Scroll to:
Primary ovarian leiomyoma in a patient with uterine leiomyoma
https://doi.org/10.21886/2219-8075-2024-15-1-94-97
Abstract
A small, unilateral tumor. Most ovarian leiomyomas (OLM) are benign, but can range from benign to borderline with malignant degeneration. In many patients, OLM are asymptomatic and are detected accidentally during surgery. In rare cases, OLM can be accompanied by severe symptoms as their size increases. This situation requires differentiation these formations from malignant ovarian tumors, which is more often observed during the perimenopausal and menopausal periods. Being discussed that the source of OLM is smooth muscle blood vessel cells, so more undiagnosed small asymptomatic OLMs can be expected. This article presents a clinical case of OLM in a 39-year-old woman operated for uterine myoma. In the case we presented the coexistence of uterine fibroids and ovarian leiomyoma, which subsequently received diagnostic confirmation.
Keywords
For citations:
Tskhay V.B., Grebennikova E.K., Brekhova I.S., Yametova N.M., Dzhunagova E.Sh. Primary ovarian leiomyoma in a patient with uterine leiomyoma. Medical Herald of the South of Russia. 2024;15(1):94-97. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-1-94-97
Introduction
Uterine leiomyoma (ULM) is the most common benign mesenchymal tumor of the uterus that can develop in any area where smooth muscle cells are found [1]. The broad ligament is the most common and the ovary is one of the rarest extrauterine localizations for ovarian leiomyoma (OLM) [2]. Primary OLM is a very rare benign mesenchymal tumor arising from the smooth muscle of ovarian blood vessel walls [3]. OLM accounts for 0.5–1% of all benign ovarian tumors. Macroscopically and microscopically, OLM is practically indistinguishable from simple ULM [2][4]. In the majority of cases, OLM is observed simultaneously with ULM (78% of cases) [5].
Usually, OLM is a unilateral tumor of small size that is found in patients with ULM [6][7]. At the same time, cases of bilateral ovarian involvement by this tumor were described. In 2004, Lim et al. described a case of a huge bilateral OLM that was not associated with a uterine tumor in a 17-year-old woman. In 2019, Asada et al. reported a second case of bilateral large OLM in a 21-year-old woman [4].
In many patients, OLMs are asymptomatic and are discovered incidentally during surgical intervention. However, they may be accompanied by significant symptoms as their size increases, which necessitates differentiating them from malignant ovarian tumors [5].
OLMs occur in women between the age of 20 and 65 years [1][5]. The available publications contain reports of clinical cases of OLM in both older postmenopausal women [5][6] and in young and even adolescent patients. The literature review shows that, in contrast to elderly patients, adolescent and young women do not usually have concomitant ULM with OLM.
Among the rare variants of OLM described in the literature, one should mention a case described by Japanese authors, in which a large-sized OLM with massive areas of necrosis was reported in a 51-year-old woman [8]. According to computed tomography findings, the dominant feature of the tumor was its cystic component with the presence of a solid component along the dorsal edge of the tumor. Cases of myxoid OLM are also extremely rare variants. Until recently, only two cases of myxoid OLM have been described in the English-language literature [7][8].
The authors of this study did not find articles on OLM cases in domestic sources, and therefore, assume that this publication is of undoubted interest to obstetrician-gynecologists.
Description of the clinical case
A patient, 39 years old, uterine myoma diagnosed within the past year. According to the ultrasound examination, at the time of admission to the hospital, it was established: uterus with dimensions of 68×53×61 mm; the myometrium was changed due to a nodal mass of 84 mm in diameter coming from the posterior wall in the isthmus region, the structure of the nodule was heterogeneous due to the appearance of a hypoechogenic zone with irregular contours with dimensions of 34×19 mm (FIGO type 7-8) and a subserosal myomatous nodule of 55 mm in diameter localized in the uterine fundus (FIGO type 7).
According to the endometrial pipel biopsy performed on the eve of hospitalization, no pathology was detected. Oncomarkers and other laboratory parameters were within normal limits.
The indication for surgical treatment was the presence of uterine fibroid with a large size of one of the nodules and the patient's further reproductive plans. In the course of laparotomy surgery, it was found that the uterine body was slightly enlarged in size. There was a large subserosal myomatous nodule with dimensions of 90×80 mm (FIGO type 7) on the posterior wall of the uterus, the nodule had a wide base (Fig. 1). The left adnexa and right fallopian tube were unchanged. The right ovary was enlarged to 60×50×65 mm due to a dense whitish-colored mass measuring 50×40 mm, resembling a fibroma by its structure (Fig. 2). A linear incision was made over the ovarian mass, through which the mass was removed by morcellation, and bipolar hemostasis was performed.

Figure 1. Intraoperatively: myomatous node (indicated by a black arrow).
Рисунок 1. Интраоперационно: миоматозный узел (указано чёрной стрелкой).

Figure 2. Intraoperative: uterine leiomyoma, ovarian leiomyoma
(indicated by black arrow).
Рисунок 2. Интраоперационно: лейомиома матки, лейомиома в яичнике
(указано чёрной стрелкой).
A histological examination of the uterine myomatous nodule revealed the presence of a typical leiomyoma consisting of bundles of multidirectional smooth muscle fibers, leiomyocytes without signs of cellular atypia, with moderate dystrophic changes, and areas of hyalinosis.
A histological examination of the ovarian mass revealed a tumor consisting of bundles of multidirectional smooth muscle fibers, leiomyocytes without signs of cellular atypia, normochromic, with moderate dystrophic changes, with areas of small focal hyalinosis in Van Gieson staining with fibrous tissue overgrowth. This histological picture was characteristic of OLM (Fig. 3).
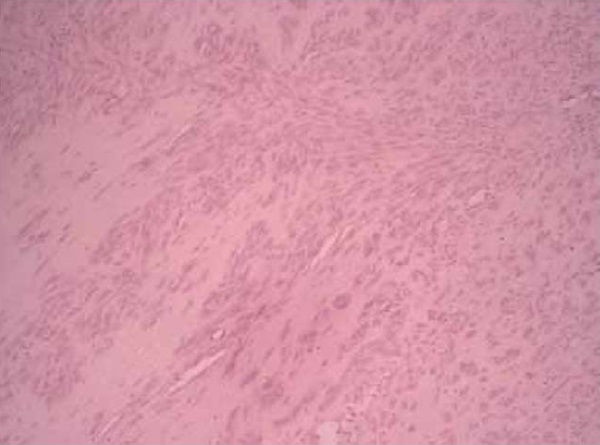
Figure 3. Histological structure of leiomyoma in the ovary (Van Gieson staining).
Рисунок 3. Гистологическое строение лейомиомы в яичнике (окраска по Ван-Гизону).
The histologic report said that there was a morphologic picture of typical ULM and OLM. The final diagnosis was: “Uterine leiomyoma and ovarian leiomyoma”. The postoperative period of the patient proceeded without complications. She was discharged from the hospital on the 4th day in a satisfactory condition.
Discussion
A systematic review of the literature revealed fewer than 100 reports of primary OLMs, with some cases showing residual ovarian tissue. Up to 85% of OLMs are detected in premenopausal women [1][5][6]. Clinical manifestations of OLMs are mainly manifested by symptoms such as unilateral lower abdominal pain or menstrual irregularities. Sonograms usually show large tumors measuring 5–15 cm with normal content of CA-125 oncomarker. It is discussed that smooth muscle cells of blood vessels are the source of OLM, so one can expect more undiagnosed small asymptomatic OLMs.
OLMs are often discovered incidentally either during surgery for uterine fibroid or ovarian tumors. Since clinical symptoms tend to develop when the mass is large, these symptoms are not specific. In the case described here, the coexistence of uterine myoma and OLM was presented, which was subsequently diagnostically confirmed.
Surgery is important in the treatment of OLM, and it is important to consider the age of the patient when choosing the extent of surgical intervention. For example, in postmenopausal or middle-aged women who are not fertile or do not wish to preserve their fertility, bilateral salpingo-oophorectomy is the best option. In the considered case, the patient was at a relatively young age and expressed a desire for subsequent childbearing, so the most organ-sparing extent of surgery was chosen on both the uterus and the affected ovary.
Conclusion
Most OLMs are benign in nature, but can range from benign to borderline with malignant degeneration [6][8]. Rare cases of malignant ovarian neoplasm, particularly cases of malignant primary ovarian leiomyosarcoma, were described in the literature, so careful preoperative diagnostic measures are necessary.
References
1. Bharti S, Khera S, Sharma C, Balakrishnan A. Unilateral primary ovarian leiomyoma masqueraded as ovarian fibroma: A histopathological diagnosis. J Family Med Prim Care. 2021;10(9):3494-3497. https://doi.org/10.4103/jfmpc.jfmpc_2546_20
2. Thombare P, Chheda P, Parikh R, Shetty R, Verma M, Patkar D. Primary ovarian leiomyoma: Imaging in a rare entity. Radiol Case Rep. 2020;15(7):1066-1070. https://doi.org/10.1016/j.radcr.2020.04.058
3. Kitamura Y, Ito F, Kokabu T, Mori T, Kusuki I, Kitawaki J. Primary Ovarian Leiomyoma Associated with Multiple Uterine Leiomyomas. Gynecol Minim Invasive Ther. 2021;10(1):50-52. https://doi.org/10.4103/GMIT.GMIT_97_19
4. Asada T, Yamada T, Kumano R. Primary ovarian leiomyoma with predominant cystic change. Radiol Case Rep. 2019;14(11):1315-1319. https://doi.org/10.1016/j.radcr.2019.08.012
5. Liang G, Wu Z, Zhu L, Ruan F. Case Report: Primary Ovarian Leiomyoma: A Clinical Analysis of Case Series and Literature Review. Front Med (Lausanne). 2022;9:822339. https://doi.org/10.3389/fmed.2022.822339.
6. Alshwairikh K, Al Otaibi W, Alshammari S, Alshammari T, Hakami R, et al. Cystic Ovarian Leiomyoma in a Patient with Progressive Abdominal Pain. Am J Case Rep. 2021;22:e930299. https://doi.org/10.12659/AJCR.930299
7. Pervan M, Gembicki M, Princk H, Rody A, Hanker L, et al. Primary ovarian leiomyoma: a rare ovarian tumour. Arch Gynecol Obstet. 2023;308(4):1379-1380. https://doi.org/10.1007/s00404-022-06842-4
8. Wang QM, Zhao Y, Ma Y, Yao LT, Han X. One case report of giant atypical leiomyoma of the ovary. Medicine (Baltimore). 2018;97(40):e12526. https://doi.org/10.1097/MD.0000000000012526
About the Authors
V. B. TskhayРоссия
Vitaly B. Tskhay, Dr. Sci. (Med.), Professor, Head of the Department of Perinatology, Obstetrics and Gynecology, Faculty of Medicine
Krasnoyarsk
E. K. Grebennikova
Elvira K. Grebennikova, Cand. Sci. (Med.), Associate Professor of the Department of Perinatology, Obstetrics and Gynecology, Faculty of Medicine
Krasnoyarsk
I. S. Brekhova
Irina S. Brekhova, Cand. Sci. (Med.), Associate Professor of the Department of Perinatology, Obstetrics and Gynecology, Faculty of Medicine
Krasnoyarsk
N. M. Yametova
Natalya M. Yametova, assistant at the Department of Perinatology, Obstetrics and Gynecology, Faculty of Medicine
Krasnoyarsk
E. Sh. Dzhunagova
Eliza Sh. Dzhunagova, obstetrician-gynecologist, gynecology department
Krasnoyarsk
Review
For citations:
Tskhay V.B., Grebennikova E.K., Brekhova I.S., Yametova N.M., Dzhunagova E.Sh. Primary ovarian leiomyoma in a patient with uterine leiomyoma. Medical Herald of the South of Russia. 2024;15(1):94-97. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-1-94-97
JATS XML







































