Scroll to:
Quality of life of patients and distinctive properties of the postoperative period after minimally invasive video-assisted hemithyroidectomy
https://doi.org/10.21886/2219-8075-2024-15-2-33-43
Abstract
Objective: to study indicators of the quality of life of patients and features of the course of the postoperative period after minimally invasive video-assisted hemithyroidectomy (MIVAH) in comparison with traditional open hemithyroidectomy (OH).
Materials and methods: an analysis of the quality of life and postoperative results was carried out in 92 patients with benign nodular neoplasms of the thyroid gland. The study group included 45 patients who underwent MIVAH. The control group included 47 patients who underwent OH.
Results: pain levels were lower in the MIVAH group throughout the evaluation period. At the same time, the statistical significance of the differences (p<0.05) in the level of pain was noted at 24–-48 hours after the operation. Swallowing disorders were noted by patients less frequently in the MIVAH group (by 14.0% 1 month after surgery and by 8.0% after 6 months). Analysis of quality of life indicators on the SF-36 scale demonstrated that at 1 month after surgery, patients in the MIVAH group had higher values of the Physical Functioning (92.7±10.2 versus 83.1±15.3 points; p<0.05), Role-Physical Functioning (86.1±11.7 versus 63.0±14.8 points; p<0.01) and Social Functioning (82.4±13.9 versus 72.6±14.8 points; p<0.05). 6 months after surgery, all SF-36 scale indicators showed leveling off between the comparison groups.
Conclusions: the MIVAH technique, compared with traditional open surgery, is characterized by an improvement in a number of indicators of the postoperative period. After MIVAH, the quality of life of patients is significantly higher in the early postoperative period, but in the long-term postoperative period, the quality of life shows comparable indicators both after MIVAH and after OH.
Keywords
For citations:
Kurganov I.A., Mamistvalov M.Sh., Usmanov I.S., Emelyanov S.I. Quality of life of patients and distinctive properties of the postoperative period after minimally invasive video-assisted hemithyroidectomy. Medical Herald of the South of Russia. 2024;15(2):33-43. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-2-33-43
Introduction
Minimally invasive video-assisted surgery on thyroid glands (TGs), first developed by P. Miccoli, is currently the most common intervention in thyroid surgery performed using videoendoscopic technologies [1][2].
A number of advantages have been noted upon the introduction of minimally invasive video-assisted thyroid surgery into clinical practice. Those include reducing the surgical trauma; a good level of visual control of anatomical structures due to the use of endoscopic equipment with an increased field of view; a low complication rate, not exceeding that at open surgery; a relatively short duration of the intervention; possibility of rapid conversion of access; convenience for both hemithyroidectomy and total thyroidectomy; applicability upon malignant neoplasms; relative ease of mastering the technique compared to other methods of endoscopic thyroid surgery for surgeons experienced in performing traditional thyroid interventions [3–5].
The above advantages are confirmed by the successful implementation of a fairly large series of video-assisted surgeries. For instance, Del Rio et al. [6] performed thyroid surgeries through a mini-access in 497 patients over 10 years. Among the complications of the surgery, 1 case (0.2%) of bleeding, 12 cases (2.4%) of transient vocal cord paralysis, and 4 cases (0.8%) of permanent cord paralysis were recorded. Besides, the frequency of serological hypocalcemia was 24.9% (124 cases), clinical hypocalcemia amounted to 7.2% (36 cases), and permanent hypoparathyroidism developed in 1 patient (0.2%). In total, the team headed by the author of the considered technique Miccoli [7] performed 2698 minimally invasive video-assisted thyroid surgeries from 1998 to 2019. Thyroidectomy was performed in 1862 cases (69%), while hemithyroidectomy was accomplished in 763 cases (28.3%). Total thyroidectomy with central lymph node dissection in the neck was performed in 31 patients (1.2%). In 42 cases (1.6%), removal of parathyroid glands was performed along with total thyroidectomy due to concomitant primary hyperparathyroidism. Temporary postoperative hypoparathyroidism was detected in 188 cases (7%), and permanent hypoparathyroidism was registered in 12 cases (0.4%). Permanent unilateral vocal cord paralysis was recorded in 38 patients (1.4%). Permanent bilateral vocal cord dysfunction was not observed in any of the cases. Six patients (0.2%) required reoperation due to postoperative bleeding, and four patients (0.1%) developed wound infection. Access conversion was performed in 43 cases (1.6%).
It should be noted that at present, along with the trend towards expanding the use of minimally invasive technologies in thyroid surgery, there is also a trend towards more frequent organ-preserving surgical treatment in the form of hemithyroidectomy, which is considered sufficient and adequate in a significant number of patients with nodular goiter. The corresponding provisions are also reflected in clinical recommendations [8][9].
On the other hand, despite numerous works devoted to the safety and short-term results of endoscopic and video-assisted thyroid surgery, the issues of investigating the postoperative period and the quality of life of patients after these operations remain insufficiently analyzed and require further careful assessment, which determines the relevance of this research work.
The aim of the study was to examine the quality of life of patients and the features of the postoperative period after minimally invasive video-assisted hemithyroidectomy (MIVAH) in comparison with traditional open hemithyroidectomy (OH).
Materials and methods
The study was based on the analysis of the quality of life and postoperative results in 92 patients with benign nodular neoplasms of the TGs, who were indicated for surgical intervention in the volume of hemithyroidectomy. The studied group included 45 patients who underwent MIVAH according to Miccoli’s method (MIVAH group). The control group included 47 patients who underwent hemithyroidectomy according to the traditional open method (OH group). The type of investigation corresponds to a non-randomized controlled study, which is based on a comparative analysis of the indicators of the postoperative period course in the specified groups of patients including the level of pain syndrome in the early postoperative period, data on changes and impairments in head function and the act of swallowing in the early and late postoperative periods, as well as an analysis of indicators of the quality of life of patients at the corresponding times after surgery.
All operations were performed in the surgical department of the hospital of the Central Union of the Russian Federation, which is the clinical base of the Department of Endoscopic Surgery of the Federal State Budgetary Educational Institution of Higher Education "Russian University of Medicine" of the Ministry of Health of the Russian Federation (previously called Federal State Budgetary Educational Institution of Higher Education "Moscow State University of Medicine and Dentistry named after A.I. Evdokimov" of the Ministry of Health of the Russian Federation until 2023).
The criteria for inclusion of patients in the study were the age of 18 years or older, nodular or multinodular goiter localized in one lobe of the TG, the benign nature of the nodule/nodes (TIRADS 2-3 and Bethesda II or IV), voluntary consent of the patient for surgery and participation in the study. The criteria for non-inclusion of patients in the study were the contraindications to planned surgical treatment or to general anesthesia, signs of malignancy of the tumor, body mass index (BMI) of the patient over 35 kg/m2, confirmed diagnosis of thyroiditis, diffuse toxic goiter, multiple endocrine neoplasia syndrome, primary/secondary/tertiary hyperparathyroidism, previous surgeries and/or radiation therapy in the neck area. The exclusion criteria involved the detection of a disease during the preoperative examination or in intraoperative time, which could affect the scope and nature of the surgical intervention, as well as failing to follow the recommendations of the attending physician in the postoperative period and refusing to undergo a follow-up examination.
The patients included in the study were operated in the period between 2018 and 2022; the follow-up period lasted for 6 months with control points at 1 and 6 months after the surgery. Patients were surveyed during follow-up examinations and/or remotely in the postoperative period. The level of pain was assessed using a typical ten-point visual analogue scale (VAS). Patients completed the VAS questionnaire within the first 6 days after the surgery. The presence and severity of changes in the voice function and the act of swallowing were determined at 1 and 6 months after the operation using a three-point questionnaire, in which patients gave a subjective assessment of their sensations (0 points — no changes compared to the period before the intervention, 1 point — minor changes, 2 points — moderate changes, 3 points — significant changes). To estimate the postoperative quality of life of patients, the standard SF-36 questionnaire was used to assess physical functioning, role functioning stipulated by the physical condition, pain intensity, general health, vital activity, social functioning, role functioning stipulated by the emotional state, and mental health. A questionnaire survey according to the SF-36 scale was conducted 1 and 6 months after the operation.
To compare perioperative data in the studied and control groups, the main indicators characterizing the selected clinical material were recorded. Moreover, the complications obtained were recognized as one of the most important factors directly affecting the course of the postoperative period (Table 1).
Таблица / Table 1
Периоперационные показатели у пациентов в группах сравнения
Perioperative indicators in patients in comparison groups
|
Показатель Index |
Группа МИВАГ (n=45) MIVAH Group (n=45) |
Группа ОГ (n=47) OH Group (n=47) |
Статистическая значимость различий, p Statistical significance of differences, p |
|
Мужчины / Женщины, n (%) Men / Women, n (%) |
10 (22,2%) 35 (77,8%) |
13 (28,7%) / 34 (72,3 %) |
p>0,05 |
|
Возраст, лет Age, years |
36,3±12,9 |
39,4±12,1 |
p>0,05 |
|
ИМТ, кг/м² BMI, kg/m² |
24,0±6,6 |
24,9±6,7 |
p>0,05 |
|
Правостороннее / Левостороннее узловое образование), n (%) Right-sided / Left-sided nodular formation, n (%) |
23 (51,1%) 22 (48,9%) |
24 (51,1%) / 23 (48,9%) |
p>0,05 |
|
Средний размер узла, см Average size of the node, cm |
2,7±0,9 |
4,4±1,6 |
p<0,05 |
|
Средний объём ЩЖ, мл Average thyroid volume, ml |
28,9±8,5 |
57,8±11,8 |
p<0,05 |
|
Bethesda II / Bethesda IV, n (%) Bethesda II / Bethesda IV, n (%) |
15 (33,3%) / 30 (66,7%) |
31 (66,0%) / 16 (34,0%) |
p<0,05 |
|
Эутиреоз / Тиреотоксикоз (тиреотоксическая аденома), n (%) Euthyroidism / Thyrotoxicosis (thyrotoxic adenoma), n (%) |
39 (86,7%) / 6 (13,3%) |
42 (89,4%) / 5 (10,6%) |
p>0,05 |
|
Среднее время операции, мин. Average operation time, min. |
54,4±15,2 |
55,1±15,5 |
p>0,05 |
|
Средний уровень кровопотери, мл Average blood loss, ml |
18,7±9,9 |
19,2±8,1 |
p>0,05 |
|
Средняя длина операционного разреза, см Average length of surgical incision, cm |
1,8±0,4 |
5,7±0,4 |
p<0,01 |
|
Средний объём отделяемого по дренажу, мл Average volume of drainage discharge, ml |
- |
25,7±7,3 |
- |
|
Средняя длительность госпитализации, сут. Average duration of hospitalization, days |
3,2±1,3 |
4,1±1,7 |
p<0,05 |
|
Осложнения, n (%) Complications, n (%) – Clavien-Dindo I, n (%) – Clavien-Dindo II, n (%) – Clavien-Dindo IIIb, n (%) |
2 (4,4%) - - 2 (4,4%) |
3 (6,4%) - 2 (4,3%) 1 (2,1%) |
p>0,05 p>0,05 p>0,05 p>0,05 |
The presented data demonstrated that the groups were comparable in terms of demographic parameters (distribution by gender, age, BMI), the side of the thyroid nodule location, the frequency of detection of thyrotoxicosis associated with the functional autonomy of the nodule, the average time of surgery, and the level of blood loss.
Concurrently, the average node size and thyroid volume according to ultrasound data were significantly smaller in the MIVAH group compared to the OH group. Significant differences were also revealed in the results of the cytological examination of the material obtained during fine-needle biopsy. Patients with the established cytological category Bethesda II predominated in the OH group, while in the MIVAH group patients with the Bethesda IV category were prevalent. This distribution was associated with limitations in the average size of the angular formation and the TG volume, which are available for performing surgery according to the MIVAH method. In this regard, the OH group more often included patients who were diagnosed with colloid goiter with a large node size or with its rapid growth before surgery, while in the MIVAH group, the indication for surgery in a significant number of cases was the diagnosis of "thyroid adenoma" established at the stage of preoperative examination.
It is important to note that predictably the average length of the skin incision was significantly shorter in the studied group. In addition, the hospitalization period of patients in the studied group was also significantly shorter than in the control group. It should be especially emphasized that after performing MIVAH, wound drainage was not performed, which was one of the factors affecting the length of stay of patients in hospital conditions.
The differences in the complication rate between the studied and control groups were insignificant. Complications were assessed by the Clavien-Dindo scale. No case of complications of the first degree was recorded in any of the comparison groups. Complications of the second degree according to the Clavien-Dindo scale were revealed in 2 cases (4.3%) in the control group and were represented by transient unilateral paresis of the vocal cords, which resolved within 6 months after surgery. Complications of degree IIIb according to the Clavien-Dindo scale were represented by bleeding in the early postoperative period in 2 cases (4.4%) in the MIVAH group and in 1 case (2.1%) in the OH group. In all cases of bleeding, the revision of the postoperative wound was performed to identify the source of bleeding and arrest it.
Besides, it should be noted that in the MIVAH group, there were 2 cases (4.4%) of conversion of surgical access due to the impossibility of further safe tissue dissection within the limited space.
Methods of statistical data proceeding
The software included in the Microsoft Excel 2021 data editor and the AnalystSoft StatPlus 7 statistical complex were used to record, analyze, and statistically process the obtained results. The statistical significance of differences in qualitative indicators was assessed by calculating the Pearson χ2 criterion and Fisher's exact test. The statistical significance of differences in quantitative indicators was assessed by calculating Student's t-test or the nonparametric Mann-Whitney U-test. In all cases, differences between the studied and control groups were considered significant at p<0.05, and highly significant at p<0.01. For quantitative indicators, confidence intervals were also calculated for a statistical probability of 95.0%.
Results
In the present work, special attention was paid to analyzing the results of interventions on the TG, which affect the quality of life of patients in the early and late postoperative period. In particular, an assessment of the level of pain syndrome in the early postoperative period (Fig. 1) showed that the intensity of pain was less in the MIVAH group throughout the follow-up period. Notably, significant differences (p<0.05) in the level of pain syndrome were noted 24–48 hours after the operation. The maximum average difference in the assessment of pain intensity according to VAS was 1.8 points and was noted 48 hours after the surgery. In general, with the existing pain intensity, parenteral analgesia was required in patients of the comparison groups in the period up to 48–72 hours after the operation as then the pain intensity decreased to minimal values.
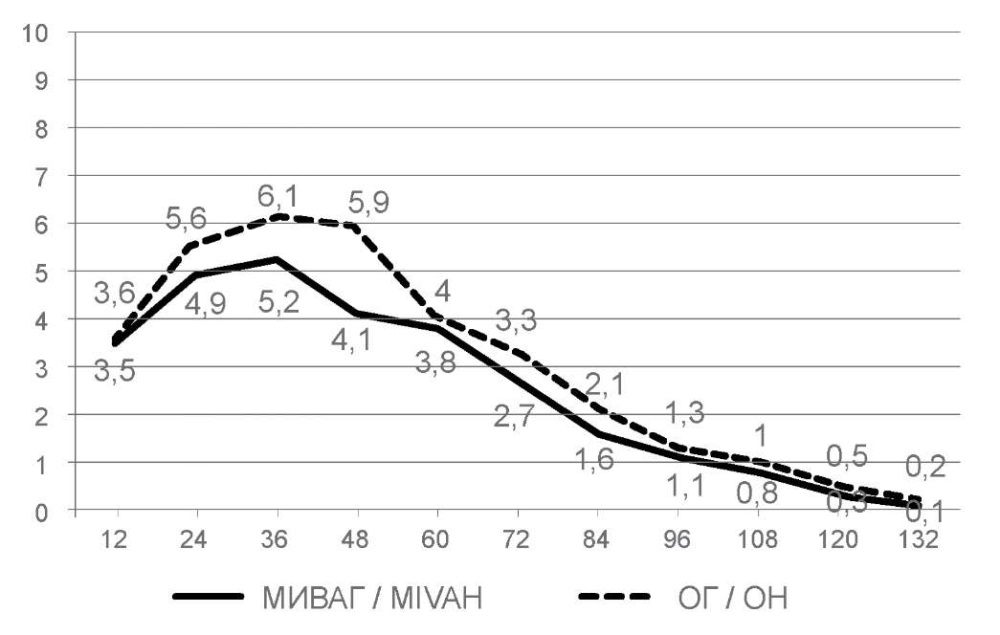
Рисунок 1. Уровень послеоперационного болевого синдрома по ВАШ в группах сравнения
(по оси абсцисс — часы после операции, по оси ординат — балльная оценка).
Figure 1. The level of postoperative pain syndrome according to VAS in the comparison groups
(the x-axis is hours after surgery, the y-axis is the score)
The investigation of voice function and swallowing disorders 1 month after the operation (Table 2) revealed that voice changes were noted by 9 patients (20.0%) in the MIVAH group and 10 patients (21.3%) in the OH group (p> 0.05). The average score of voice disorders after a month of the follow-up period was 0.24 among patients in the studied group and 0.36 among patients in the control group (p>0.05). It should be noted that 2 cases of pronounced voice changes, which were noted in patients in the control group, were stipulated by transient unilateral paresis of the vocal cords. In all other cases, voice changes at minor and moderate levels were recorded by patients against the background of an uncomplicated postoperative period.
Таблица / Table 2
Оценка наличия и выраженности нарушений голосовой функции и акта глотания
после гемитиреоидэктомии в группах сравнения через 1 месяц после операции
Assessment of the presence and severity of disorders of voice function and swallowing
after hemithyroidectomy in comparison groups 1 month after surgery
|
Выраженность изменений в соответствие с балльной оценкой The severity of changes in accordance with the score |
Группа МИВАГ (n=45) MIVAH Group (n=45) |
Группа ОГ (n=47) OH Group (n=47) |
Статистическая значимость различий, p Statistical significance of differences, p |
|
Изменения голоса Voice changes |
|||
|
0 баллов, n (%) 0 points, n (%) |
36 (80,0%) |
37 (78,7%) |
p>0,05 |
|
1 балл, n (%) 1 point, n (%) |
7 (15,6%) |
5 (10,6%) |
p>0,05 |
|
2 балла, n (%) 2 points, n (%) |
2 (4,4%) |
3 (6,4%) |
p>0,05 |
|
3 балла, n (%) 3 points, n (%) |
- |
2 (4,3%) |
p>0,05 |
|
Дискомфорт при глотании Discomfort when swallowing |
|||
|
0 баллов, n (%) 0 points, n (%) |
35 (77,8%) |
30 (63,8%) |
p>0,05 |
|
1 балл, n (%) 1 point, n (%) |
5 (11,1%) |
10 (21,3%) |
p>0,05 |
|
2 балла, n (%) 2 points, n (%) |
4 (8,9%) |
6 (12,8%) |
p>0,05 |
|
3 балла, n (%) 3 points, n (%) |
1 (2,2%) |
1 (2,1%) |
p>0,05 |
The presence of discomfort and changes during the act of swallowing 1 month after the operation was noted by 10 patients (22.2%) of the MIVAH group and 17 patients (36.2%) of the OH group, which did not constitute significant differences (p<0.05) despite the variation of the indicators in the analyzed volume of clinical material. The average score of changes in the act of swallowing was 0.36 in the MIVAH group and 0.53 in the OH group, which also proved to be an insignificant difference (p<0.05).
Analysis of changes in the voice function and swallowing act 6 months after the surgery (Table 3) showed that 3 patients (6.7%) in the studied group and 4 patients (8.5%) in the control group noted the retaining of voice changes (p> 0.05). Concurrently, all patients who had previously been diagnosed with dysphonia due to impaired vocal cord mobility noted the complete resolution of these symptoms. The average score of voice changes 6 months after the intervention was 0.07 in the MIVAH group and 0.11 in the OH group, which did not differ significantly (p>0.05).
Таблица / Table 3
Оценка наличия и выраженности нарушений голосовой функции и акта глотания
после гемитиреоидэктомии в группах сравнения через 6 месяцев после операции
Assessment of the presence and severity of disorders of voice function and swallowing
after hemithyroidectomy in comparison groups 6 months after surgery
|
Выраженность изменений в соответствие с балльной оценкой The severity of changes in accordance with the score |
Группа МИВАГ (n=45) MIVAH Group (n=45) |
Группа ОГ (n=47) OH Group (n=47) |
Статистическая значимость различий, p Statistical significance of differences, p |
|
Изменения голоса Voice changes |
|||
|
0 баллов, n (%) 0 points, n (%) |
42 (93,3%) |
43 (91,5%) |
p>0,05 |
|
1 балл, n (%) 1 point, n (%) |
3 (6,7%) |
3 (6,4%) |
p>0,05 |
|
2 балла, n (%) 2 points, n (%) |
- |
1 (2,1%) |
p>0,05 |
|
3 балла, n (%) 3 points, n (%) |
- |
- |
- |
|
Дискомфорт при глотании Discomfort when swallowing |
|||
|
0 баллов, n (%) 0 points, n (%) |
40 (88,9%) |
38 (80,9%) |
p>0,05 |
|
1 балл, n (%) 1 point, n (%) |
4 (8,9%) |
7 (14,9%) |
p>0,05 |
|
2 балла, n (%) 2 points, n (%) |
1 (2,2%) |
2 (4,2%) |
p>0,05 |
|
3 балла, n (%) 3 points, n (%) |
- |
- |
- |
Discomfort during swallowing continued to be noted 6 months after the operation by 5 patients (11.1%) from the MIVAH group and 9 patients (19.1%) from the OH group (p>0.05). The average score of the noted changes was 0.13 and 0.23, respectively (p>0.05).
Analysis of quality of life indicators according to the SF-36 scale demonstrated that 1 month after the operation (Table 4, Fig. 2), patients in the MIVAH group had a number of higher indicators compared to patients in the OH group. In particular, higher values of the physical functioning criterion (92.7±10.2 versus 83.1±15.3 points; p<0.05) and the role functioning criterion due to physical condition (86.1±11.7 versus 63.0±14.8 points; p<0.01) were recorded from the physical health component group. In the group of indicators of the psychological component of health, the differences in the criterion of social functioning (82.4±13.9 versus 72.6±14.8 points; p<0.05) were significant in favor of the MIVAH group. It should be noted that for all other criteria of both the physical and psychological components of health, patients from the MIVAH group also showed higher indicators but they did not have significant differences compared to the OH group according to statistical proceeding.
Таблица / Table 4
Показатели качества жизни пациентов по шкале SF-36
через 1 месяц после гемитиреоидэктомии в группах сравнения
Indicators of the quality of life of patients on the SF-36 scale
1 month after hemithyroidectomy in the comparison groups
|
Показатель Index |
Группа МИВАГ (n=45) MIVAH Group (n=45) |
Группа ОГ (n=47) OH Group (n=47) |
Статистическая значимость различий, p Statistical significance of differences, p |
|
Физическое функционирование Physical Functioning |
92,7±10,2 |
83,1±15,3 |
p<0,05 |
|
Ролевое функционирование, обусловленное физическим состоянием Role-Physical Functioning |
86,1±11,7 |
63,0±14,8 |
p<0,01 |
|
Интенсивность боли Bodily pain |
85,2±10,1 |
81,70±12,0 |
p>0,05 |
|
Общее состояние здоровья General Health |
76,8±14,2 |
71,8±13,9 |
p>0,05 |
|
Жизненная активность Vitality |
75,1±12,7 |
74,7±11,1 |
p>0,05 |
|
Социальное функционирование Social Functioning |
82,4±13,9 |
72,6±14,8 |
p<0,05 |
|
Ролевое функционирование, обусловленное эмоциональным состоянием Role-Emotional Functioning |
72,3±13,5 |
67,8±11,8 |
p>0,05 |
|
Психическое здоровье Mental Health |
74,3±18,6 |
70,4±19,3 |
p>0,05 |

Рисунок 2. Сравнение показателей качества жизни пациентов по шкале SF-36
в группах сравнения через 1 месяц после операции в графическом виде
Figure 2. Comparison of quality of life indicators of patients on the SF-36 scale
in comparison groups 1 month after surgery in graphical form
Six months after the operation (Table 5, Fig. 3), all SF-36 scale indicators in both groups demonstrated an increase in values compared to those at a month follow-up period. Concurrently, the values of all criteria were higher in the MIVAH group but significant differences according to statistical proceeding were not recorded for any of the indicators. The greatest average difference in scores was noted on the indicators of role functioning due to physical condition (4.5 points) and social functioning (4.9 points) in favor of the MIVAH group.
Таблица / Table 5
Показатели качества жизни пациентов по шкале SF-36
через 6 месяцев после гемитиреоидэктомии в группах сравнения
Indicators of the quality of life of patients on the SF-36 scale
6 months after hemithyroidectomy in the comparison groups
|
Показатель Index |
Группа МИВАГ (n=45) MIVAH Group (n=45) |
Группа ОГ (n=47) OH Group (n=47) |
Статистическая значимость различий, p Statistical significance of differences, p |
|
Физическое функционирование Physical functioning |
94,1±8,5 |
92,2±10,7 |
p>0,05 |
|
Ролевое функционирование, обусловленное физическим состоянием Role-physical functioning |
88,7±11,0 |
84,2±13,5 |
p>0,05 |
|
Интенсивность боли Bodily pain |
90,3±7,9 |
89,4±10,3 |
p>0,05 |
|
Общее состояние здоровья General health |
88,2±11,8 |
85,8±12,0 |
p>0,05 |
|
Жизненная активность Vitality |
87,5±10,2 |
87,3±11,4 |
p>0,05 |
|
Социальное функционирование Social functioning |
90,3±7,5 |
85,4±9,6 |
p>0,05 |
|
Ролевое функционирование, обусловленное эмоциональным состоянием Role-emotional functioning |
84,5±10,1 |
81,1±11,2 |
p>0,05 |
|
Психическое здоровье Mental health |
90,7±10,6 |
89,1±11,1 |
p>0,05 |
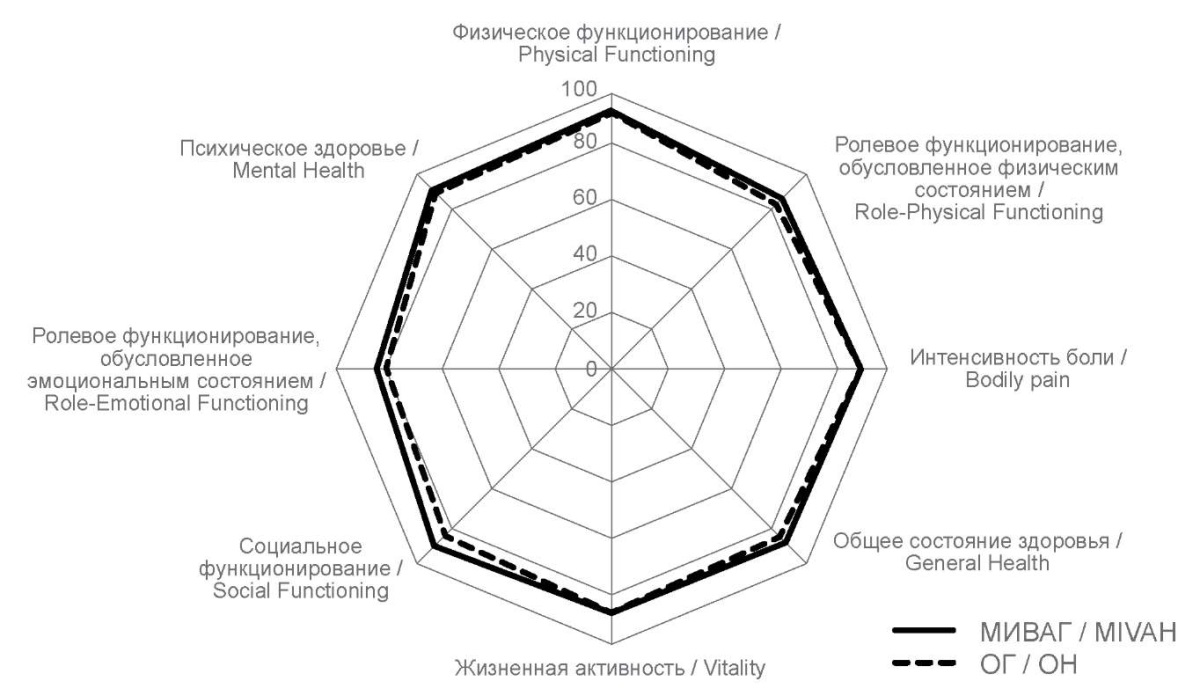
Рисунок 3. Сравнение показателей качества жизни пациентов по шкале SF-36
в группах сравнения через 6 месяцев после операции в графическом виде
Figure 3. Comparison of quality of life indicators of patients on the SF-36 scale
in comparison groups 6 months after surgery in graphical form
Discussion
Minimally invasive video-assisted interventions are currently the most common thyroid surgeries performed by videoendoscopic technologies. They combine a low surgical injury level and relative ease of mastering. On the other hand, the impact of these interventions on the course of the postoperative period, in particular on the postoperative quality of life of patients, has not been sufficiently studied.
A comparative analysis of short- and long-term postoperative results of surgical treatment of patients who underwent hemithyroidectomy according to the MIVAH method and the traditional open technique was carried out in the presented work. Among the studied indicators were the level of postoperative pain syndrome according to VAS, changes in the voice function and act of swallowing, and quality of life indicators assessed by the SF-36 scale.
Assessment of the level of pain syndrome at the short-term postoperative period demonstrated that patients in the MIVAH group had lower pain intensity throughout the entire period of its monitoring. Moreover, the greatest difference was recorded during the first to second days after the intervention compared to the OH group. A decrease in pain syndrome after performing MIVAH was obviously associated with a shorter length of the skin incision and a reduction in the volume of tissue dissection in the anterior neck area stipulated by the possibility of more accurate intraoperative manipulations under conditions of image magnification. In addition, the use of an endoscopic system for visual control of the surgical field improved the conditions for examining areas, which were difficult to access during open surgery.
It is known that a scar on the anterior surface of the neck after thyroid surgery can be a source of certain disorders in the voice function and the act of swallowing even in the absence of specific complications but only due to the development of the adhesion process in the postoperative period. This fact served as the reason for the investigation of the corresponding postoperative disorders in this study. Assessment of changes in the voice function revealed that the differences between the comparison groups were minimal and insignificant according to statistical analysis although generally, the results attested to the advantages of the MIVAH method. Besides, it should be noted that, in our experience, the implementation of MIVAH made it possible to avoid such a complication as intraoperative injury of the recurrent laryngeal nerve with the subsequent development of paresis of the vocal cords. Swallowing disorders were noted by patients less frequently in the MIVAH group, namely by 14.0% and by 8.0% at 1 month and 6 months of follow-up periods, respectively. However, these differences were not significant within the studied volume of clinical material. Thus, one can conclude that hemithyroidectomy in the MIVAH variant has a certain positive effect related to the lower probability of developing voice and swallowing disorders during the postoperative period; however, due to the maintenance of layer-by-layer intersection of structures in the anterior neck area, this effect is lower than after a number of endoscopic operations using extracervical surgical approaches.
The comparison of the quality of life indicators between the patients of the MIVAH and OH groups according to the SF-36 scale demonstrated that the main differences in favor of the MIVAH method were identified at 1 month of the follow-up period after the surgery. Specifically, in the MIVAH group, all indicators responsible for both the physical and psychological components of health were higher; significant differences were recorded towards the criteria of physical functioning, role functioning stipulated by the physical condition, and social functioning. At six months after the operation, there was an increase in all SF-36 scale indicators in both comparison groups, simultaneously with their alignment. Although all indicators in the MIVAH group remained slightly higher than in the OH group, the difference between them became minimal in the absence of significant differences in any of the criteria according to statistical proceeding. These results indicated that hemithyroidectomy performed by the MIVAH method significantly improved the postoperative quality of life of patients but this effect was fully realized only within the early postoperative period. In our opinion, the positive effect of the MIVAH method on the quality of life is based on a decrease in the traumaticity of the operation and a corresponding reduction in the rehabilitation period for patients. However, the retaining of the scar on the anterior surface of the neck does not lead to an increase primarily in the psychological component of health in the long-term postoperative period, compared to operations performed according to the OH method.
Among not abundant works devoted to the analysis of the data on video-assisted thyroid surgery, we have identified several sources that consider the issues of the postoperative period course and the postoperative quality of life in patients. In particular, Chen et al. [10] compared satisfaction with the cosmetic result and the quality of life in patients after video-assisted surgery and robotic thyroidectomy performed according to the method of bilateral axillary-thoracic extracervical access. This study analyzed the results of surgical treatment of 60 and 35 patients, respectively. In terms of the subjective perception of the scar, no significant difference was found between the comparison groups. However, the results of the assessment by the SF-36 scale revealed a number of higher indicators in the group of patients who underwent video-assisted operations, which concerned general health, vitality, and mental health. In another study, Alesina et al. [11] presented the remote cosmetic results of thyroidectomy performed by a video-assisted technique as a component of the postoperative quality of life in patients compared to outcomes of traditional surgery. The studied and control groups included 48 patients each, in which surgeries were performed using the video-assisted technique or the traditional open-access method, respectively. The patient scar assessment scale (PSAS) and the observer scar assessment scale (OSAS) were used to compare the results. The average follow-up time was 31.7±6.4 months for the studied group and 32.9±4.6 months for the control group (p=0.39). The average scar length was 2.6 cm versus 3.8 cm, respectively (p<0.0001). The overall PSAS score was 9.93 versus 9.72 points (p=0.22), while the OSAS score upon determination by an independent surgeon was 13.19 versus 12.33 points, respectively (p=0.01). As a result, the authors conclude that video-assisted surgery did not demonstrate sufficient cosmetic advantages compared with traditional open surgery.
Conclusion
The MIVAH technique, compared to traditional open surgery, demonstrated an enhancement in a number of the postoperative period indicators including the intensity of postoperative pain syndrome and changes in the act of swallowing. After MIVAH, the quality of life in patients was significantly higher in the early postoperative period but in the late postoperative period, the quality of life gained comparable indicators in patients who underwent surgery according to both MIVAH and OH techniques.
References
1. de Vries LH, Aykan D, Lodewijk L, Damen JAA, Borel Rinkes IHM, Vriens MR. Outcomes of Minimally Invasive Thyroid Surgery - A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2021;12:719397. https://doi.org/10.3389/fendo.2021.719397
2. Romashchenko P.N., Maistrenko N.A., Krivolapov D.S., Simonova M.S. Innovative technologies in the diagnosis and safe surgical treatment of thyroid diseases. Bulletin of the Russian Military Medical Academy. 2022;24(1):9-15. (In Russ.) https://doi.org/10.17816/brmma73249
3. Scerrino G, Melfa G, Raspanti C, Rotolo G, Salamone G, et al. Minimally Invasive Video-Assisted Thyroidectomy: Analysis of Complications From a Systematic Review. Surg Innov. 2019;26(3):381-387. https://doi.org/10.1177/1553350618823425
4. Kurganov I.A., Mamistvalov M.Sh., Emel'ianov S.I., Bogdanov D.Iu., Lukianchenko D.V., Agafonov O.A. Minimally invasive video-assisted thyroid surgery technique (results and application features). Endoscopic Surgery. 2020;26(1):13‑20. (In Russ.) https://doi.org/10.17116/endoskop20202601113
5. Matveev I.A., Sipachev N.V., Matveev A., Gibert B.K., Pausova T.I. Features of achieving experience in minimally invasive video-assisted hemithyroidectomy. Medicinskaja nauka i obrazovanie Urala. 2022;23(2)52-56. (In Russ.) https://doi.org/10.36361/18148999_2022_23_2_52
6. Del Rio P, Viani L, Montana CM, Cozzani F, Sianesi M. Minimally invasive thyroidectomy: a ten years experience. Gland Surg. 2016;5(3):295-299. https://doi.org/10.21037/gs.2016.01.04
7. Miccoli P, Fregoli L, Rossi L, Papini P, Ambrosini CE, et al. Minimally invasive video-assisted thyroidectomy (MIVAT). Gland Surg. 2020;9(Suppl 1):S1-S5. https://doi.org/10.21037/gs.2019.12.05
8. Vanushko V.E., Beltsevich D.G., Mel'nichenko G.A., Rumyantsev P.O., Fadeyev V.V. DRAFT: Russian Association of Endocrinologists Clinic Guidelines for Thyroid Nodules Diagnostic and Treatment. Endocrine Surgery. 2015;9(1):15-21. (In Russ.) https://doi.org/10.14341/serg2015115-21
9. Bel’tsevich D.G., Mudunov A.M., Vanushko V.E., Rumiantsev P.O., Mel’nichenko G.A., et al. Differentiated thyroid cancer. Journal of Modern Oncology. 2020;22(4):30-44. https://doi.org/10.26442/18151434.2020.4.200507
10. Chen WH, Chen CY. Postoperative quality of life and cosmetic outcome between minimally invasive video-assisted thyroidectomy and bilateral axillo-breast approach robotic thyroidectomy: a single center retrospective cohort study. Updates Surg. 2021;73(4):1459-1465. https://doi.org/10.1007/s13304-021-01035-1
11. Alesina PF, Wahabie W, Meier B, Hinrichs J, Mohmand W, et al. Long-term cosmetic results of video-assisted thyroidectomy: a comparison with conventional surgery. Langenbecks Arch Surg. 2021;406(5):1625-1633. https://doi.org/10.1007/s00423-021-02196-8
About the Authors
I. A. KurganovРоссия
Igor A. Kurganov - Dr. Sci. (Med.), Associate Professor, associate professor of Department of endoscopic surgery.
Moscow
Competing Interests:
none
M. Sh. Mamistvalov
Россия
Mikhail Sh. Mamistvalov - assistant of the department of endoscopic surgery.
Moscow
Competing Interests:
none
I. S. Usmanov
Россия
Islam S. Usmanov - graduate student of the department of endoscopic surgery.
Moscow
Competing Interests:
none
S. I. Emelyanov
Россия
Sergey I. Emelyanov - Dr. Sci. (Med.), Professor, Corresponding Member of the Russian Academy of Sciences, head of Department of endoscopic surgery.
Moscow
Competing Interests:
none
Review
For citations:
Kurganov I.A., Mamistvalov M.Sh., Usmanov I.S., Emelyanov S.I. Quality of life of patients and distinctive properties of the postoperative period after minimally invasive video-assisted hemithyroidectomy. Medical Herald of the South of Russia. 2024;15(2):33-43. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-2-33-43
JATS XML







































