Scroll to:
The problem of comorbidity in patients with HIV infection and hepatic cirrhosis in the intensive care unit
https://doi.org/10.21886/2219-8075-2024-15-3-82-89
Abstract
Objective: clinical and laboratory assessment of HIV-infected patients in the intensive care unit with liver cirrhosis that developed as a result of hepatitis of various etiologies.
Materials and methods: a retrospective assessment of 91 medical records of patients with hepatic cirrhosis among 494 HIV-infected patients in the intensive care unit (ICU) was carried out in order to describe the clinical and laboratory features of the course of liver pathology against the background of HIV infection with secondary diseases. The subjects under observation were 46 (50.5%) men, 45 (49.5%) women, median age — 41 years.
Results: patients were diagnosed with profound immunodeficiency (CD4+ lymphocyte count 100,000 copies of HIV RNA per 1 ml — in 45.1% of patients). Child-Pugh class C hepatic cirrhosis was diagnosed in 72.5% of patients. Cirrhosis in most cases developed as a result of toxic hepatitis in combination with chronic hepatitis C (CHC). More than half of the patients showed clinical and laboratory signs of decompensated hepatic cirrhosis. Combinations of two to five secondary infections were diagnosed in 52.8% of patients. The structure of secondary diseases was dominated by bacterial pneumonia, encephalitis and visceral candidiasis. 75.8% of patients did not receive ART, all patients did not receive antiviral therapy for chronic hepatitis.
Conclusion: the mortality rate of patients with decompensated liver cirrhosis in the intensive care unit was 80.2% and was associated with the number of secondary diseases and the lack of antiretroviral therapy. Patients with a combination of HIV infection and viral hepatitis require earlier diagnosis and prescription of etiotropic therapy.
For citations:
Burdova E.Yu., Voznesenskiy S.L., Samotolkina E.S., Ermak T.N., Klimkova P.V., Korneva I.A. The problem of comorbidity in patients with HIV infection and hepatic cirrhosis in the intensive care unit. Medical Herald of the South of Russia. 2024;15(3):83-89. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-3-82-89
Introduction
As of December 31, 2022, 1,168,076 Russians with a laboratory-confirmed diagnosis of HIV infection lived in the Russian Federation. In 2022, 63,150 new cases of HIV infection identified by immune blot were reported (according to preliminary data), excluding those identified anonymously and in foreign citizens. The death of 34,410 Russians infected with HIV was reported. Since HIV infection is an incurable disease, and the number of new HIV infections exceeds the number of deaths, the total number of Russians living with HIV continues to grow1. In patients with HIV infection, one of the leading causes of hospitalization and mortality are liver diseases and their complications [1]. Taking into account the general routes of transmission with HIV, parenteral viral hepatitis occupies a significant proportion of the liver pathology which occurs with varying severity and leads to cirrhosis, thereby worsening the prognosis of the underlying disease. Due to the continuing relevance of the injection route of infection with parenteral infections of people who consume psychoactive substances, viral hepatitis C occupies a significant place in a number of co-infections [2][3]. According to a number of studies, chronic viral hepatitis C is associated with HIV in more than half of cases in the Russian Federation [4][5]. Despite the modern possibilities of etiotropic therapy for hepatitis C, many patients do not receive treatment due to alcohol abuse, taking psychoactive substances, low immune status, and the patient's refusal of treatment [6]. Hepatitis B is also often diagnosed in patients with HIV, and it is more severe in this group [7]. According to WHO, more than 70% of HIV-infected people have serological markers of current or previous viral hepatitis B [7][8]. In addition, chronic hepatitis with liver cirrhosis progresses faster with co-infection of hepatitis and HIV [9]. According to the studies, liver cirrhosis develops faster and 3 times more often in patients with HIV than in patients with hepatitis C mono-infection [10]. The mutually differentiating effect of the hepatitis C virus and HIV also affects the course of HIV infection in addition to accelerating the progression of liver damage. For example, a high HCV RNA viral load accelerates the progression of HIV [11]. Thus, the problem of liver pathology is relevant for patients with HIV at all its stages.
The leading cause of death in patients with advanced HIV is the presence of severe comorbid variants, which include a combination of HIV infection and chronic viral hepatitis in the cirrhotic stage [2][12]. Complications associated with liver disease were the most common cause of death (14.5%), not directly associated with HIV infection and opportunistic lesions, according to a cohort study [13]. Most of the patients were diagnosed with hepatitis C, hepatitis B, and co-infection B + C. An association between immunodeficiency and the risk of death from liver lesions was also identified [13]. Mortality from liver disease accounted for 13% of total deaths in another large European cohort study examining HIV infection. This indicator also ranks second after death from AIDS-associated diseases [1][14].
At the same time, the treatment of HIV in patients with decompensated cirrhosis requires a decrease in the dosage of antiretroviral drugs due to deterioration in drug metabolism [15]. The presence of clinically pronounced liver cirrhosis is an absolute indication for the treatment of chronic hepatitis B. At compensated liver cirrhosis, there are no contraindications to the use of any drugs. In the case of decompensated liver cirrhosis, treatment of chronic hepatitis B should be long, most likely lifelong, since increased viral replication after stopping treatment can lead to rapid clinical deterioration [16]. CHC therapy is indicated for all patients with HIV who have HCV replication (HCV RNA) [17]. Moreover, the presence of secondary diseases in the later stages of HIV is an absolute contraindication for liver transplantation2. Another problem that doctors face when treating combined pathology is the potential hepatotoxic effect of many antiretroviral drugs, which is combined with the existing liver damage [18]. Further study of the effect of antiretroviral therapy (ART) on the course of chronic liver pathology is necessary [19], since several studies have shown that patients with HCV and/or HBV co-infection had a greater risk of severe hepatotoxic effects of ART [19][20]. In addition to ART, patients in advanced stages of HIV require treatment for secondary/opportunistic diseases, which currently often occur in combination with each other [21][22]. Such patients need inpatient care, including in intensive care units (ICUs). An ICU for HIV-infected patients has been deployed in Infectious Clinical Hospital No. 2 in Moscow since 2014. Patients in a serious condition with a complicated course of opportunistic infections and concomitant pathology, a significant part of which is liver damage of various etiologies, are treated in this intensive care unit [23]. The treatment of such patients is extremely difficult in terms of prognosis.
The purpose of the study is a clinical and laboratory assessment of HIV-infected patients in the ICU with cirrhosis of the liver, which developed as a result of hepatitis of various etiologies.
Materials and methods
A retrospective analysis of the case histories of 494 patients with HIV infection who were in the ICU of Infectious Clinical Hospital No. 2 in Moscow (ICH No. 2) in 2020 was carried out, of which hepatitis of various etiologies was diagnosed in 294 (59.5%). Liver cirrhosis was diagnosed in 91 (18.4%) patients. Examination and treatment of patients were carried out on the basis of current clinical guidelines for the treatment of HIV and related diseases [24]. Diagnosis of liver diseases and secondary diseases was carried out on the basis of a set of anamnestic, clinical laboratory, and instrumental data. To assess pathological processes, liver function, and severity of the patient's condition, routine laboratory diagnostic methods were used: biochemical blood test and analysis of the blood coagulation system. Hepatic dysfunction was assessed using the Child-Pugh scale. To verify secondary diseases, a set of methods was used, including bacteriological, serological, and molecular biological studies of various biological substrates using test systems produced by the Central Research Institute of Epidemiology of Rospotrebnadzor, as well as Abbott and Roche. To assess the depth of immunodeficiency, the parameters of cellular immunity, including the number of CD4 + lymphocytes, were determined. For the determination of the HIV viral load, the polymerase chain reaction was used. The data are presented as median and interquartile range (25th-75th percentile), minimum and maximum values. The statistical significance of the differences (p) in quantitative values between independent groups was assessed by analyzing arbitrary conjugacy tables using the Chi-square test. Differences between groups were considered statistically significant at the probability of the fairness of the null hypothesis that there was no difference between groups (p) < 0.05.
Results
The medical history of patients with HIV and liver cirrhosis as an outcome of hepatitis of various etiologies was studied, their number was 91 people. The median age was 41, the age of patients was from 26 to 62, 46 (50.5%) men, 45 (49.5%) women. The duration of diagnosed HIV, based on the immune blot date, ranged from 1 (positive immune blot was first determined during the current hospitalization) to 7950 days. The median was 1950 days (5 years). The route of infection with HIV in 40 (44%) patients was declared as artificial, in 5 (5.5%) patients – sexual, and in 46 (50.5%) patients, it was not clear. CD4 + lymphocytes < 100 cells/µL were in 37.4%, 101–200 cells/µL were in 17.6%, 201–350 cells/µL were in 15.4%, 350–500 cells/µL were in 9.8%, and more than 500 cells/µL were in 3.3% of patients. The number of HIV RNA copies in 1 ml (viral load) was < 20 copies in 9.9%, 21–1000 copies – in 9.9%, 1001–100,000 copies – in 18.7%, and > 100,000 copies – in 45.1% of patients. Prior to this hospitalization, 75.8% of patients did not take ART or discontinued ART on their own, 23.1% received ART, and 1.1% of patients were prescribed ART in the department. The prehospital period was 1–7 days in 21 (23.1%) patients, 8–30 days in 26 (28.6%) patients, 31–60 days in 17 (18.7%) patients, and more than 60 days in 8 (8.8%) patients. In 19 (20.8%) patients, data on the period of the disease before hospitalization were not obtained. The structure of liver diseases in patients with cirrhosis is represented by the following conditions: chronic hepatitis C (CHC) in combination with toxic hepatitis – in 56 (61.5%) patients, toxic hepatitis in 19 (20.9%) patients, CHC – in 12 (13.2%) patients, chronic hepatitis B (CHB) – in 1 (1%) patient, CHC in combination with CHB, CHD, and toxic hepatitis – in 1 (1%) patient. In 2 (2.2%) patients, the etiology of liver damage could not be determined. According to Child-Pugh classification, cirrhosis was represented by the following classes: class A – in 5 (5.5% of patients), class B – in 13 (14.3%) patients, class C – in 66 (72.5%) patients; in 7 (7.7%) patients, the cirrhosis class was not specified. No patient had a history of etiotropic therapy for viral hepatitis. The duration of hospitalization in the ICU ranged from 0 to 89 days; the median was 7 days. The outcome of hospitalization in the study group in 73 (80.2%) cases was fatal, 14 (15.4%) people were discharged or transferred to specialized therapeutic departments with improvement, and 4 (4.4%) people were discharged of their own free will or transferred to specialized therapeutic departments without improvement.
All patients during their stay in the ICU were in serious condition due to both secondary diseases and liver pathology. Symptoms of jaundice syndrome, severe intoxication, impaired consciousness, and instability of hemodynamics were recorded in patients. An analysis of clinical manifestations, such as encephalopathy, edema-ascitic and hemorrhagic syndromes, which are markers of severe liver cirrhosis, showed that a severe course was dominant. Despite the possible polyetiological genesis of encephalopathy, it was reported in 65.9% of cases. The incidence of hemorrhagic syndrome was 53.8%. Edematous ascitic syndrome was diagnosed in 38.5% of cases.
Laboratory data were characterized by the presence of cytolysis and hepatic cell failure. The results of the investigation of metabolic, immunological, and virological parameters are presented in Table 1.
Таблица / Table 1
Лабораторные показатели больных ВИЧ-инфекцией с циррозом печени (n=91)
Laboratory parameters of patients with HIV infection with hepatic cirrhosis (n=91)
|
Показатель Index
|
Медиана Median |
Минимум Minimum |
Максимум Maximum |
25,75 перцентиль 25.75 percentile |
|
АЛТ, Ед/л ALT, U/l |
38,2 |
7,6 |
690 |
20-79,95 |
|
АСТ, Ед/л AST, U/l |
106 |
15 |
1610 |
51,3-217 |
|
Билирубин, мкмоль/л Bilirubin, µmol/l |
55,3 |
2,9 |
454,5 |
21,35-155,2 |
|
Альбумин, г/л Albumin, g/l |
20,4 |
12,3 |
34,6 |
18-25 |
|
ПТИ, % PTI, % |
37,6 |
6,6 |
102 |
26,1-52,5 |
|
Количество CD4+ лимфоцитов, кл/мкл Number of CD4+ lymphocytes, cells/µl |
115 |
0 |
972 |
46,5-242 |
|
Количество копий РНК ВИЧ в мл Number of HIV RNA copies per ml |
141034 |
0 |
10000000 |
2761-642478,5 |
The course of the disease was characterized not only by liver damage, but also by the presence of combined opportunistic infections, which was the reason for both the aggravation of the patient's condition and the atypical clinical picture. Bacterial pneumonia, encephalitis, and visceral candidiasis prevailed in the spectrum of combined secondary pathology. HIV wasting syndrome was reported in 20% of patients. Data on the structure of secondary pathology are presented in Table 2.
Таблица / Table 2
Структура вторичных заболеваний у больных ВИЧ-инфекцией и циррозом печени (n=91)
Structure of secondary diseases in patients with HIV infection and hepatic cirrhosis (n=91)
|
Заболевание Disease |
Абс. (%) Abs. (%) |
|
Бактериальная пневмония Bacterial pneumonia |
69 (75,9) |
|
Энцефалит неуточненной этиологии Encephalitis of unspecified etiology |
24 (26,4) |
|
Кахексия Cachexia |
18 (19,8) |
|
Кандидоз пищевода Candidiasis of the esophagus |
14 (15,4) |
|
Кандидоз лёгких Pulmonary candidiasis |
12 (13,2) |
|
ЦМВ-инфекция CMV infection |
10 (11, 0) |
|
Пневмоцистная пневмония Pneumocystis pneumonia |
4 (4,4) |
|
Церебральный токсоплазмоз Cerebral toxoplasmosis |
2 (2,2) |
|
Прогрессирующая многоочаговая лейкоэнцефалопатия Progressive multifocal leukoencephalopathy |
2 (2,2) |
|
Лимфома Беркитта Burkitt's lymphoma |
1 (1,0) |
However, the description of the structure of secondary diseases does not fully reflect the clinical picture of the disease. In 10.9% of patients, the severity of the condition was due to manifestations of liver cirrhosis. Thirty-three patients (36.3%) were diagnosed with one opportunistic infection, and 52.8% had 2 to 5 secondary diseases in addition to liver damage with an outcome of cirrhosis (Table 3).
Таблица / Table 3
Количество сочетанных вторичных заболеваний
Number of combined secondary diseases
|
Количество вторичных заболеваний Number of secondary diseases |
Абс. (%) Abs. (%) |
|
0 |
10 (10,9) |
|
1 |
33 (36,3) |
|
2 |
29 (31,9) |
|
3 |
12 (13,2) |
|
4 |
5 (5,5) |
|
5 |
2 (2,2) |
We analyzed the outcome of the disease in patients with liver cirrhosis depending on the number of combined secondary diseases. According to the clinical conclusion, the cause of death in 52 (71.2%) patients out of 73 deaths was multiple organ failure, in 8 (11%) patients – cerebral edema, in 3 (4.1%) patients – acute heart failure, and in 2 (2.7%) patients – acute liver failure. In 8 (11%) patients, the cause of death has not been established. Statistically significant differences in the frequency of favorable and fatal outcomes were obtained. So, in the absence of secondary concomitant diseases, 60% of patients survived, but already in the presence of one secondary lesion, the frequency of a favorable outcome decreased to 15.2%, in the presence of 2 and 3 combined opportunistic infections, the risk of death increased, and in 4 and 5 secondary diseases, death occurred in all patients (the critical value of χ2 at the level of significance p = 0.01 is 15.086, the relationship between the number of combined secondary diseases and the incidence of disease outcome is statistically significant at the level of significance p < 0.01) (Fig. 1).
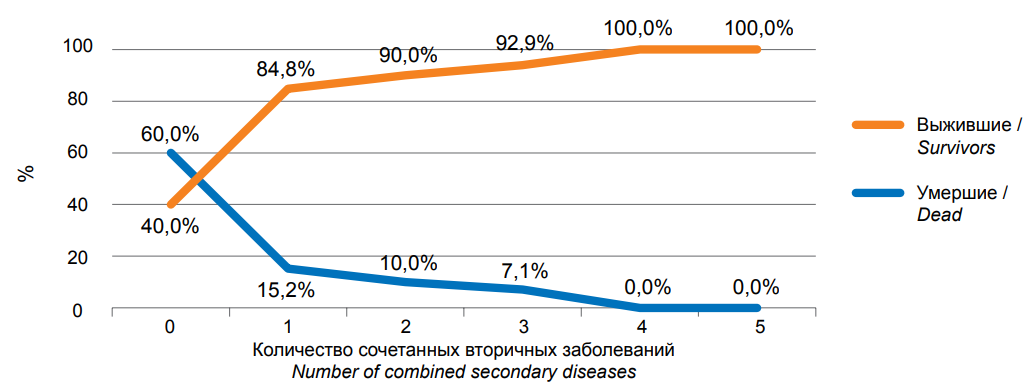
Рисунок. 1. Связь исходов болезни у больных ВИЧ-инфекцией и циррозом печени при различном количестве вторичных заболеваний (n=91)
Figure. 1. Relationship between disease outcomes in patients with HIV infection and liver cirrhosis with varying numbers of secondary diseases (n=91)
Discussion
The proportion of HIV patients with liver damage was 59.5%. Liver cirrhosis as an outcome of hepatitis of various etiologies was 18.4%; Child-Pugh class C was established in 13.4% of the total number of patients. Consequently, this is the proportion of patients requiring immediate antiviral therapy for chronic viral hepatitis, but at the same time 55% of patients with cirrhosis had severe immunodeficiency (CD4 cell count less than 200 per μl) and 45.1% had a high HIV viral load (more than 100,000 copies/ml), which is associated with the lack of ART in 75.8% of patients. Only 10.9% of patients with liver cirrhosis did not have secondary diseases, and in this group, the proportion of survivors was maximum – 60%. More than half (52.8%) of patients were diagnosed with combined secondary diseases; with an increase in their number, the proportion of deaths increased statistically significantly, and with 4–5 secondary diseases, death occurred. Bacterial pneumonia, encephalitis of unspecified etiology, CMV infection, and visceral candidiasis were diagnosed more often than others. Such patients need to be prescribed appropriate etiotropic therapy, including antifungal and broad-spectrum antibacterial drugs with hepatotoxicity, which cannot but affect the condition of patients with cirrhosis.
Conclusion
To improve the survival prognosis of patients in serious condition, it is necessary to take into account the problem of combined secondary and concomitant diseases, including liver lesions, timely prescribe ART and treatment of concomitant lesions at the prehospital stage.
1. Reference HIV in Russia 31.12.2022. Moscow. Specialized Research Department for the Prevention and Control of AIDS FBUN of the Central Research Institute of Epidemiology of Rospotrebnadzor. 2023. URL: http://www.hivrussia.info/wp-content/uploads/2023/09/Spravka-VICH-v-Rossii-na-31.12.2022.pdf
2. Gauthier SV, et al. Liver transplantation. National Guidelines 2013; 9. URL:https://transpl.ru/images/cms/data/pdf/nacional_nye_klinicheskie_rekomendacii_po_transplantacii_pecheni.pdf?ysclid=l3cpfn14d2
References
1. Yushchuk N.D., Znoyko O.O., Safiullina N.Kh., Ivannikov E.V., Aristambekova M.S. Elastometry in complex assessment of hepatic fibrosis in patients with HIV and HIV/VHC coinfected patients. Infectious Diseases: News. Opinions. Education. 2014;2(7):84-88. (In Russ.) eLIBRARY ID: 21857031 EDN: SKHSWJ
2. Leonova O.N., Stepanova Ye.V., Belyakov N.A. Severe and comorbid conditions in HIV patients: an analysis of adverse outcomes. HIV Infection and Immunosuppressive Disorders. 2017;9(1):55-64. (In Russ.) https://doi.org/10.22328/2077-9828-2017-9-1-55-64
3. Belyakova N.A., Rassokhina V.V., Stepanova E.V., eds. HIV infection, secondary and concomitant diseases: Medical thematic archive. St. Petersburg: Baltic Medical Education Center; 2014. (In Russ.)
4. Manapova E.R., Fazylov V.Kh., Tkacheva S.V. Clinical and pathogenetic significance of alanine aminotransferase activity in co-infection with HIV/HCV and HIV infection. Infectious diseases: news, opinions, training. 2019;8(3):14-20. (In Russ.) eLIBRARY ID: 40953116 EDN: TFKSRB
5. Kravchenko A.V., Gankina N.Yu., Kanestri V.G. Features of antiretroviral therapy in combination of HIV infection and chronic viral hepatitis. Pharmateka. 2008;(19):10-18. (In Russ.) eLIBRARY ID: 11931067 EDN: KBCHBX
6. Sundukov A.V., Melnikov L.V., Evdokimov E.Yu. Characteristics of patients with chronic hepatitis C and HIV infection. breast cancer. Medical review. 2018;2(7(II)):64-67. (In Russ.) eLIBRARY ID: 36907222 EDN: YWCXWH
7. Thio CL. Hepatitis B in the human immunodeficiency virusinfected patient: epidemiology, natural history, and treatment. Semin Liver Dis. 2003;23(2):125-136. https://doi.org/10.1055/s-2003-39951
8. World Health Organization. Hepatitis B. Geneva, WHO; 2002.
9. Kravchenko A.V., Maksimov S.L. Antiretroviral therapy and therapy of chronic hepatitis с in HIV-infected patients. Infectious diseases: news, opinions, training. 2014;1(6):70-76 (In Russ.) eLIBRARY ID: 21498597 EDN: SCLUPD
10. Soriano V, Sulkowski M, Bergin C, Hatzakis A, Cacoub P, et al. Care of patients with chronic hepatitis C and HIV co-infection: recommendations from the HIV-HCV International Panel. AIDS. 2002;16(6):813-828. https://doi.org/10.1097/00002030-200204120-00001
11. Zheenalieva G.M., Kanatbekova A.K., Abdikerimova M.M., Abdikerimov M.M., Zholdoshev S.T. Chronic hepatitis C and HIV infection. International Journal of Applied and Basic Research. 2021;(6):57-62. (In Russ.) https://doi.org/10.17513/mjpfi.13231
12. eLIBRARY ID: 21537582 EDN: SDHZHJ
13. Weber R, Sabin CA, Friis-Møller N, Reiss P, El-Sadr WM, et al. Liver-related deaths in persons infected with the human immunodeficiency virus: the D:A:D study. Arch Intern Med. 2006;166(15):1632-1641. https://doi.org/10.1001/archinte.166.15.1632. PMID: 16908797.
14. Smith CJ, Ryom L, Weber R, Morlat P, Pradier C, et al. Trends in underlying causes of death in people with HIV from 1999 to 2011 (D:A:D): a multicohort collaboration. Lancet. 2014;384(9939):241-248. https://doi.org/10.1016/S0140-6736(14)60604-8
15. Pokrovsky V.V., ed. HIV infection and AIDS: national guidelines. Moscow: GEOTAR-Media; 2013. (In Russ.)
16. Kravchenko A.V., Gankina N.Yu., Kanestri V.G., Maksimov S.L. Tactics of treatment of chronic hepatitis B in patients with HIV infection. Infectious diseases. 2008;6(2):88-95. (In Russ.) eLIBRARY ID: 11148784 EDN: JJZEVV
17. Kravchenko A.V. Kanestri V.G. The hepatitis C virus protease inhibitor telaprevir in therapy regimens for chronic hepatitis C in patients with hiv infection. Epidemiology and infectious diseases. Topical issues. 2013;(2):68-72. (In Russ.) eLIBRARY ID: 19049270 EDN: QAWFYH
18. Sulkowski MS, Thomas DL, Mehta SH, Chaisson RE, Moore RD. Hepatotoxicity associated with nevirapine or efavirenz-containing antiretroviral therapy: role of hepatitis C and B infections. Hepatology. 2002;35(1):182-189. https://doi.org/10.1053/jhep.2002.30319
19. Sulkowski MS, Thomas DL, Chaisson RE, Moore RD. Hepatotoxicity associated with antiretroviral therapy in adults infected with human immunodeficiency virus and the role of hepatitis C or B virus infection. JAMA. 2000;283(1):74-80. https://doi.org/10.1001/jama.283.1.74
20. den Brinker M, Wit FW, Wertheim-van Dillen PM, Jurriaans S, Weel J, et al. Hepatitis B and C virus co-infection and the risk for hepatotoxicity of highly active antiretroviral therapy in HIV-1 infection. AIDS. 2000;14(18):2895-2902. https://doi.org/10.1097/00002030-200012220-00011
21. Volchkova E.V., Lunchenkov N.Yu., Kanshina N.N. Risk factors for toxoplasmosis infection reactivation in HIV-infected patients. International research journal. 2014;(8):34-36. (In Russ.) eLIBRARY ID: 21994896 EDN: SNIEHJ
22. Shkarin V.V., Saperkin N.V. Epidemiological features of combined opportunistic infections (review). Medical almanac. 2017;4(49):22-28. (In Russ.) eLIBRARY ID: 30114665 EDN: ZIZZFL
23. Kozhevnikova G.M., Voznesenskiy S.L., Ermak T.N., Smetanina S.V., Petrova E.V., Samotolkina E.A. Prognostic factors of a favourable outcome of treating HIV-infected patients in an intensive care unit. Infekc. bolezni (Infectious diseases). 2017;15(3):20–24. (In Russ.). https://doi.org/10.20953/1729-9225-2017-3-20-24
24. Pokrovsky V.V., Yurin O.G., Kravchenko A.V., Belyaeva V.V., Buravtsova V.V., Deulina M.O., et al. Recommendations for the treatment of HIV infection and related diseases, chemoprevention of HIV infection. Epidemiol. infectious illness. Actual. Question. 2022;12(4S1):1-107. (In Russ.) eLIBRARY ID: 44812014 EDN: SMISQQ
About the Authors
E. Yu. BurdovaElena Yu. Burdova, assistant Professor of the Department of Infectious Diseases, Epidemiology and Phthisiology
Moscow
S. L. Voznesenskiy
Russian Federation
Sergey L. Voznesenskiy, MD, PhD, associate Professor of the Department of Infectious Diseases, Epidemiology, and Phthisiology, Medical Institute
Moscow
E. S. Samotolkina
Elena S. Samotolkina, infectious diseases specialist of the intensive care unit for patients with HIV infection
Moscow
T. N. Ermak
Tatiana N. Ermak, Dr. Sci. (Med.), leading researcher
Moscow
P. V. Klimkova
Klimkova V. Polina, infectious diseases specialist of the intensive care unit for patients with HIV infection
Moscow
I. A. Korneva
Irina A. Korneva, infectious diseases specialist of the intensive care unit for patients with HIV infection
Moscow
Review
For citations:
Burdova E.Yu., Voznesenskiy S.L., Samotolkina E.S., Ermak T.N., Klimkova P.V., Korneva I.A. The problem of comorbidity in patients with HIV infection and hepatic cirrhosis in the intensive care unit. Medical Herald of the South of Russia. 2024;15(3):83-89. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-3-82-89







































