Scroll to:
The influence of family history of schizophrenic spectrum disorders on the clinical presentation of schizophrenia
https://doi.org/10.21886/2219-8075-2024-15-3-26-32
Abstract
Objective: to identify the characteristics of the clinical debut of schizophrenia, as well as clinical aspects related to hereditary aggravation within schizophrenic spectrum disorders.
Materials and methods: patients with a confirmed diagnosis of F20.0 “Paranoid schizophrenia” selected according to inclusion/non-inclusion criteria participated in the study. Material was collected through clinical interviewing, analysis of medical records and documentation, and self-questionnaires.
Results: a total of 264 individuals participated in the study. Hereditary aggravation with schizophrenic spectrum disorders within two generations was detected in 127 of them (48.1%). Our results showed that having a family history of schizophrenic spectrum disorders correlated with earlier age of schizophrenia debut (p=0.018) and higher scores on the Calgary Depression Scale (p=0.013).
Conclusions: the findings may serve as an effective tool for developing more accurate diagnostic strategies in individuals at high risk of developing schizophrenia due to hereditary aggravation, as well as for the subsequent treatment of these individuals.
For citations:
Gashkarimov V.R., Sultanova R.I., Efremov I.S., Sabanaeva I.E., Iskhakov A.A., Bakirov L.R., Asadullin A.R. The influence of family history of schizophrenic spectrum disorders on the clinical presentation of schizophrenia. Medical Herald of the South of Russia. 2024;15(3):26-32. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-3-26-32
Introduction
Schizophrenia is one of the most complex and mysterious human diseases. Its multifaceted nature, variety of clinical manifestations, and unclear mechanisms of occurrence continue to arouse great interest among researchers. The term was introduced by Eugen Bleuler in 1908, but the exact etiopathogenetic mechanism of the disease has not yet been found [1][2]. Among the factors influencing the development of schizophrenia, hereditary predisposition is one of the most important, which in turn opens the way to understanding the genetic basis of this mental disorder [3]. Schizophrenia is a polygenic disease with a high heritability – about 80%. In addition to genetic mechanisms, epigenetic features, such as DNA methylation, also play a role in the development of schizophrenia [4][5].
As known, the hereditary burden of mental illness is a significant predictor of schizophrenia [6]. Mortensen et al. found that if both parents had schizophrenia, the chance of their child getting the disease was 46.9 times higher than that of children born to healthy parents; it was 7.2 times higher if only the father was affected and 9.3 times if only the mother was affected [7]. Kowalec et al. found that a family history of schizophrenia was associated with treatment-resistant schizophrenia [8]. Moreover, a family history of schizophrenia affects the age of onset and the severity of negative symptoms [9]. Käkelä et al. found out that a psychotic episode in the family history was associated with unfavorable professional and general outcomes of schizophrenia [10]. A Chinese study found that an early onset of schizophrenia was associated with a family history of schizophrenia [11].
A family history of schizophrenia can also serve as a predisposing factor for other diseases. For example, Sullivan et al. demonstrated that the chance of having a child with an autism spectrum disorder was 2.9 times higher if the parents suffered from schizophrenia [12]. Benros et al. established a statistically significant relationship between a family history of schizophrenia and an increased risk of developing autoimmune diseases [13]. There is also evidence of a relationship between the presence of genetic alleles of schizophrenia risk and cannabis use [14].
Therefore, the present research hypothesis is that a family history of schizophrenia spectrum disorders may play a key role in shaping the trajectory of the disease.
The research aims to determine the characteristics of the onset of schizophrenia, as well as the clinical features associated with a family history of schizophrenia spectrum disorders. This opens the door to a personalized approach to the treatment and management of schizophrenia, taking into account the individual characteristics of patients.
Materials and methods
This study involved respondents with a confirmed diagnosis of F20.0 Paranoid schizophrenia in accordance with the ICD-10 criteria. The study was conducted from January 17, 2021 to June 20, 2022 at the Ufa Republican Clinical Psychiatric Hospital. All the participants provided written informed consent. This study was approved by the Local Ethics Committee of the Federal State Budgetary Educational Institution of Higher Education Bashkir State Medical University of the Ministry of Health of the Russian Federation (Protocol No. 2 dated February 27, 2019). Inclusion criteria were: age 18–60 years and the absence of acute psychotic states. Patients were included 10–14 days after hospitalization. The exclusion criteria were: incapacity, dependence on psychoactive substances (except nicotine), difficulties in verbal contact, concomitant mental pathologies, pregnancy, severe somatic pathology, and also refusal to participate in the study after its beginning and identification of exclusion criteria during the clinical interview.
Information was collected through clinical interviews, answers to questions in self-completed questionnaires, and analysis of medical records. The following psychometric methods were used: the Positive and Negative Psychopathological Symptom Scale (PANSS), the Hamilton Anxiety Scale (HAM-A), the Calgary Depression Scale in Schizophrenia (CDSS), the Pittsburgh Sleep Quality Index (PSQI), the Insomnia Severity Index (ISI), the Clinical Global Impression (CGI), and the Global Assessment of Functioning (GAF). A family history of schizophrenia spectrum disorders was confirmed if the medical documentation indicated such diagnoses as schizophrenia, schizotypal disorder, chronic delusional disorders, schizoaffective disorder, bipolar affective disorder, depressive disorder with psychotic symptoms, and substance dependence syndrome in the respondent's relatives within two generations (parents, grandparents, uncles, aunts, cousins, and siblings). If the medical documentation did not contain information about a family history, but the respondent confidently stated it, a family history was also confirmed. Data analysis was performed using the IBM SPSS Statistics 26 software. The normality of quantitative variables distribution was assessed using the Shapiro-Wilk test. The Mann-Whitney U test was used to compare two independent populations. The method was chosen due to the lack of evidence of normal distribution of the quantitative data.
Results
A total of 264 people, 184 males (69.7%) and 80 females (30.3%) took part in the study. The average age of respondents was 39.7 ± 8.97. In 127 (48.1%) patients, a hereditary burden of schizophrenia spectrum disorders was revealed within two generations (parents, grandparents, uncles, aunts, cousins, and siblings).
The data presented in Table 1 were selected as variables dependent on the presence or absence of a hereditary burden.
Таблица / Table 1
Переменные, выбранные для поиска взаимосвязи с наличием наследственной отягощённости заболеваниями шизофренического спектра
Variables selected to search for a relationship with the presence of hereditary aggravation with schizophrenic spectrum disorders
|
№ |
Переменная / Variable |
Среднее значение / Average value |
Стандартная ошибка / Standard error |
|
1. |
Возраст инициального периода шизофрении (лет) Age of the initial period of schizophrenia (years) |
18.65 |
0.642 |
|
2. |
Возраст дебюта шизофрении (лет) Age of schizophrenia debut (years) |
23.35 |
0.587 |
|
3. |
Баллы по шкале PANSS PANSS score |
54.94 |
1.693 |
|
4. |
Субшкала «P» Subscale «P» |
12.73 |
0.543 |
|
5. |
Субшкала «N» Subscale «N» |
14.44 |
0.657 |
|
6. |
Субшкала «G» Subscale «G» |
27.77 |
0.833 |
|
7. |
Баллы по шкале HAM-A HAM-A score |
12.37 |
0.944 |
|
8. |
Баллы по шкале PSQI PSQI score |
6.45 |
0.322 |
|
9. |
Баллы по шкале ISI ISI score |
5.61 |
0.504 |
|
10. |
Баллы по шкале CDSS CDSS score |
3.8 |
0.384 |
|
11. |
Шкала CGI CGI score |
3.87 |
0.11 |
|
12. |
Шкала GAS GAS score |
62.18 |
1.782 |
To study the relationship, the data obtained from two groups (with and without a hereditary burden) was compared. The nonparametric method for independent samples, the Mann-Whitney U test, was used for the analysis, the results are presented in Table 2.
Таблица / Table 2
Взаимосвязь между наличием наследственной отягощённости заболеваниями шизофренического спектра и выбранными клиническими и анамнестическими данными
Relationship between the presence of hereditary aggravation of schizophrenic spectrum disorders and selected clinical and anamnestic data
|
№ |
Переменная / Variable |
U Манна-Уитни / Mann-Whitney U |
Стандартизованная статистика критерия / Standardized criterion statistics |
p-value |
|
1. |
Возраст инициального периода шизофрении (лет) Age of the initial period of schizophrenia (years) |
1323.5 |
-1.28 |
0.201 |
|
2. |
Возраст дебюта шизофрении (лет) Age of schizophrenia debut (years) |
7231.5 |
-2.372 |
0.018* |
|
3. |
Баллы по шкале PANSS PANSS score |
8474.5 |
-0.363 |
0.717 |
|
4. |
Субшкала «P» Subscale «P» |
8616 |
-0.136 |
0.892 |
|
5. |
Субшкала «N» Subscale «N» |
8234 |
-0.754 |
0.451 |
|
6. |
Субшкала «G» Subscale «G» |
8873 |
0.28 |
0.779 |
|
7. |
Баллы по шкале HAM-A HAM-A score |
9535 |
1.349 |
0.177 |
|
8. |
Баллы по шкале PSQI PSQI score |
9472.5 |
1.253 |
0.21 |
|
9. |
Баллы по шкале ISI ISI score |
9336 |
1.951 |
0.051 |
|
10. |
Баллы по шкале CDSS CDSS score |
10226.5 |
2.485 |
0.013* |
|
11. |
Шкала CGI CGI score |
7979 |
-1.117 |
0.264 |
|
12. |
Шкала GAS GAS score |
9478 |
1.392 |
0.164 |
Примечание: * — p-value < 0.05.
Note: * — p-value < 0.05.
The authors of the present research found that a burdened family history was associated with an earlier age of schizophrenia onset (p=0.018) and higher scores on the Calgary Depression Scale in Schizophrenia (p=0.013). The average age of schizophrenia onset with a family history was 22.59±6.37 years (95% CI 21.46–23.72, median – 22), and without a family history, it was 23.83±5.88 years (95% CI 22.81–25.85, median – 23). The average CDSS score in the group with an adverse family history was 4.58±4.64 (95% CI 3.76–5.4, median – 3), in the group without a family history, it was 3.39±3.65 (95% CI 2.76–4.02, median – 2). The results are presented in Figures 1 and 2.
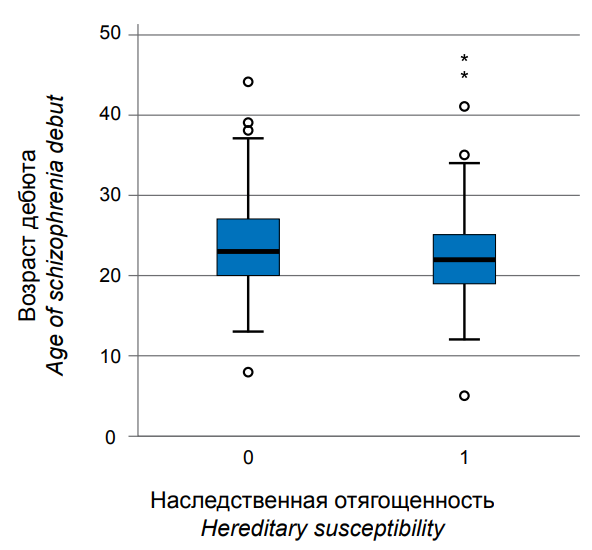
Рисунок 1. Взаимосвязь между возрастом дебюта шизофрении и наследственной отягощённостью заболеваниями шизофренического спектра.
Figure 1. Relationship between age of schizophrenia debut and hereditary susceptibility to schizophrenic spectrum disorders.
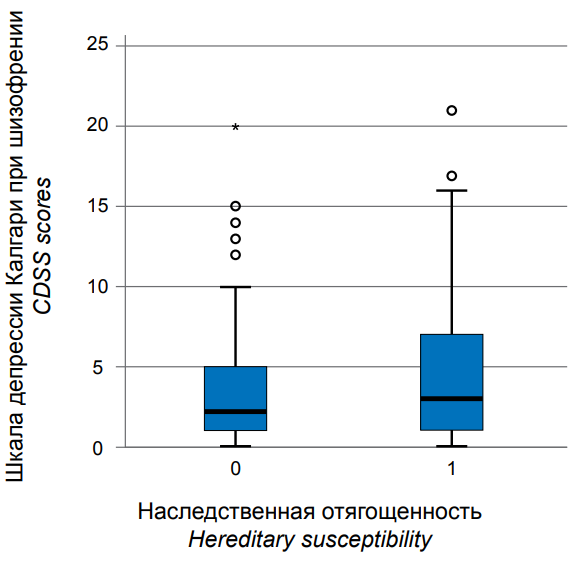
Рисунок 2. Взаимосвязь между количеством баллов по шкале CDSS и наследственной отягощённостью заболеваниями шизофренического спектра.
Figure 2. Relationship between CDSS scores and heritability of schizophrenic spectrum disorders.
Discussion
The present study confirms the existing ideas about the importance of the genetic component in the risk of developing schizophrenia. A family history of schizophrenia spectrum disorders is associated with an earlier age of onset, which is consistent with the assumptions about genetic predisposition as a factor influencing the biological basis of this disorder [15][16]. Similar results are found in other studies [9][11].
Another interesting aspect of the results is the discovered link between the hereditary burden and a higher level of depressive symptoms in people with schizophrenia. In turn, depressive symptoms in schizophrenia significantly affect the clinical picture of the disease and can lead to suicide [17][18], especially in case of concomitant alcohol dependence [19]. This observation probably indicates complex relationships between genetic risk factors for schizophrenia and the emotional state of patients, requiring a more in-depth study. For example, Peitl et al. established a relationship between certain polymorphisms of genes encoding SERT and MAO-A proteins and depressive symptoms in schizophrenia [20]. A series of Chinese studies established the influence of polymorphisms of various genes on the risk of developing both schizophrenia and depressive disorder: GSK3B [21], CMYA5 [22], GRM7 and GRM8 [23], NRG1 [24], CACNA1C [25].
The present study is not without limitations, one of them being the lack of data on specific genetic markers associated with schizophrenia in the family history. Moreover, one cannot be completely sure of the absolutely accurate division of the sample into two parts: with and without hereditary burden, since medical documentation may contain inaccuracies, and patients reporting their anamnesis data may not know about the fact of the disease of relatives and specific diagnoses. Future research will aim to find genetic associations between the clinical picture of schizophrenia and its developmental trajectory using modern methods of genetic diagnostics.
Conclusions
In the present study, 48.1% of respondents had a family history of schizophrenia spectrum disorders within two generations (parents, grandparents, uncles, aunts, cousins, and siblings). A family history was associated with an earlier onset of schizophrenia (p=0.018) and higher scores on the CDSS scale (p=0.013).
These data may serve as a useful tool for a more effective diagnostic strategy in people with a high risk of schizophrenia due to a family history and for their further treatment. The results also highlight the importance of further research that aims to uncover the genetic mechanisms underlying this severe mental disorder.
References
1. Bleuler E. Dementia praecox or the group of schizophrenias. New York: International Universities Press.; 1950.
2. Fusar-Poli P, Politi P. Paul Eugen Bleuler and the birth of schizophrenia (1908). Am J Psychiatry. 2008;165(11):1407. https://doi.org/10.1176/appi.ajp.2008.08050714
3. Janoutová J, Janácková P, Serý O, Zeman T, Ambroz P, et al. Epidemiology and risk factors of schizophrenia. Neuro Endocrinol Lett. 2016;37(1):1-8. PMID: 26994378.
4. Sullivan PF, Kendler KS, Neale MC. Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Arch Gen Psychiatry. 2003;60(12):1187-1192. https://doi.org/10.1001/archpsyc.60.12.1187
5. Eyles DW. How do established developmental risk-factors for schizophrenia change the way the brain develops? Transl Psychiatry. 2021;11(1):158. https://doi.org/10.1038/s41398-021-01273-2
6. Mortensen PB, Pedersen MG, Pedersen CB. Psychiatric family history and schizophrenia risk in Denmark: which mental disorders are relevant? Psychol Med. 2010;40(2):201-210. https://doi.org/10.1017/S0033291709990419
7. Mortensen PB, Pedersen CB, Westergaard T, Wohlfahrt J, Ewald H, et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med. 1999;340(8):603-608. https://doi.org/10.1056/NEJM199902253400803
8. Kowalec K, Lu Y, Sariaslan A, Song J, Ploner A, et al. Increased schizophrenia family history burden and reduced premorbid IQ in treatment-resistant schizophrenia: a Swedish National Register and Genomic Study. Mol Psychiatry. 2021;26(8):4487-4495. https://doi.org/10.1038/s41380-019-0575-1
9. Esterberg ML, Trotman HD, Holtzman C, Compton MT, Walker EF. The impact of a family history of psychosis on ageat-onset and positive and negative symptoms of schizophrenia: a meta-analysis. Schizophr Res. 2010;120(1-3):121-130. https://doi.org/10.1016/j.schres.2010.01.011
10. Käkelä J, Panula J, Oinas E, Hirvonen N, Jääskeläinen E, Miettunen J. Family history of psychosis and social, occupational and global outcome in schizophrenia: a meta-analysis. Acta Psychiatr Scand. 2014;130(4):269-278. https://doi.org/10.1111/acps.12317
11. Ran MS, Xiao Y, Zhao X, Zhang TM, Yu YH, et al. Family history of psychosis and outcome of people with schizophrenia in rural China: 14-year follow-up study. Asian J Psychiatr. 2018;32:14-19. https://doi.org/10.1016/j.ajp.2017.11.016
12. Sullivan PF, Magnusson C, Reichenberg A, Boman M, Dalman C, et al. Family history of schizophrenia and bipolar disorder as risk factors for autism. Arch Gen Psychiatry. 2012;69(11):1099-1103. https://doi.org/10.1001/archgenpsychiatry.2012.730
13. Benros ME, Pedersen MG, Rasmussen H, Eaton WW, Nordentoft M, Mortensen PB. A nationwide study on the risk of autoimmune diseases in individuals with a personal or a family history of schizophrenia and related psychosis. Am J Psychiatry. 2014;171(2):218-226. https://doi.org/10.1176/appi.ajp.2013.13010086
14. Power RA, Verweij KJ, Zuhair M, Montgomery GW, Henders AK, et al. Genetic predisposition to schizophrenia associated with increased use of cannabis. Mol Psychiatry. 2014;19(11):1201-1204. https://doi.org/10.1038/mp.2014.51
15. van der Merwe C, Passchier R, Mufford M, Ramesar R, Dalvie S, Stein DJ. Polygenic risk for schizophrenia and associated brain structural changes: A systematic review. Compr Psychiatry. 2019;88:77-82. https://doi.org/10.1016/j.comppsych.2018.11.014
16. Mistry S, Harrison JR, Smith DJ, Escott-Price V, Zammit S. The use of polygenic risk scores to identify phenotypes associated with genetic risk of schizophrenia: Systematic review. Schizophr Res. 2018;197:2-8. https://doi.org/10.1016/j.schres.2017.10.037
17. Sultanova R.I., Gashkarimov V.R., Efremov I.S., Asadullin A.R. Clinical features in patients with depressive manifestations in schizophrenia. Psikhicheskoe zdorovie [Mental Health]. 2023;18(7):11-20. (In Russ.). eLIBRARY ID: 48663067 EDN: FPBXVD
18. Sultanova R.I., Gashkarimov V.R., Efremov I.S., Gizatullin T.R., Asadullin A.R. Association of depressive manifestations with the severity of psychopathological symptoms in people with schizophrenia. Psikhicheskoe zdorovie [Mental Health]. 2022;17(4):26-32. (In Russ.). eLIBRARY ID: 48663067 EDN: FPBXVD
19. Buleyko A.A., Soldatkin V.A. Impact of alcohol abuse on suicide risk in schizophrenic patients. S.S. Korsakov Journal of Neurology and Psychiatry. 2021;121(10):144-148. (In Russ.) https://doi.org/10.17116/jnevro2021121101144
20. Peitl V, Štefanović M, Karlović D. Depressive symptoms in schizophrenia and dopamine and serotonin gene polymorphisms. Prog Neuropsychopharmacol Biol Psychiatry. 2017;77:209-215. https://doi.org/10.1016/j.pnpbp.2017.04.011
21. Chen J, Wang M, Waheed Khan RA, He K, Wang Q, et al. The GSK3B gene confers risk for both major depressive disorder and schizophrenia in the Han Chinese population. J Affect Disord. 2015;185:149-155. Erratum in: J Affect Disord. 2017;221:267. https://doi.org/10.1016/j.jad.2015.06.040
22. Wang Q, He K, Li Z, Chen J, Li W, Wen Z, et al. The CMYA5 gene confers risk for both schizophrenia and major depressive disorder in the Han Chinese population. World J Biol Psychiatry. 2014;15(7):553-560. https://doi.org/10.3109/15622975.2014.915057
23. Li W, Ju K, Li Z, He K, Chen J, et al. Significant association of GRM7 and GRM8 genes with schizophrenia and major depressive disorder in the Han Chinese population. Eur Neuropsychopharmacol. 2016;26(1):136-146. https://doi.org/10.1016/j.euroneuro.2015.05.004
24. Wen Z, Chen J, Khan RA, Song Z, Wang M, et al. Genetic association between NRG1 and schizophrenia, major depressive disorder, bipolar disorder in Han Chinese population. Am J Med Genet B Neuropsychiatr Genet. 2016;171B(3):468-478. https://doi.org/10.1002/ajmg.b.32428
25. He K, An Z, Wang Q, Li T, Li Z, et al. CACNA1C, schizophrenia and major depressive disorder in the Han Chinese population. Br J Psychiatry. 2014;204(1):36-39. https://doi.org/10.1192/bjp.bp.113.126979
About the Authors
V. R. GashkarimovRussian Federation
Vadim R. Gashkarimov, psychiatrist
Ufa
R. I. Sultanova
Russian Federation
Renata I. Sultanova, psychiatrist
Moscow
I. S. Efremov
Russian Federation
Ilya S. Efremov, Cand. Sci. (Med.), Deputy Director of the Center for Molecular medicine;
Researcher
Ufa;
Saint-Petersburg
I. E. Sabanaeva
Russian Federation
Ilina E. Sabanaeva, 5th year student
Ufa
A. A. Iskhakov
Russian Federation
Anatoliy A. Iskhakov, clinical resident-psychiatrist, Department of Psychiatry Narcology and Psychotherapy
Ufa
L. R. Bakirov
Russian Federation
Linar R. Bakirov, psychiatrist;
assistant professor, Department of Psychiatry, Narcology and Psychotherapy
Ufa
A. R. Asadullin
Russian Federation
Azat R. Asadullin, Dr. Sci. (Med.), Professor, Department of Psychiatry, Narcology and Psychotherapy;
Director of the Center for Molecular medicine;
Leading Researcher;
Professor, Department of Psychiatry, Narcology, Psychotherapy and clinical psychology
Ufa;
Saint-Petersburg;
Saratov
Review
For citations:
Gashkarimov V.R., Sultanova R.I., Efremov I.S., Sabanaeva I.E., Iskhakov A.A., Bakirov L.R., Asadullin A.R. The influence of family history of schizophrenic spectrum disorders on the clinical presentation of schizophrenia. Medical Herald of the South of Russia. 2024;15(3):26-32. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-3-26-32






































