Scroll to:
Results of a personalized approach to surgical correction of portal hypertension in patients with liver cirrhosis
https://doi.org/10.21886/2219-8075-2024-15-2-54-60
Abstract
Objective: to improve the results of treatment of patients with complicated intrahepatic portal hypertension by developing optimal surgical treatment tactics and choosing drug correction aimed at preventing thrombotic venous complications.
Materials and methods: 82 patients with clinically significant portal hypertension of cirrhotic origin were examined and treated. The I group consisted of 24 patients who underwent transjugular intrahepatic portosystemic stent bypass surgery, the II group included 58 patients for whom the operation was supplemented with selective embolization of the gastric veins. Methods: clinical and laboratory examination, “Thrombodynamics” test using a “prognostic calculator” (RF patent), surgical, statistical.
Results: it was established that 26,8% of patients had a risk of developing venous thrombotic complications: in group I 4/24 (16,6%), in group II — 18/58 (31,0%). Personalized drug correction carried out in the postoperative period led to the absence of risk in 2/22 (9,1%) patients in group I and in 8/53 (15,1%) in group II. The number of deaths in group I was 2/24 (8,33%) and in group II 5/58 (8,62%). Shunt thrombosis was detected in 3/22 (13,63%) patients of group I and in 1/53 (1,88%) patients of group II in the period from 24 to 32 months after surgery. Varicose esophageal-gastric bleeding occurred in 2/22 (9,00%) patients with shunt thrombosis of group I and in 1/53 (1,88%) of group II patients who underwent endoscopic ligation of esophageal varices.
Conclusion: a method for predicting the risk of developing thrombotic complications in patients with liver cirrhosis is a convenient tool for risk stratification of patients. An individual approach ensures monitoring of the patient not only before, but also after the operation. Drug correction regimens for identifying high, moderate and low risks of complications made it possible to prevent them. TIPS surgery alone and in combination with selective embolization of gastric veins allows achieving comparable results in observation groups against the background of corrective therapy.
For citations:
Sapronova N.G., Kantsurov R.N., Stagniev D.V., Frolova A.A. Results of a personalized approach to surgical correction of portal hypertension in patients with liver cirrhosis. Medical Herald of the South of Russia. 2024;15(2):54-60. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-2-54-60
Introduction
According to WHO, intrahepatic portal hypertension (IPH) (according to the Baveno VII consensus (2021) – “Clinically significant portal hypertension” (CSPH)) is the cause of death of almost a million people per year [1]. In economically developed countries, despite progress in approaches to diagnosis and treatment, hepatic cirrhosis (HC) is among the six leading causes of death in working-age patients aged 35 to 60 years [2][3].
Esophagogastric variceal hemorrhage is one of the life-threatening and most common HC complications. The mortality rate from the first episode is 10–20%, while with the decompensated cirrhosis, it constitutes 76–80% [4].
The current state of surgery complicated by IPH caused by HC is characterized by minimally invasive endovascular interventions being more widely introduced into clinical practice than previously and reducing the portosystemic pressure gradient in order to stop and prevent esophagogastric variceal hemorrhage, refractory ascites, and the development of hepatorenal syndrome [5]. In recent years, indications for transjugular intrahepatic portosystemic shunting (TIPS) have been steadily expanding in Russia [6].
The surgical clinic of the Rostov State Medical University has extensive experience in performing this type of surgical intervention for the last 15 years.
The research was aimed at improving the treatment results of patients with complicated IPH by developing optimal surgical treatment tactics and choosing pharmacological correction aimed at preventing venous thrombotic complications.
Materials and methods
The research groups included 82 patients with HC complicated by IPH, treated in the period from 2016 to 2021 in the surgical clinic of the Rostov State Medical University. The patients were divided into two groups: patients of group I underwent TIPS surgery (n=24), and patients of group II underwent TIPS surgery with selective embolization of the gastric veins (n=58). The data were analyzed using Statistica SPSS 26.0 (IBM Statistic, USA) by means of descriptive and variation statistics methods. Mathematical calculations for the parameters obtained during the research were performed using standard functions, modules, and formula builders. In group I, there were 11/24 women (45.8%) and 13/24 men (54.2%), in group II – 29/58 women (50%) and 29/58 men (50%), p=0.731. The mean age in group I was M±SD: 52±9 years [ 95% CI: 48–56], in group II – M±SD: 54±11 years [ 95% CI: 52-57], p=0.305. The median disease duration (MD) in group I was Me: 4 [Q1-Q₃: 3–5], in group II – Me: 5 [Q1-Q₃: 2–10], p<0.05. According to the classes of hepatocellular failure by Child-Turcotte-Pugh, the patients were distributed as follows: in group I, class A – 14/24 (58.3%), class B – 7/24 (29.2%), class C – 3/24 (12.5%); in group II, class A – 35/58 (60.3%), class B – 20/58 (34.5%), class C – 3/58 (5.2%). When considering the grade of esophageal and gastric varices (EGV) according to Paquet, grade 1EGV was not established in the observation groups. In group I, grade 2 EGV was present in 3/24 (12.5%) patients, grade 3 EGV – in 21/24 (87.5%) patients, and grade 4 EGV was absent. In group II, 8/58 (13.8%) patients had grade 2 EGV, 44/58 (75.9%) patients had grade 3 EGV, and 6/58 (10.3%) patients had grade 4 EGV. These data characterized the severity of PH manifestations in patients in the groups, determining the possibility of the most formidable complication in the form of esophagogastric variceal hemorrhage.
In the anamnesis, episodes of esophagogastric variceal hemorrhage were present on average in group I Me: 1 [Q1-Q₃: 0–1], in group II — Me: 1 [Q1-Q₃: 1–2], p=0.009, which determined the choice of surgical intervention toward TIPS or TIPS with selective gastric vein embolization. In order to assess the results of the performed surgical interventions and pharmacological treatment in patients in groups I and II, the lethal outcome, as well as cases of complications after surgical portosystemic shunting (shunt thrombosis, episodes of esophagogastric variceal hemorrhage) were identified. The timing of events was calculated in months. The observation period ranged from 1 to 71 months.
Results
The distribution of patients by Child-Turcotte-Pugh hepatocellular failure classes before surgery was determined by a certain preoperative preparation, including the use of non-selective β-blockers (propranolol), ursodeoxycholic acid, octreotide 100–200 mcg/day, and glucose-salt solutions with diuresis correction. The inevitable progression of hepatic encephalopathy after shunting surgery was prevented by taking lactulose 30–60 ml/day per os, rifaximin 800–1200 mg/day per os, and L-ornithine-L-aspartate 10–15 g per os daily. Standard prevention of thromboembolic complications during surgery for all patients included intravenous administration of 5000 U of heparin.
In accordance with the stated goal of preventing thrombotic venous complications, patients were prescribed corrective therapy, including anticoagulants and antiplatelet agents according to a specific scheme. The choice of a combination of these drugs was due to the features of the coagulation and cellular mechanisms of hemostasis disorders in patients with HC and a specific type of surgical intervention (TIPS or TIPS with gastric vein embolization), when platelet aggregation occurred in the lumen of the installed stent and microthrombi were formed in the target organs.
The method for predicting the risk of developing thrombotic complications in the postoperative period in patients with HC after TIPS, registered by the Russian Federation patent for invention No. 2717210, was based on the use of the discriminant method of statistical analysis, where a set of laboratory parameters of the hemostasis system was used as independent predictors (two from the Thrombodynamics test – clot size after 30 minutes and the presence of spontaneous clots, two from the coagulogram – INR and prothrombin time) (Table 1).
Таблица / Table 1
Анализ показателей предикторов в группах наблюдения
Analysis of predictor indicators in observation groups
|
Показатели Indicators |
Категории Categories |
M ± SD / Me |
95% ДИ / Q₁ – Q₃ |
n |
p |
|
Размер сгустка через 30 мин. Clot size after 30 min (Сs) (мкм / mkm) |
I группа / group |
1083 ± 123 |
1031 – 1135 |
24 |
0,032 |
|
II группа / group |
1166 ± 119 |
1134 – 1197 |
58 |
||
|
МНО INR |
I группа / group |
1,29 |
1,20 – 1,46 |
24 |
0,666 |
|
II группа / group |
1,31 |
1,21 – 1,46 |
58 |
||
|
ПТВ PTT (сек. / sec) |
I группа / group |
17 |
15 – 19 |
24 |
0,448 |
|
II группа / group |
17 |
15 – 19 |
58 |
According to Thrombodynamics data, spontaneous clots were found in 5/24 (20.8%) patients in group I and in 12/58 (20.7%) patients in group II.
The “classification weight” (belonging) of the patient to the group without predicted thrombus formation in the shunt (Y1) and the patient's belonging to the group with predicted thrombus formation in the shunt (Y2) were determined, which was calculated using the “prognostic calculator”. With the “classification weight” value Y1>Y2, the absence of the probability of shunt thrombosis in the patient was predicted (probability – less than 50%), with Y1<Y2, a high probability (more than 50%) of postoperative venous thrombosis was predicted.
Of the 82 patients in both groups, 11/82 (13.4%) patients showed negative values of the “Classification weight difference” indicator on the “prognostic calculator”, which was assessed as a high risk of developing thrombotic complications; another 11/82 (13.4%) patients showed positive indicators of the risk of developing these complications, since the positive values of the difference did not exceed the value of “+4”. Therefore, 22/82 (26.8%) of the examined patients with HC were at risk of developing venous thrombotic complications. The value of the “Classification weight difference” indicator was assessed, and it was found that in 5/82 (6.1%) patients, this risk was high (Y1-Y2)≤-4, in 6/82 (7.3%) patients it was moderate (Y1-Y2)>-4<0, and in 11/82 (13.4%) patients it was low (Y1-Y2)>0≤4. In 60/82 (73.2%) patients with a calculated difference exceeding 4 on the “prognostic calculator”, there was no risk of thrombotic complications. These patients were distributed among the observation groups as follows: in group I – 4/24 (16.6%) patients, and in group II – 18/58 (31.0%) patients. The distribution of patients in the observation groups by the Child-Turcotte-Pugh class while considering the “Classification weight difference” (Y1-Y2) by groups is shown in Figs. 1, 2.
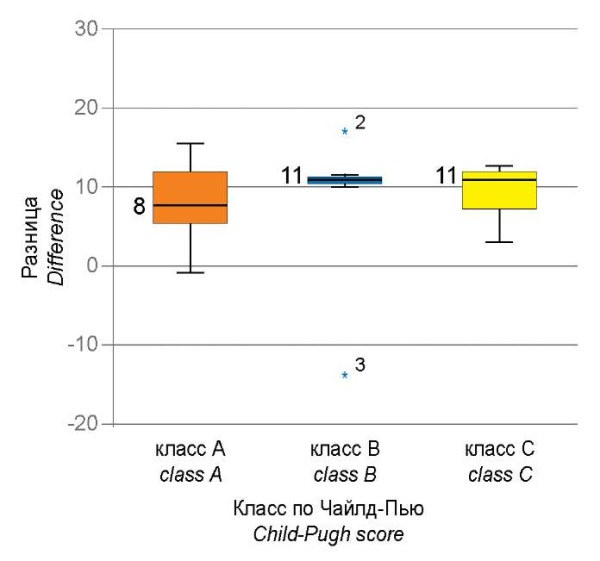
Рисунок 1. Анализ показателя «Разница весов классификации» (Y1-Y2)
в зависимости от показателя «Класс по Child-Turcotte-Pugh»
у пациентов I группы до операции, р=0,572.
Figure 1. Analysis of the indicator “Difference in classification weights” (Y1-Y2)
depending on the indicator “Class according to Child-Turcotte-Pugh”
in patients of group I before surgery, p = 0,572.
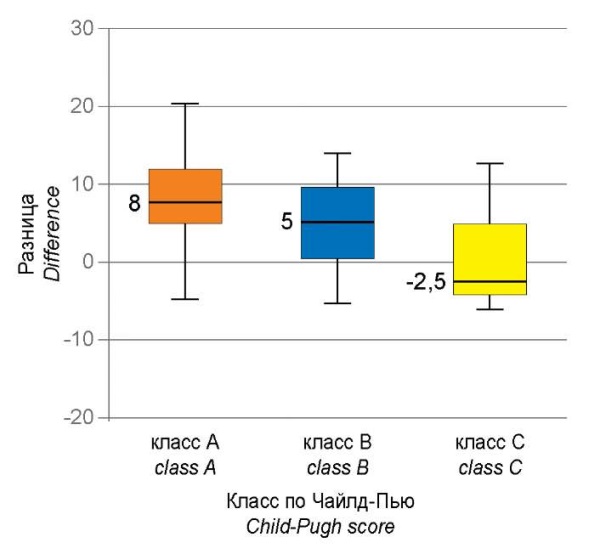
Рисунок 2. Анализ показателя «Разница весов классификации» (Y1-Y2)
в зависимости от показателя «Класс по Child-Turcotte-Pugh»
у пациентов II группы до операции, р=0,033.
Figure 2. Analysis of the indicator “Difference in classification weights” (Y1-Y2)
depending on the indicator “Class according to Child-Turcotte-Pugh”
in patients of group II before surgery, p = 0,033.
Therefore, having determined the risk stratification of thrombotic complications in patients in the observation groups, pharmacological correction of possible complications in patients with high, moderate, and low risk according to hepatocellular failure classes by Child-Turcotte-Pugh was performed. High-risk patients of Child-Turcotte-Pugh classes A and B were prescribed anticoagulants (enoxaparin sodium) at a dosage of 20 mg subcutaneously once a day for 10 days with subsequent hemostasis monitoring and after 10 days were transferred to oral antiplatelet agents (clopidogrel 75 mg) 1 time per day with subsequent hemostasis monitoring 1 time in 10 days. High-risk patients of Child-Turcotte-Pugh class C were prescribed anticoagulants (enoxaparin sodium) at a dosage of 20 mg subcutaneously once a day for 10 days with subsequent hemostasis monitoring. Patients with a moderate risk of developing thrombotic complications of Child-Turcotte-Pugh class A and B were prescribed oral antiplatelet agents (clopidogrel 75 mg) once a day, followed by hemostasis monitoring once every 10 days. Patients with a moderate risk of Child-Turcotte-Pugh class C were prescribed oral antiplatelet agents (disaggregants) (acetylsalicylic acid) at a dosage of 100 mg once a day, followed by hemostasis monitoring once every 10 days. Patients with a low risk of Child-Turcotte-Pugh classes A, B and C were prescribed oral antiplatelet agents (disaggregants) (acetylsalicylic acid)) at a dosage of 100 mg once a day, followed by hemostasis monitoring once every 10 days. The therapy was selected individually for each patient under the control of a coagulogram, the “Thrombodynamics” test using a “prognostic calculator” and lasted from 10 days to 4 months; if the risk group changed during treatment, the prescriptions were adjusted.
The number of fatal outcomes in the observation groups was as follows: group I – 2/24 (8.33%) patients, group II – 5/58 (8.62%) patients.
Similar to the preoperative examination, the analysis of the “Classification weight difference” (Y1–Y2) indicator was performed in the groups 4–5 months after surgery. In 2/22 (9.1%) patients in group I and in 8/53 (15.1%) patients in group II while considering two deceased in group I and five deceased in group II, a low risk of developing venous thrombotic complications was detected, which required prolongation of corrective therapy for another 2–4 months. In 2/22 (9.1%) patients in group I and in 8/53 (15.1%) patients in group II, there was no risk of developing venous thrombotic complications.
A comparative analysis of the predictor “Classification weight difference” (Y1–Y2) was also conducted in patients of groups I and II according to the hepatocellular failure classes by Child-Turcotte-Pugh against the background of corrective therapy (Figs. 3, 4).
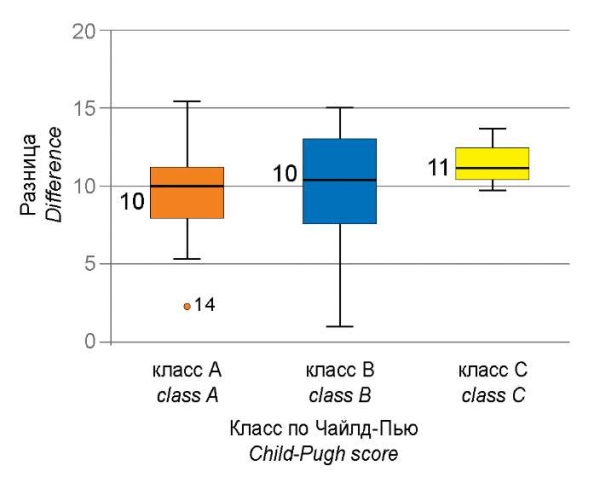
Рисунок 3. Анализ показателя «Разница весов классификации» (Y1-Y2) после операции
в зависимости от показателя «Класс по Child-Turcotte-Pugh»
у пациентов I группы, р=0,726.
Figure 3. Analysis of the indicator “Difference in classification weights” (Y1–Y2)
after surgery depending on the indicator “Child-Turcotte-Pugh Class”
in patients of group I, p = 0,726.
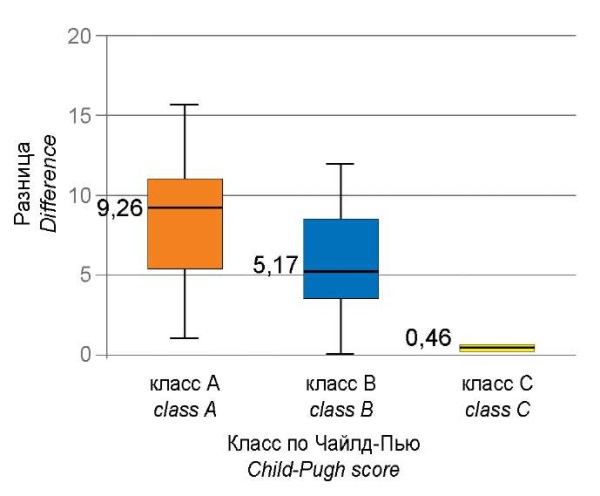
Рисунок 4. Анализ показателя «Разница весов классификации» (Y1–Y2) после операции
в зависимости от показателя «Класс по Child-Turcotte-Pugh»
у пациентов II группы, р=0,021.
Figure 4. Analysis of the indicator “Difference in classification weights” (Y1-Y2)
after surgery depending on the indicator “Child-Turcotte-Pugh Class”
in patients of group II, p = 0,021.
Discussion
After surgery, statistically significant differences (p=0.021) in the “Classification weight difference” indicator were established in patients of group II in class C. However, in patients of group I, there were no statistically significant differences in this parameter (p=0.726).
When analyzing the long-term treatment results, on the one hand, the incidence of death as the most unfavorable consequence was assessed, taking into account the period of its occurrence, and on the other hand, the event-free survival rate was identified in the event of hemorrhage and/or shunt thrombosis.
During the observation period, shunt thrombosis manifested by hemorrhage was detected in 3/22 (13.63%) patients of group I and in 1/53 (1.88%) patients of group II in the periods from 24 to 32 months after surgery, who were not included in the risk groups for thrombotic complications and did not receive corrective therapy. Esophagogastric variceal hemorrhage occurred in 2/22 (9.00%) patients with shunt thrombosis of group I and in 1/53 (1.88%) patients of group II who underwent endoscopic ligation of esophageal varices. Of these, in one patient of group I, shunt thrombosis was detected during ultrasound examination without manifestation of variceal hemorrhage.
The next step was to assess the dependence of the risk of developing a fatal outcome on the TIPS technique in the observation groups, assessed using the Mantel-Cox Log-rank criterion when defining survival using the Kaplan-Meier method. At the same time, no statistically significant difference in survival rate in the subgroups was found (p=0.895) (Fig. 5). The average time to developing a fatal outcome was 63.4±3.8 months in group I (95% CI: 55.9–70.84), 65.25±2.2 months – in group II (95% CI: 60.45–70.04).
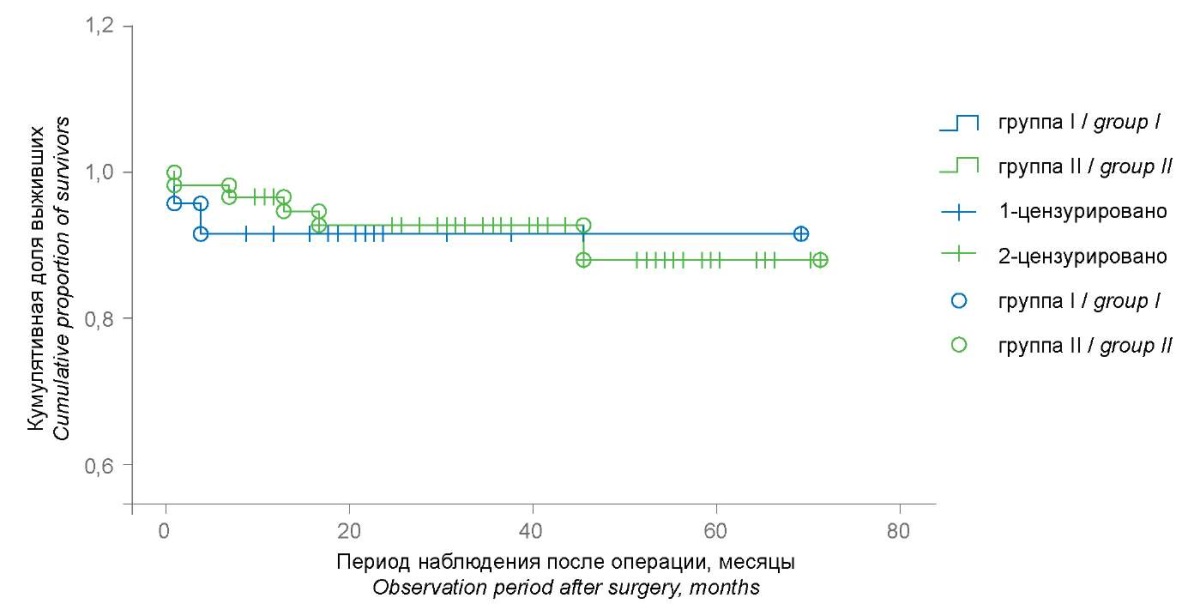
Рисунок 5. Анализ выживаемости пациентов I группы (n=24) и II группы (n=58)
с помощью метода Каплан-Майера и оценкой статистической разницы
с помощью Log-rank критерия Мантеля-Кокса, р=0,895.
Figure 5. Analysis of survival of patients in groups I (n=24) and group II (n=58)
using the Kaplan-Meier method and assessing the statistical difference
using the Log-rank Mantel-Cox test, p=0,895.
The dynamics of the accumulated proportion of survivors by the end of the interval for 66 months after surgery did not change in group I, being determined at the level of 0.92 while considering the death of two patients in the first observation interval, and decreased in group II from 0.98 to 0.88; however, no statistically significant difference was found either (p=0.754).1
Conclusion
The developed method for predicting the risk of developing thrombotic complications in patients with HC (RU Patent No. 2717210) is a convenient tool for risk stratification of patients and allows identifying the risk of developing complications before TIPS surgery due to an individual approach by means of using the “Classification weight difference” indicator of the mathematical model, and also ensures patient monitoring not only before but also after surgery.
The use of the developed schemes of individual pharmacological correction in patients with high, moderate, and low risk of developing thrombotic venous complications allows preventing them in patients of different hepatocellular failure classes by Child-Turcotte-Pugh.
A comparative analysis of the results of patient treatment has demonstrated that TIPS surgery alone and in combination with selective embolization of the gastric veins, while also considering risk stratification and the algorithm for its implementation, allows achieving comparable results in observation groups against the background of corrective therapy, helps to prevent life-threatening complications, and increases survival rate.
1. Kantsurov R.N. Justification of the algorithm for surgical treatment of patients with complicated intrahepatic portal hypertension: diss. ... candidate of medical sciences / R.N. Kantsurov. Rostov-on-Don, 2022, 148 p.
References
1. de Franchis R, Bosch J, Garcia-Tsao G, Reiberger T, Ripoll C; Baveno VII Faculty. Baveno VII - Renewing consensus in portal hypertension. J Hepatol. 2022;76(4):959-974. Erratum in: J Hepatol. 2022. PMID: 35120736. https://doi.org/10.1016/j.jhep.2021.12.022
2. Korobka V.L., Pasechnikov V.D., Korobka R.V., Pak E.S., Shapovalov A.M., Pasechnikov D.V. Nonselective beta-blockers in primary prophylaxis of esophageal variceal bleeding in patients with ascites waitlisted for liver transplantation. Russian Journal of Transplantology and Artificial Organs. 2023;25(1):68-76. (In Russ.) https://doi.org/10.15825/1995-1191-2023-1-68-76
3. GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5(3):245-266. https://doi.org/10.1016/S2468-1253(19)30349-8
4. Khoronko Yu.V., Sidorov R.V., Sapronova N.G., Kosovtsev E.V., Khoronko E.Yu., et al. Transjugular intrahepatic portosystemic shunt (TIPS procedure) for complicated portal hypertension: Evaluating efficacy and expanding intervention opportunities. Bulletin of Pirogov National Medical & Surgical Center. 2023;18(3):25-29. (In Russ.) https://doi.org/10.25881/20728255_2023_18_3_25
5. Sapronova N.G., Kalinin D.S., Kosovtsev E.V., Khoronko Yu.V., Stagniev D.V., et al. Results of transjugular intrahepatic portosystemic shunt combined with selective gastric vein embolization. Annaly khirurgicheskoy gepatologii = Annals of HPB Surgery. 2023;28(3):31-38. (In Russ.) https://doi.org/10.16931/1995-5464.2023-3-31-38
6. Durleshter V.M., Gabriel’ S.A., Korochanskaya N.V., Buhtoyarov A.Yu., Markov P.V., et al. Transjugular intrahepatic portosystemic stent-shunt as minimally invasive method of portal hypertension correction in multi-disciplinary clinic. Annaly khirurgicheskoy gepatologii = Annals of HPB Surgery. 2020;25(4):95-106. (In Russ.) https://doi.org/10.16931/1995-5464.2020495-106
About the Authors
N. G. SapronovaРоссия
Natalia G. Sapronova - Dr. Sci. (Med.), Professor, head of the Department of surgical diseases №1.
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest. The article was written based on materials from a defended dissertation, some of the results of which were not published
R. N. Kantsurov
Россия
Roman N. Kantsurov - Cand. Sci. (Med.), cardiovascular surgeon, Department of Vascular Surgery.
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest. The article was written based on materials from a defended dissertation, some of the results of which were not published
D. V. Stagniev
Россия
Dmitry V. Stagniev - Cand. Sci. (Med.), Associate Professor, Associate Professor of the Department of Surgical Diseases N1.
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest. The article was written based on materials from a defended dissertation, some of the results of which were not published
A. A. Frolova
Россия
Anastasia A. Frolova - 6th year student.
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest. The article was written based on materials from a defended dissertation, some of the results of which were not published
Review
For citations:
Sapronova N.G., Kantsurov R.N., Stagniev D.V., Frolova A.A. Results of a personalized approach to surgical correction of portal hypertension in patients with liver cirrhosis. Medical Herald of the South of Russia. 2024;15(2):54-60. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-2-54-60
JATS XML







































