Scroll to:
Development of idiopathic intracranial hypertension on the background of zoledronic acid therapy in Gorham-Stoat syndrome
https://doi.org/10.21886/2219-8075-2023-14-3-46-50
Abstract
Idiopathic intracranial hypertension (IVH) is a condition or a heterogeneous group of vessels characterized by an increase in intracranial pressure (ICP) without signs of mass formation, hydrocephalus, infection, venous thrombosis, and hypertensive encephalopathy. The term "pseudotumoral cerebral hypertension" is used to describe the secondary origin of ICP due to various causes and is a diagnosis of exclusion. One of the risk factors for the development of IVH are hypocalcemic conditions of the development of etiology, leading to the development of ICP. Long-term use of zoledronic acid, which is a risk factor for the development of hypocalcemia, can contribute to the occurrence and fluctuating course of IVH, requires monitoring clinical monitoring of the patient's condition in order to prevent the occurrence of secondary atrophy of the optic discs, with further progressive decline and loss of vision. The choice of vaccine for a 12-year-old child with a clinically-instrumentally-histologically confirmed diagnosis of Gorham-Stout syndrome, with progressive bone resorption, receiving zoledronic acid therapy. Attracting the attention and informing a wide range of specialists in various fields about the likelihood of IVH on the background of long-term use of bone and cartilage metabolism correctors can serve as an important factor in the timely diagnosis, prevention and correction of this pathological condition in childhood.
Keywords
For citations:
Domracheva A.M., Fomina-Chertousova N.A., Sozaeva D.I. Development of idiopathic intracranial hypertension on the background of zoledronic acid therapy in Gorham-Stoat syndrome. Medical Herald of the South of Russia. 2023;14(3):46-50. (In Russ.) https://doi.org/10.21886/2219-8075-2023-14-3-46-50
Introduction
Idiopathic intracranial hypertension (IIH) is a pathological condition characterized by increased intracranial pressure without identification of a space-occupying formation, signs of thrombosis, or an infectious process [1].
IIH has gender differences with a ratio from 2:1 to 8:1 for women and men, respectively, which are absent in the juvenile period and very rare in infancy. The incidence of the disease among obese women of childbearing age is 19–21 cases per 100,000 of the population, while the overall incidence is 1–2 per 100,000 people [2]. Children account for 37% of cases of the disease and 90% of them with predominance in children 5–15 years old [3].
Currently, it is recommended to make a diagnosis of IIH according to Dandy’s criteria, adapted by Friedman (2013) [4].
The diagnosis of IIH is considered definite if the following manifestations are present:
a) swelling of the optic discs;
b) absence of deviations in the neurological status excluding injury in the abducens nerve;
c) normal brain structure under neuroimaging, without evidence of hydrocephalus, a space-occupying formation or focal lesion, changes in the meninges, and signs of sinus thrombosis;
d) absence of deviations in the composition of the cerebrospinal fluid;
e) increase in cerebrospinal fluid pressure during lumbar puncture, performed without technical errors in the lateral decubitus position, ≥250 mm of water column (normalcy for children and adults is 100–150 mm of water column) [5].
The diagnosis is considered probable if items a–d are fulfilled, but the cerebrospinal fluid pressure is below 250 mm H2O column. In the absence of optic disc edema, the diagnosis of IIH can be made if criteria b–d are met and, in addition, the patient has unilateral or bilateral abducens neuropathy [6].
The most common condition with a proven association with IIH development in adults is excess body weight leading to two realization mechanisms:
1. IIH theory. It is based on the physical effects of increased abdominal mass, causing an increase in intra-abdominal and intrathoracic (pleural) pressure, as well as cardiac filling pressure. In return, these effects contribute to the obstruction of venous outflow from the brain and, consequently, an increase in intracranial pressure.
2. Hormonal theory. Adipocytes convert androstenedione (a precursor of sex hormones) to estrone, which leads to an increase in the production of cerebrospinal fluid by the choroid plexus and the emergence of intracranial pressure [1].
There is also a hypothesis indicating the role of aquaporins, which are membrane proteins responsible for the selective diffusion of water molecules, in IIH pathogenesis. Aquaporin-1 or the “water protein channel” is widely distributed in human brain cells and regulates the secretion and outflow of water within the subarachnoid space. Overexpression of aquaporin-1 causes an increase in intracranial pressure; drugs, which reduce its expression level, contribute to the weakening of clinical symptoms and decrease the risk of IIH development. Conditions, presumably associated with IIH development, include hypervitaminosis A and the administration of capron and lindane [7].
When studying the mechanisms of IIH development in children, the metabolic theory has become most widespread. Intracranial hypertension has been described upon total thyroidectomy and levothyroxine sodium replacement therapy for juvenile hypothyroidism. It has been suggested that rapid correction of hypothyroidism disrupts sodium metabolism and leads to changes in the dynamics of cerebrospinal fluid production [8]. Older children with excess body weight have been found to be more likely to suffer from IIH than children of younger age groups. Cases of IIH have been described upon abrupt cessation of corticosteroids in children with inflammatory bowel diseases. The prevalence of pathology in children receiving recombinant (biosynthetic) human growth hormone (GH) was 100 times higher than in the general population. Moreover, the proposed mechanism for its realization includes GH, which passes through the blood-brain barrier and increases the production of cerebrospinal fluid from the choroid plexus by raising the level of insulin-like growth factor-1 [8].
Gorham-Stout syndrome, or “vanishing bone disease”, or phantom bone disease, or idiopathic progressive massive osteolysis, is a rare disease of unknown etiology, characterized by the abnormal proliferation of thin-walled capillaries and small lymphatic vessels in bone structures, followed by massive osteolysis of the adjacent bone [9].
Description of a clinical case
Female patient P., 12 years old, was admitted to the neurological center of the Federal State Budgetary Institution of Higher Education “Rostov State Medical University” of the Ministry of Health of Russia with complaints about periodic headaches of a diffuse nature, mainly in the morning, accompanied by nausea, with a frequency of 2–3 times a month, as well as a first-time acute episode of double vision in the horizontal plane with both eyes, which self-regressed within 2 weeks.
Life history. The child was born from the 1st pregnancy, which occurred against the background of a threat of miscarriage in the 1st half; it was the 1st planned birth at a gestational age of 38–39 weeks by a cesarean section, with a double tight entanglement of the umbilical cord around the neck; body weight was 3200 g, length was 50 cm, and Apgar score was 8–9 points. In subsequent age periods of childhood, she grew and developed according to her age.
History of the disease. At the age of 10 years (June 2020), the child first developed noise in the left ear, and therefore, an MRI of the brain was performed. In the projection of the left cerebellopontine angle, MRI revealed an extracerebral formation measuring 13.0×11.0×12.5 mm without significant extension into the internal auditory canal with the following features: round in shape, with clear uneven contours, homogeneous liquid structure, with the presence of septa, adjacent to the dura mater shell, without perifocal edema and mass effect, without accumulating contrast (Figure 1).

Figure 1. MRT of the brain of a girl P., 12 years old, June 2020.
To clarify the diagnosis, the girl’s mother independently sought advice from the Department of Radiation Diagnostics of Children of the Russian Medical Academy of Continuing Professional Education (RMANPO), Moscow (February 2021). According to the conclusion of specialists, the clinical picture of the disease, and expert assessment of neuroimaging data, there was a formed opinion in favor of the endocrine genesis of the identified changes with the demand to clarify the diagnosis in the conditions of the National Medical Research Center for Endocrinology of the Federal State Budgetary Institution of the Ministry of Health of the Russian Federation, Moscow. Totally, neuroimaging data included the following items: the presence of areas of lytic destruction of the right parietal bone filled by cystic contents with a hemorrhagic component (“chocolate cysts”); a destructive cavity with cystic formations having soft tissue septa; without accumulation of a contrast agent at the apex of the pyramid of the left temporal bone; moderate deformation of the lower jaw with a sharp change in its structure due to the presence of multiple areas of lytic destruction with the formation of cysts and destruction of the cortical layer (Figure 2).
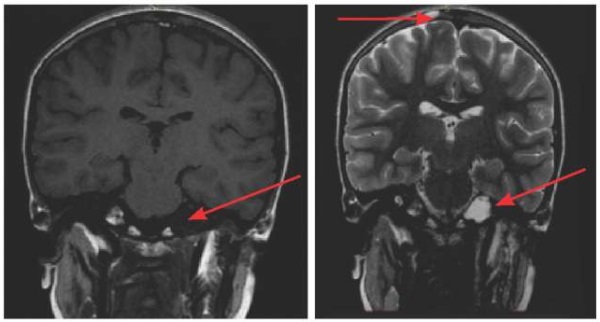
Figure 2. MRT of the brain of a child P., 12 years old.
Multiple foci of lytic destruction with hemorrhagic component (“chocolate cysts”).
Based on the results of the examination (March 2021), the girl was diagnosed with primary hypothyroidism; she was recommended to take eutyrox 25 mg/day and consult a neurosurgeon to clarify the patient’s management tactics and verify the identified pathological foci of the bone structures in the skull.
Subsequently, during the examination at the National Medical Research Center of Oncology (NMRC) in Rostov-on-Don (June 2021), spiral computed tomography (SCT) of the facial part of the skull, abdominal and pelvic organs revealed multiple foci of bone tissue destruction ranging in size from 6.1×9.4×9.3 mm to 10.4×12×20 mm, signs of polyostotic form of fibrous dysplasia of the right ilium, left femoral neck and ribs, respectively (Figure 3).

Figure 3. SCT of a 12-year-old child of the facial part of the skull (a),
abdominal cavity (b), and right iliac bone (c)
For histological verification of the identified lesions, the child underwent resection craniotomy of the right parietal region with microsurgical removal of the formation. Analysis of biopsy material in the conditions of the Russian Children’s Clinical Hospital (RCCH) in Moscow (October 2021) made it possible to establish the diagnosis of Gorham-Stout syndrome with progressive bone tissue resorption, and therefore a course of treatment with zoledronic acid was recommended in a regimen of 3 mg intravenously by drop infusion once every 3 months against the background of constant immunosuppression with sirolimus 2 mg/day.
After 5 courses of therapy with zoledronic acid, the child experienced first an episode of horizontal double vision in both eyes (September 2022), which was self-regressed. Repeated ophthalmoscopy revealed a variety of clinical interpretations of the fundus picture: from signs of pseudocongestive optic discs to the formation of a complete picture of optic disc congestion in both eyes while maintaining normal visual acuity.
Discussion
Considering the child’s complaints and the results of dynamic ophthalmoscopy, it was requisite to perform a lumbar puncture to determine the parameters of intracranial pressure, general biochemical indices of the cerebrospinal fluid, and indices of oligoclonal IgG antibodies both in cerebrospinal fluid and blood serum, as well as determine the blood electrolyte composition, in particular the levels of total calcium, ionized calcium, and phosphorus, with additional assessment of blood serum alkaline phosphatase and antibodies to aquaporin-4 for the purpose of differential diagnosis of IIH against the background of hypocalcemia during therapy with zoledronic acid and demyelinating disease. The cerebrospinal fluid pressure during lumbar puncture corresponded to the age norm (60 drops/min.). According to the results of that investigation, a demyelinating disease in the child was excluded as antibodies to aquaporin-4 in the blood serum were less than 1:10 (normalcy <1:10) although conducted tests revealed type 1 of the synthesis of oligoclonal IgG in the cerebrospinal fluid and blood serum. The investigation of the electrolyte composition of the blood did not reveal a hypocalcemic state as total calcium was 2.45 mmol/l (normalcy 2.25–2.75 mmol/l), ionized calcium was 1.08 mmol/l (normalcy 1.07–1.35 mmol/l), phosphorus was 1.16 mmol/l (normalcy 0.87–1.45 mmol/l), and alkaline phosphatase was 270.0 U/l (normalcy 180–1200 U/l); all that, however, did not exclude transient hypocalcemia passing at earlier stages of the disease.
During the ophthalmological examination during that hospitalization, no data on the pathology of the optic disc were obtained: the thickness of the layer of nerve filament was within the age norm, and the disc excavation profile was physiological. The child was recommended for dynamic clinical monitoring after 6 months with using optical coherence tomography devices designed for examining pediatric patients.
Conclusion
Thus, based on the complex clinical, instrumental, and laboratory examinations, it can be concluded that currently, the child does not have IIH syndrome. However, considering the expectation of transient hypocalcemia caused by the long-term administration of zoledronic acid, leading to the emergence of IIH and its fluctuating course, it is advisable to inform a wide range of pediatric specialists about the probability of occurrence of this pathological condition, its timely diagnosing, correction, and formation of a follow-up plan in order to prevent a progressive decline and loss of visual acuity due to the secondary atrophy of the optic nerves in this group of children.
References
1. Sergeev AV. Idiopathic intracranial hypertension. Zhurnal Nevrologii i Psikhiatrii imeni S.S. Korsakova. 2016;116(5):93‑97. (In Russ.) https://doi.org/10.17116/jnevro20161165193-97
2. Greenberg MS. Handbook of neurosurgery. New York: Thieme; 2020.
3. Ko MW, Liu GT. Pediatric idiopathic intracranial hypertension (pseudotumor cerebri). Horm Res Paediatr. 2010;74(6):381-9. https://doi.org/10.1159/000321180
4. Parkhomenko E.V., Nartov S.E., Barinov A.N., Karpov D. Yu., Sorokina E.A. Problem of diagnosis and treatment of idiopathic intracranial hypertension. Medical alphabet. 2017;2(15):5-13. (In Russ.) eLIBRARY ID: 30674744
5. Guzeva V.I., ed. Federal Guide to Child Neurology. Moscow: Special Publishing House of Medical Books; 2016. (In Russ.)
6. Petrayevskiy AV, Trishkin KS, Gndoyan IA, Lomakina VE, Adelshina NA. Idiopathic intracranial hypertension (case study). Vestnik Oftalmologii. 2021;137(5):122‑129. (In Russ.) https://doi.org/10.17116/oftalma2021137051122
7. Stiebel-Kalish H, Eyal S, Steiner I. The role of aquaporin-1 in idiopathic and drug-induced intracranial hypertension. Med Hypotheses. 2013;81(6):1059-62. https://doi.org/10.1016/j.mehy.2013.10.002
8. Ioyleva E.E., Markova E.Y., Bondarenko M.A. Bilateral optic nerve swelling after thyroidectomy followed by a course of radioiodine therapy. Acta Biomedica Scientifica. 2018;3(1):125-129. (In Russ.) https://doi.org/10.29413/ABS.2018-3.1.20
9. Kryukov AI, Karpova EP, Toropchina LV, Zelikovich EI, Rogozhin DV, Donyush EK. Unilateral subjective tinnitus «vanishing bone» disease (Goram—Stout syndrome). Vestnik Oto-Rino-Laringologii. 2022;87(5):92‑98. (In Russ.) https://doi.org/10.17116/otorino20228705192
About the Authors
A. M. DomrachevaРоссия
Anastasia M. Domracheva - resident of the 2nd year of the Department of Nervous Diseases and Neurosurgery, Rostov State Medical University.
Rostov-on-Don
Competing Interests:
None
N. A. Fomina-Chertousova
Россия
Neonila A. Fomina-Chertousova - Cand. Sci. (Med.), Associate Professor of the Department of Nervous Diseases and Neurosurgery, Rostov State Medical University.
Rostov-on-Don
Competing Interests:
None
D. I. Sozaeva
Россия
Diana I. Sozaeva - Dr. Sci. (Med.), Associate Professor, Department of Neurology and Neurosurgery, Rostov State Medical University.
Rostov-on-Don
Competing Interests:
None
Review
For citations:
Domracheva A.M., Fomina-Chertousova N.A., Sozaeva D.I. Development of idiopathic intracranial hypertension on the background of zoledronic acid therapy in Gorham-Stoat syndrome. Medical Herald of the South of Russia. 2023;14(3):46-50. (In Russ.) https://doi.org/10.21886/2219-8075-2023-14-3-46-50
JATS XML







































