, assistant of the Department of obstetrics and gynecology №1
Rostov-on-Don
Competing Interests:
Authors declare no conflict of interest
Review
For citations:
Sapronova N.G., Khoronko Yu.V., Balandin A.F., Malitsky N.A., Oganesian M.G., Balyasnikova D.A., Kantsurova M.R. Past and present of portal hypertension surgery (about the Rostov school of surgeons). Medical Herald of the South of Russia. 2025;16(2):128-135. (In Russ.) https://doi.org/10.21886/2219-8075-2025-16-2-128-135
JATS XML







































