Scroll to:
Ten years’ experience of vacuum systems in treatment of complicated postoperative wounds of various etiologies
https://doi.org/10.21886/2219-8075-2024-15-3-106-114
Abstract
Objective: increase effectiveness of wounds treatment after various etiology by using VAC.
Materials and methods: study included 128 patients with surgical infection. Specter of operations is presented: pilonidal cyst excision — 40 (31.2%), sternomediastinitis — 23 (18%), mesh hernioplasty — 16 (12.5%), laparotomy — 15 (11.7%), emergency laparotomy — 7 (5.5%), traumatology paraimplant complications — 7 (5.5%), abdominoplasty — 7 (5.5%), postoperative esophageal fistulas — 6 (4.7%), decubital ulcers — 4 (3.1%), mammoplasty — 3 (2.3%).
Results: duration of VAC-therapy averaged 22.1±0.26 days. Systemic inflammatory reaction noted in 43 (33.6%) patients. Granulation tissue on 8th day of treatment noted in 98 (76.6%) cases. Microscopically, on day 8 of treatment, inflammatory-regenerative cytograms were detected in 104 (81.3%) patients. Over the course of 16 days, wounds decreased by 62.1±2.5% in all observations. In 47 (36.7%) cases, secondary sutures were applied, in 30 (23.4%) — grafting. A month later, healing was noted in 106 (82.8%) patients. Complications (wound bleeding) were noted in 7 (5.5%) patients. Reoperations were performed in 11 (8.5%) patients. Period of complete healing was 29.3±0.4 days.
Conclusions: vacuum therapy is an effective way to treat wounds in purulent surgery. Time of complete reparative regeneration of wound and period of expensive inpatient treatment are reduced.
Keywords
For citations:
Cherkasov M.F., Galashokyan K.M., Startsev Yu.M., Cherkasov D.M., Melikova S.G., Rudkova K.E. Ten years’ experience of vacuum systems in treatment of complicated postoperative wounds of various etiologies. Medical Herald of the South of Russia. 2024;15(3):106-114. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-3-106-114
Introduction
Surgical operations are accompanied by dissection of the integumentary tissues, while purulent-inflammatory diseases occur in more than a third of cases. Infection in surgery is relevant at the current stage of active development of reconstructive, plastic, and military field surgery.
Currently, there is an increase in the number of operations and resistance of microorganisms, as a result of which the infection of the surgical area is characterized by a complicated course that is difficult to respond to standard treatment [1].
Despite the use of modern achievements of aseptics and antiseptics, the development of purulent infection is an important problem at the junction of various surgical specialties in a multidisciplinary hospital [2]. In operations with contaminated wounds, the frequency of suppuration is 5–15% of cases, which requires the introduction of effective methods of treatment. The contingent of comorbid patients with obesity, diabetes mellitus, immunodeficiency, and cancer is increasing annually. In comorbid patients, surgical infection is detected more often, reaching 20–25%, and the postoperative period is often complicated by sepsis and multiple organ failure with a fatal outcome [3]. The incidence of infectious complications in all wounded in modern armed conflicts is 19.2%, and local infection occurs in 72.2% of cases [4]. At present, combat surgical pathology has a characteristic feature for wars of a new type: combined thermomechanical wounds, up to 90% of gunshot wounds are associated with the use of explosive ammunition, and only 10% with small arms, which increases the frequency of suppuration of wounds [5].
In purulent surgery, the search for mechanisms of influence on the reparative regeneration of purulent wounds continues intensively and the method of treatment in conditions of controlled negative pressure occupies a special place. Now vacuum therapy is a standard that complements the surgical treatment of the purulent focus, complex antibacterial therapy, and rehabilitation [6, 7].
Many beneficial effects of vacuum therapy on reparative regeneration have been detailed in the scientific literature: exudate removal, maintenance of optimal humidity under the wound dressing, reduction of bacterial load, improvement of blood flow and lymph flow, reduction of interstitial fluid, and wound contraction [8].
Application principles of vacuum therapy in purulent surgery have been known for a long time. For example, Professor N.N. Kanshin intensively developed methods for active drainage of abscesses of various etiologies using vacuum aspirators of various designs [9]. As medical technology developed, various devices for vacuum treatment of wounds appeared.
Over the past two decades, purulent surgery has been looking for ways to influence the regeneration of the wound process, among which the vacuum therapy technique is currently leading. Currently, it is difficult to find such a field of surgery, where the method of active exudate aspiration is not used [10].
The purpose of the study is to increase the effectiveness of the treatment of wounds formed after various surgical operations by using negative pressure systems.
Materials and methods
This study is prospective and presents the experience of treating patients with postoperative wounds of various origins from July 2013 to December 2023. The study included patients of both sexes from 18 years of age who were diagnosed with surgical site infection and soft tissue infection. Subjects who received vacuum therapy with voluntary consent were included. Subjects under 18 years of age without surgical complications who did not receive vacuum therapy and who discontinued the study were excluded.
The study was carried out within the dissertation work "Vacuum therapy in the treatment of the epithelial coccygeal passage", as well as the State assignment for the implementation of applied scientific research devoted to the use of vacuum therapy in the treatment of purulent wounds of various etiologies No.: AAAA-A16-116101410046-3 dated December 1, 2017 (deadlines 2018–2020). The work complied with the standards of the Helsinki Declaration and was approved by an independent meeting of the local ethics committee of the Rostov State Medical University, protocol No. 16/13 of November 14, 2013. All persons participating in the study signed informed voluntary consent for participation in the study and publishing their health data.
The experience of treating 128 patients with surgical site infections treated with vacuum therapy is presented. The study was performed at the Surgical Center of the Rostov State Medical University Clinic, as well as at the Department of Purulent Surgery of Regional Clinical Hospital No. 2.
Among the patients included in the clinical study, there were 88 (68.8%) men and 40 (31.2%) women. The average age of men was 47.9 ± 2.2 years, and the average age of women was 52.3 ± 2.7.
Comorbidity was detected in 59 (46.1%) patients. Diabetes mellitus was detected in 42 (32.8%) patients, obesity – in 93 (72.6%), chronic heart failure – in 75 (58.6%), and chronic renal failure was detected in 15 (11.7%).
After standard additional examination and preoperative preparation, the patients underwent complex treatment with negative pressure therapy; the distribution of patients is presented in Table 1.
Таблица / Table 1
Распределение больных по характеру оперативных вмешательств
Distribution of patients by the type of surgical operation
|
Характер операции Type of surgical operation |
Число больных, n (%) Number of patients n (%) |
|
|
Иссечения эпителиального копчикового хода Excision of pilonidal sinus |
40 (31,2) |
|
|
Стерномедиастинит Sternomediastinitis |
23 (18) |
|
|
Герниопластика с эксплантом Hernioplasty with mesh |
16 (12,5) |
|
|
Плановая лапаротомия Common laparotomy |
15 (11,7) |
|
|
Экстренная лапаротомия Emergency laparotomy |
7 (5,5) |
|
|
Параимплантные осложнения в травматологии Paraimplant complications in traumatology |
7 (5,5) |
|
|
Аутогерниопластика, абдоминопластика Autohernioplasty, abdominoplasty |
7 (5,5) |
|
|
Послеоперационные пищеводные свищи Postoperative esophageal fistulas |
6 (4,7) |
|
|
Декубитальные язвы Decubital ulcers |
4 (3,1) |
|
|
Маммопластика Mammoplasty |
3 (2,3) |
|
|
Всего Total |
128 |
|
The program of complex treatment of patients consisted of surgical processing of infection and dressings with removal of non-viable tissues. Therapy of comorbid, dysmetabolic disorders, broad-spectrum antibacterial therapy, and etiotropic therapy was performed upon receipt of microbiological study results. Vacuum therapy was carried out using various developed methods of treatment with negative pressure, depending on the type of previous operation and the phase of the wound process.
During the study, we used various certified vacuum therapy systems and consumables: Suprasorb CNP 1 (Lohmann & Rauscher, Germany), VACFreedom (KCI, USA), ATMOS S042 VivanoTec (Medicine Technik, Germany), and portable devices for negative pressure wound therapy PICO (Smith & Nephew, UK). The general view of the vacuum dressing is shown in Figure 1.
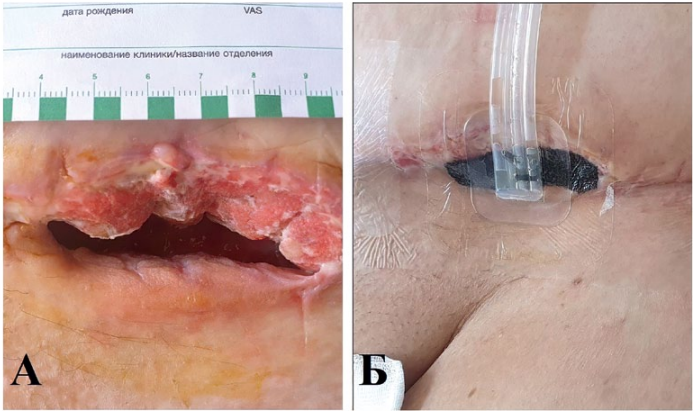
Рисунок 1. Общий вид вакуумной повязки. А — осложненная рана после герниопластики и абдоминопластики; Б — вид раны с установленной вакуумной повязкой (в рану расположена по размеру повязка-губка, сверху приклеена полупроницаемая прозрачная пленка, в область сформированного отверстия на пленке установлен двухходовый дренаж, подключённый к вакуумному аппарату).
Figure 1. General view of VAC. A — complicated wound after hernioplasty and abdomenoplasty; B — wound with installed VAC (sponge located in the wound according to size, a semi-transparent film installed, a two-way drainage connected to a vacuum device).
In the treatment of sacrococcygeal region and perineum wounds, vacuum therapy with variable pressure was used: during the first 8 days, a pressure of 50 mmHg for 2 minutes and 125 mmHg for 5 minutes was used; during the next 12 days, a variable regimen of pressure – 75 mmHg for 5 minutes and 125 mmHg for 2 minutes was used (Patent No. 2559936 of the Russian Federation, 2015). A clinical example of treatment with this method is shown in Figure 2.
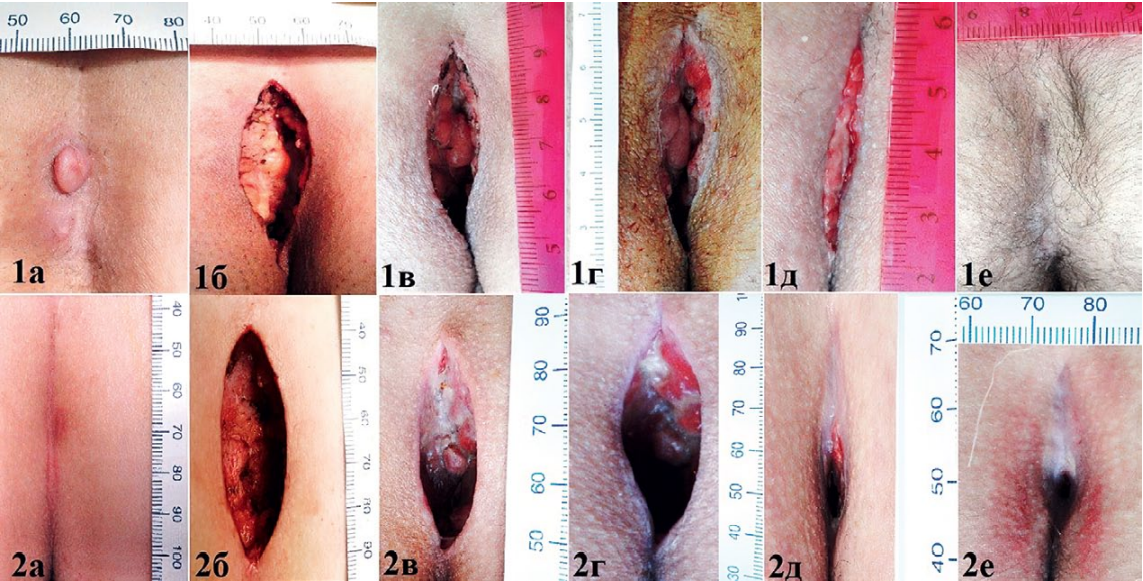
Рисунок 2. Динамика заживления после иссечения эпителиального копчикового хода с открытым ведением раны. 1е — рана c вакуум-терапией, полная эпителизация на 30-е сутки, 2е — рана без вакуумной терапии, на 41-е сутки полного заживления нет.
Figure 2. Dynamics of healing after excision of pilonidal sinus with open wound. 1e — wound with VAC, epithelialization on the 30th day, 2e — wound without VAC, on 41st day complete healing was not recorded.
Subsequently, the method was additionally modified for the treatment of wounds with paraimplant complications in surgery, where vacuum therapy was also used, but with the introduction of an antiseptic solution: round-the-clock VAC therapy in constant and variable modes of operation depending on the phase of the wound process with negative pressure from 75 to 125 mm Hg with instillation of antiseptic solutions (Patent No. 2760088 of the Russian Federation, 2021). The case of treatment with the developed method is illustrated in Figure 3.
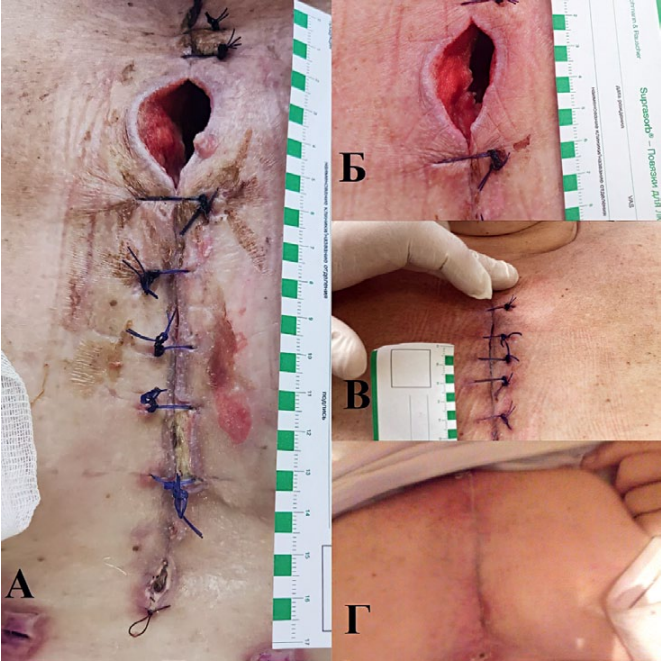
Рисунок 3. Динамики заживления раны у больной с послеоперационным стерномедиастинитом. А — вид раны до начала лечения вакуумной терапией; Б — 7-й день лечения; В — 15-й день лечения, наложены вторичные швы; Г — рана на 25-й день, полная эпителизация.
Figure 3. Dynamics of wound healing in a patient with sternomediastinitis. A — type of wound before the start of VAC; B — 7 days of treatment; С — 15th day of treatment, secondary sutures are applied; D — wound on day 25th, complete epithelialization.
In order to treat such life-threatening complications as postoperative esophageal fistula, a method of intracavitary vacuum therapy with antiseptic solutions washing was developed: in the first 10 days of treatment, pressure values were 100 mm Hg, 3 times a day through the mouth and into the drainage system 50 ml of antiseptic injected, in the next 7 days therapy was carried out at a pressure level of 70 mm Hg and 2 times a day 30 ml of antiseptic solution was used. Then the aspiration level was reduced to 50 mm Hg and maintained until the wound canal was completely regenerated (Patent No. 2758546 of the Russian Federation, 2021). The case of treatment with this method is illustrated in Figure 4.
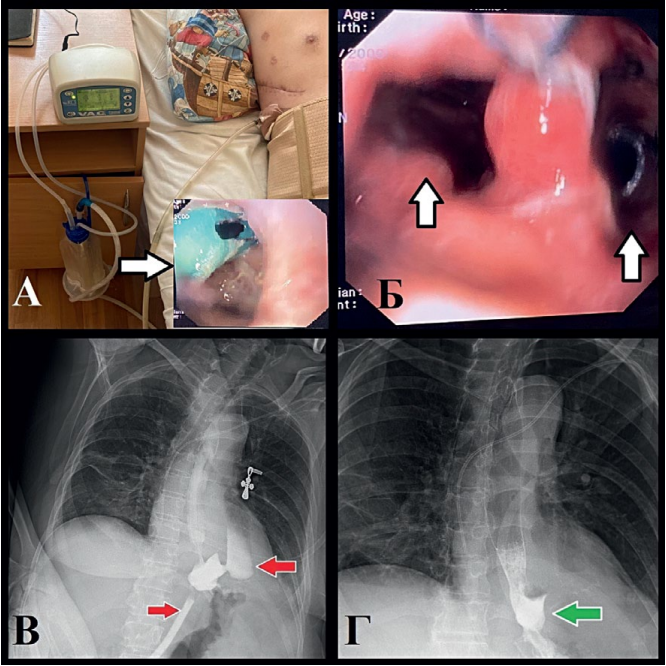
Рисунок 4. Клинический случай лечения послеоперационного пищеводного свища с помощью вакуумной терапии у пациента с гигантской параэзофагеальной грыжей. А — вид вакуумной системы, стрелкой указана эндоскопическая картина при госпитализации с установленной дренажной трубкой в просвете пищевода в другом учреждении, дренаж подтянут в свищевой ход, Б — эндоскопическая картина пищеводного свища (левая стрелка — просвет пищевода, правая — просвет свища с дренажем для вакуумной терапии), Г — рентгенографические признаки пищеводного свища до начала лечения; Д — заживление пищеводного свища на 6 сутки вакуумной терапии.
Figure 4. Clinical case of treatment postoperative esophageal fistula with vacuum therapy in a patient with a giant paraesophageal hernia. A — common view of VAC, arrow indicates endoscopic picture during hospitalization with a drainage tube installed in the lumen of esophagus in another institution, drainage is tightened into the fistula, B — endoscopic view of esophageal fistula (left arrow — esophagus, right — lumen of the fistula with drainage), D — radiographic signs of esophageal fistula before treatment; D — healing of esophageal fistula on the 6th day of VAC.
The intensity of pain syndrome before and after the start of vacuum therapy was assessed on a 10-point visual analog scale (VAS). To assess the general condition of patients, quantitative signs of a systemic inflammatory reaction were recorded. To characterize wound healing, a planimetric method was used with photographing and recording the rate of reduction of the wound surface and cytological examination of smears from the wound surface. A microbiological examination of the wound was carried out on the 1st and 8th day after the start of vacuum therapy.
Statistical data analysis was performed using Microsoft Excel 2016 and R (version 3.2, Vienna, Austria). Methods of descriptive statistics and the Shapiro-Wilk test for the normality of distributions were used, and for non-parametric indicators, the Fisher test was used to compare the frequency of signs, parametric indicators were indicated as mean and standard error (M ± m), and reliability was assessed using Student's t-test. Differences were accepted at p < 0.05.
Results
Vacuum therapy was started on the 2nd day after surgical treatment of wounds in 68 (53.1%) patients, on the 3rd-7th day – in 38 (29.7%), and in the remaining 22 (17.2%) patients – in the time of late postoperative treatment. The duration of negative pressure therapy averaged 22.1 ± 0.26 days with a range of 7 to 32 days.
In 47 (36.7%) cases, after the wound entered the reparative stage, secondary sutures were required, and in 30 (23.4%) cases skin grafting was required.
The VAS score averaged 1.4 ± 0.23 points. Figure 5 shows the dynamics of pain reduction. By the fourth day of treatment with VAC therapy, the pain decreased to 2.1 ± 0.22 points, on the 8th day the pain intensity was 1.5 ± 0.2, and by the 12th day of treatment with VAC therapy, the pain score did not exceed 0.8 ± 0.2 points, and in 76 (59.4%) patients, the pain syndrome was completely absent.
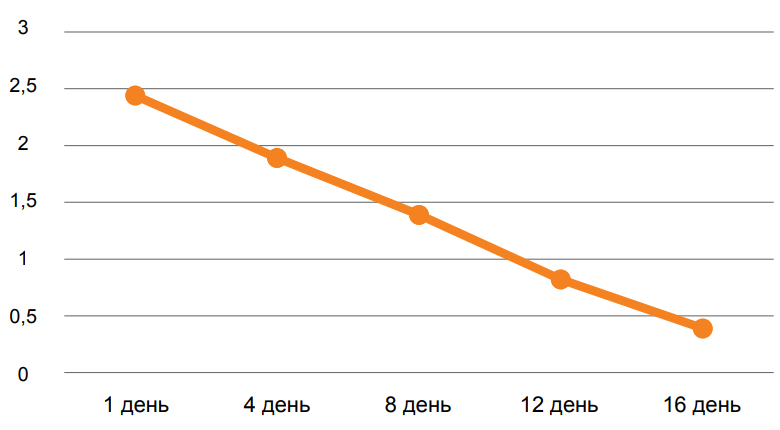
Рисунок 5. Динамика показателя ВАШ у пациентов с вакуумной терапией.
Figure 5. Dynamics of VAS index in patients with vacuum therapy.
A systemic inflammatory response was noted in 43 (33.6%) patients. Hemoculture growth was established in 20 (15.6%) cases; in 47.6% the infectious agent was Staphylococcus aureus, which in 33.3% of observations was MRSA. In 15.6% of cases, no microflora growth was obtained in the wound discharge. Microbiological examination of wound discharge revealed Staphylococcus aureus (MRSA) in 63.3% of cases, Enterococcus faecalis – in 24.7%, Pseudomonas aeruginosa – in 20.3%, Acinetobacter baumannii – in 19.7%, Escherichia coli – in 15.6%, in 12.6% – representatives of the genus Proteus, 14.4% – Klebsiella pneumoniae, 1.6% – Staphylococcus haemolyticus, and 0.8% – Serratia marcescenc. In wound discharge, monoculture was detected in 35 (32%) cases, and associations of microbes were detected in 73 (68%) observations and were represented by two to four types of microorganisms.
A cytological examination of wound smears on day 4 revealed inflammatory characteristics in 38 (29.7%) cases. On the 8th day after treatment, areas of granulation tissue were noted in 98 (76.6%) cases. Marginal epithelization and wound contraction were observed in 82 (64.1%) patients on day 12. One month after treatment complete healing was observed in 106 (82.8%) patients.
Microscopic characterization of the wound process on day 4 revealed inflammatory cytograms in 93 cases (72.6%), on day 8 of treatment with vacuum therapy inflammatory-regenerative cytograms in 104 (81.3%) cases, and on day 12 of treatment no inflammatory cytograms were observed, but regenerative cytograms were recorded in 39 (30.5%) cases.
The rate of wound healing with VAC therapy was 2.7 ± 0.35 cm2/day and ranged from 0.22 to 4.3 cm2/day. In all clinical cases, during the first 16 days of treatment wounds were more than halved in size by 62.1 ± 2.5% (57 to 69%) of the original wound area.
Complications of complex treatment with the use of vacuum therapy include wound bleeding in 7 (5.5%) patients, which required a change in treatment strategy: temporary cessation of vacuum therapy, loose plugging of the wound with ointment wipes, local hemostatic agents used in the area of the source of bleeding, and the resumption of vacuum therapy after hemostasis.
Repeat surgeries and necrectomies were required in 11 (8.5%) patients. Of the 128 patients, 1 patient with postoperative sternomediastinitis died, the overall mortality rate was 0.8%, the cause of death was acute cardiovascular failure. Patients were discharged from the hospital on the 10th-25th day of treatment, the average period of complete healing of postoperative wounds was 29.3 ± 0.4 days (from 22 to 53 days), which corresponded to the terms of temporary disability, there were no cases of patients refusing to undergo vacuum therapy. Treatment results are presented in Table 2.
Таблица / Table 2
Результаты лечения ран с применением вакуум-терапии
Results of wound treatment with VAC
|
Характер операции Type of surgical operation |
n* |
Краевая эпителизация на 12-й день**, Epithelialization, day 12th, ** |
Контракция раны на 50% к 16-му дню**, Wound contraction, day 16th, ** |
Полное заживление раны, дни, Complete wound healing |
Нетрудоспособности, дни, Disability |
Осложнения, n** Complications, n** |
|
Иссечения эпителиального копчикового хода Excision of pilonidal sinus |
40 (31,2) |
28 (70) |
31 (77,5) |
27,3 |
28,6 |
4 (10) |
|
Стерномедиастинит Sternomediastinitis |
23 (18) |
10 (43,5) |
11 (47,8) |
32,5 |
34,8 |
3 (13) |
|
Герниопластика с эксплантом Hernioplasty with mesh |
16 (12,5) |
10 (62,5) |
11 (68,8) |
29,1 |
30,7 |
0 |
|
Плановая лапаротомия Common laparotomy |
15 (11,7) |
15 (100) |
14 (93,3) |
26,9 |
28,7 |
0 |
|
Экстренная лапаротомия Emergency laparotomy |
7 (5,5) |
7 (100) |
5 (71,4) |
28,7 |
31,2 |
0 |
|
Параимплантные осложнения в травматологии Paraimplant complications in traumatology |
7 (5,5) |
6 (85,7) |
5 (71,4 |
29,5 |
30,2 |
0 |
|
Аутогерниопластика, абдоминопластика Autohernioplasty, abdominoplasty |
7 (5,5) |
7 (100) |
7 (100) |
29,5 |
30,6 |
0 |
|
Послеоперационные пищеводные свищи Postoperative esophageal fistulas |
6 (4,7) |
- |
6 (100) |
31,2 |
31,6 |
0 |
|
Декубитальные язвы Decubital ulcers |
4 (3,1) |
2 (50) |
2 (50) |
31,7 |
32,6 |
0 |
|
Маммопластика Mammoplasty |
3 (2,3) |
3 (100) |
3 (100) |
26,9 |
29,3 |
0 |
|
Всего Total |
128 |
88 (68,8) |
95 (73,4) |
- |
- |
7 (5,5) |
|
Средние значение Average values |
- |
- |
- |
29,3 |
30,8 |
- |
Примечание: *в скобках приведены % отношения выявленных случаев к общему количеству наблюдений; ** в скобках приведены % отношения выявленных случаев к характеру операции.
Note: *in parentheses are the % ratio of identified cases to the total number of observations; **% ratio of identified cases to the nature of the operation is given in parentheses.
Discussion
Due to the active development of surgery, there is an increase in the number of operations annually. However, despite modern surgical technologies, aseptic and antiseptic advances, and antimicrobial therapy, the problem of treatment of surgical site infections remains relevant [2].
The problem of complications in the operating wound area is relevant against the background of an increase in the number of geriatric, comorbid patients, and an increase in the incidence of diabetes mellitus and resistance of microorganisms [2]. In the presented study, resistant microflora in the wound discharge was found in 63.3% of patients, and comorbidity was detected in 59 (46.1%) patients, of which 42 (32.8%) had diabetes mellitus.
The expansion of the operation with the use of various types of prostheses, unfortunately, increased the incidence of infectious complications in the deep tissues of the surgical area. It should also be noted the role of microorganisms with biofilm-forming ability, which contributes to a long-functioning focus of infection, forming chronic forms. At the same time, reparative regeneration is imperfect, and reactions in the implant zone ultimately lead to rejection and elimination [10]. In our study, prosthetic operations were performed in 30 (23.4%) patients, of which 23 (18%) underwent abdominal wall prosthetics and 7 (2.4%) joint prosthetics, while against the background of complex treatment using vacuum therapy, the prosthesis was preserved in all cases.
Conclusions
Local negative pressure therapy is an effective option for wound management in purulent surgery.
Vacuum therapy provides an accelerated transition of the wound process into the reparative stage due to increased exudate outflow and reduced bacterial load, improved blood flow, which is manifested in the positive dynamics of the cytological picture of the wound and accelerated reduction in its size.
Negative pressure therapy reduces the likelihood of seroma and hematoma formation, as well as repeated operations. With paraimplant and paraprosthetic infection, in combination with instillation with modern antiseptic solutions, it effectively drains the focus area of inflammation, isolates the implant, and reduces the frequency of secondary wound infection, which in most cases allows preserving the prosthesis.
Our experience demonstrates the convenience of vacuum therapy for the patient and hospital staff, as it can significantly reduce the number of bandages even during the exudation phase. Vacuum dressings are compact, do not cause discomfort when worn, and can be used in outpatient treatment.
As a result, the terms of complete wound repair for surgical infection of soft tissues are significantly reduced, as well as the period of expensive inpatient treatment and the terms of disability of patients.
References
1. Fedyushkin V.V., Barishev A.G. Vacuum-assisted healing of various-aetiology wounds: A systematic review. Kuban Scientific Medical Bulletin. 2021;28(6):117-132. (In Russ.) https://doi.org/10.25207/1608-6228-2021-28-6-117-132
2. Cherkasov M.F., Galashokjan K. M., Lukash A. I., Starcev Ju.M., Cherkasov D.M. et al. Treatment of various ethiology wounds with vac-therapy. Modern problems of science and education. 2019;(6):136. (In Russ.) https://doi.org/10.17513/spno.29337
3. Fedjushkin V.V., Pjatakov S.N., Baryshev A.G., Pjatakova S.N., Shсherba S.N., et al. Vacuum therapy for the prevention of suppurations in sutured soft tissue wounds. First experience. Wounds and wound infections. The prof. B.M. Kostyuchenok journal. 2022;9(4):6-15. (In Russ.) https://doi.org/10.25199/2408-9613-2022-9-4-6-15
4. Gumanenko E.K., Ogarkov P.I., Lebedev V.F., Bojarincev V.V., Kuzin A.A. Infectious complications of polytraumas: microbiological and epidemiological aspects. Grekov's bulletin of surgery. 2006;165(5):56-62. (In Russ.). EDN: KVKWBF
5. Samokhvalov I.M., Kryukov E.V., Markevich V.Y., Badalov V.I., Goncharov A.V. Military field surgery in 2031. Voenno-medicinskij žurnal. 2021;342(9):4-11. (In Russ.) https://doi.org/10.52424/00269050_2021_342_9_04
6. Huang C, Leavitt T, Bayer LR, Orgill DP. Effect of negative pressure wound therapy on wound healing. Curr Probl Surg. 2014;51(7):301-331. https://doi.org/10.1067/j.cpsurg.2014.04.001
7. Silin A.A., Zhidkov A.S., Korik V.E., Zhidkov S.A. Vacuum therapy in the treatment of the wounds. Modern tendencies. Military medicine. 2019;1(50):117–122. (In Russ.). EDN: YWJJIL
8. Obolenskiy V.N. Modern treatment methods of the chronic wounds. Meditsinskiy sovet = Medical Council. 2016;(10):148-154. (In Russ.) https://doi.org/10.21518/2079-701X-2016-10-148-154
9. Kanshin N.N. Nesformirovannye kishechnye svishhi i gnojnyj peritonit (hirurgicheskoe lechenie). Moscow: Profil'; 2007. (In Russ.)
10. Agarwal P, Kukrele R, Sharma D. Vacuum assisted closure (VAC)/negative pressure wound therapy (NPWT) for difficult wounds: A review. J Clin Orthop Trauma. 2019;10(5):845-848. https://doi.org/10.1016/j.jcot.2019.06.015
About the Authors
M. F. CherkasovRussian Federation
Mikhail F. Cherkasov, Dr. Sci. (Med.), Professor, Head of the Department of Surgery No. 4
Rostov-on-Don
K. M. Galashokyan
Russian Federation
Karapet M. Galashokyan, Cand. Sci. (Med.), Assistant Professor of Surgery No. 4
Rostov-on-Don
Yu. M. Startsev
Russian Federation
Yuri M. Startsev, Cand. Sci. (Med.), Associate Professor of Surgery Department No. 4
Rostov-on-Don
D. M. Cherkasov
Russian Federation
Denis M. Cherkasov, Dr. Sci. (Med.), Associate Professor of the Department of Surgical Diseases No. 2
Rostov-on-Don
S. G. Melikova
Russian Federation
Sabina G. Melikova, surgeon of the clinical and polyclinic department
Rostov-on-Don
K. E. Rudkova
Russian Federation
Ksenia E. Rudkova, 5th year student
Rostov-on-Don
Review
For citations:
Cherkasov M.F., Galashokyan K.M., Startsev Yu.M., Cherkasov D.M., Melikova S.G., Rudkova K.E. Ten years’ experience of vacuum systems in treatment of complicated postoperative wounds of various etiologies. Medical Herald of the South of Russia. 2024;15(3):106-114. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-3-106-114







































