Scroll to:
Effect of combined antioxidant and photodynamic therapy on the emotional state of patients with vulvar craurosis
https://doi.org/10.21886/2219-8075-2023-14-1-5-12
Abstract
Objective: studying of the effect of combined antioxidant and photodynamic therapy (PDT) on the emotional state of patients with vulvar kraurosis.
Materials and methods: the study involved 90 women with vulvar kraurosis who were randomized into three groups of 30 participants. In the first group, treatment included photodynamic therapy (PDT) followed by administration of the antioxidant Ethylmethylhydroxypyridine succinate for one month. Participants in the second group received only PDT. Patients of the third group underwent a course of laser therapy on the perineal region. The emotional state of the participants was assessed using the Hospital Anxiety and Depression Scale (HADS) before and at the end of treatment, 1, 6 and 12 months after the end of therapy.
Results: before treatment, participants from the three groups scored a similar number of HADS scores. In the course of observations, the best result on the scales of anxiety and depression was recorded in patients who received combined antioxidant and photodynamic therapy. After a month of taking Ethylmethylhydroxypyridine succinate, the HADS score in these women was significantly lower than in the comparison groups. Further, these patients continued to show better scores on the depression scale. The total scores on the anxiety scale in this group were comparable to those in patients who received only PDT.
Conclusion: combined antioxidant and photodynamic therapy, including Ethylmethylhydroxypyridine succinate, has a more pronounced positive effect on the emotional background of patients with vulvar kraurosis in comparison with PDT and laser therapy.
For citations:
Kiseleva E.A., Makhmutkhodzhaev A.Sh., Mikheenko G.A. Effect of combined antioxidant and photodynamic therapy on the emotional state of patients with vulvar craurosis. Medical Herald of the South of Russia. 2023;14(1):5-12. (In Russ.) https://doi.org/10.21886/2219-8075-2023-14-1-5-12
Introduction
Vulvar craurosis is characterized by a long recurrent course and distressing symptoms: itching, pain, and discomfort in the external genital area [1–7]. In the presence of somatic sufferings, an integral part of the general clinical picture of craurosis becomes an impairment of the emotional sphere of patients [7–9].
The depressed psychological state of female patients can become pathological up to the development of anxiety and depressive disorders [10]. According to Kolitz et al., 21% of patients with craurosis have comorbid anxiety or depression [11], which is consistent with the result of a survey of the British Association of Dermatologists: every fifth woman with vulvar disease thought about suicide or self-harm because of her condition [12]. According to another study, anxiety and depression are much more common in female patients with craurosis: 68.4% and 75.4%, respectively [7].
Improving the quality of life [13–16] and psycho-emotional state of patients with craurosis is an important clinical task. Based on the resources and opportunities available to the obstetrician-gynecologist, the solution to this problem implies the formation of a trusting contact with the patient, providing her with relevant information support regarding her disease [17–19] and, of course, individual selection of effective and safe therapy for craurosis [20–27].
The aim of the study was to investigate the effect of combined antioxidant and photodynamic therapy (PDT) on the emotional state of patients with vulvar craurosis.
Materials and Methods
This prospective randomized controlled experimental clinical trial was conducted in accordance with international GCP standards. It involved 90 patients who underwent examination and treatment for vulvar craurosis (syn. sclerotic vulvar lichen, ICD-10 code – N90.4) in the gynecological department of the Tomsk Regional Clinical Hospital (Tomsk) and the Perinatal Health Center (Tomsk) in the period from 2017 to 2020.
The criteria for inclusion in the study were the presence of a histologically confirmed diagnosis of vulvar craurosis in the postmenopausal period of over 5 years and informed voluntary consent for participation in the study and medical intervention.
The criteria for exclusion from the study were the presence of histologically confirmed combination of vulvar craurosis with other vulvar pathology, including cancer, detection of decompensated somatic pathology and acute inflammatory diseases at the time of the study, gynecologic pathology requiring surgical treatment, contraindications for laser therapy, PDT, and administration of ethylmethylhydroxypyridine succinate, as well as the patient's refusal to participate in the study.
Using the method of pseudorandom number generation, the patients included in the study were randomized into three groups of 30 participants each. In the first group, women underwent one PDT session [28] using 0.5% Radachlorin® gel (RADA-PHARMA® LLC, Russia). Pathologic foci were irradiated in pulsed mode, the radiation wavelength was 662 nm, the output power of the light source was 2 W, and the energy density was 200 J/cm2. The duration of the procedure was 15–40 minutes. In each case, it was calculated individually and depended on the lesion area.
Seven days after PDT, patients received antioxidant therapy [29] with ethylmethylhydroxypyridine succinate 125 mg 3 times a day for 1 month. This drug, in addition to antioxidant properties, also has anxiolytic, stress-protective, and nootropic effects.
In Group II, patients received one session of PDT (the procedure corresponded to that in Group I) without further prescription of antioxidant therapy. In Group III, patients received 10 sessions of laser therapy on the perineal area.
All patients answered the Hospital Anxiety and Depression Scale (HADS) questions before treatment (first visit), seven days after PDT in Groups I and II, and immediately after laser therapy in Group III (second visit), and at 1, 6, and 12 months after the second visit (3rd, 4th, and 5th visits, respectively). The results were processed according to the questionnaire instructions: anxiety and depression levels were assessed separately from each other; a score of 0–7 points meant no signs of anxiety/depression, a sum of 8-10 points corresponded to subclinically expressed anxiety/depression, and 11 or more points corresponded to clinically expressed anxiety/depression [30].
The results of this questionnaire survey are not a diagnosis and are used for screening by physicians of all specialties. Patients with subclinical or clinically significant anxiety and/or depression on the Hospital Anxiety and Depression Scale were recommended to consult a psychiatrist.
The obtained data were processed using the program STATISTICA 8.0 (StatSoft, USA). The normality test was performed using the Kolmogorov-Smirnov test. Quantitative continuous data were presented as the mean and standard deviation (SD), ordinal variables as the median (Me) and interquartile range (Q1; Q3), and qualitative variables as percentage (%).
A comparison of quantitative variables in independent groups was performed using the Mann-Whitney test, in dependent groups – using the Wilcoxon test. A comparison of groups on qualitative variables was performed using Fisher’s exact test. Differences between groups were considered statistically significant at p<0.05.
Results
The participants of the study groups were comparable in terms of medical, social, and clinical characteristics. The mean age of the patients was 62±5 years old (52 to 75 years old). All women were postmenopausal, with a mean duration of 12±5 years (6 to 31 years). The mean disease duration was defined as 8±5 years (1 to 22 years).
Before treatment, the participants of the three groups scored similarly on the anxiety scale (Table 1), with 19 (63.3%) women in Group 1, 17 (56.7%) in Group 2, and 17 (56.7%) in Group 3 (p1=0.16, p2=0.16) having a sum of scores corresponding to subclinically expressed anxiety (see Graph 1).
Table 1
Hospital Anxiety and Depression Scale (HADS), anxiety scale, scores, Me (Q1; Q3)
|
Visit |
Anxiety Scale |
||
|
Group 1 n=30 |
Group 2 n=30 |
Group 3 n=30 |
|
|
Before treatment |
8 (7; 9) |
8 (7; 9) p1=1 |
8 (7; 9) p2=0.9 |
|
After treatment |
6 (5; 7) |
6 (5; 7) p1=0.6 |
4 (3; 5) p2<0.00001 |
|
1 month after treatment |
3 (2; 3) |
5 (4; 5) p1<0.00001 |
5 (5; 6) p2<0.00001 |
|
6 months after treatment |
6 (5; 6) |
6 (5; 6) p1=0.72 |
7 (7; 8) p2<0.00001 |
|
12 months after treatment |
6 (6; 7) p3<0.00001 |
7 (6; 7) p1=0.31 p3=0.000043 |
8 (7; 8) p2<0.00001 p3=1 |
Note: Me — median; Q1 and Q3 — quartiles; n — sample size; p1 — significance of differences in comparison between Groups 1 and 2; p2 — significance of differences in comparison between Groups 1 and 3; p3 — significance of differences in comparison between data before treatment and 12 months after treatment within the same group.
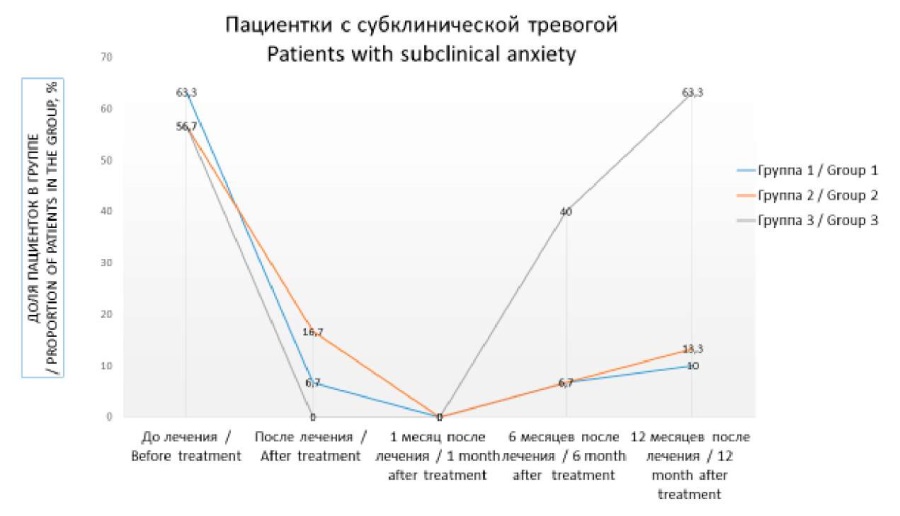
Fig. 1. Patients with subclinical anxiety
Immediately after treatment, all groups showed a decrease in anxiety scale scores. Patients from Group 1 showed the lowest values of this indicator after one month of taking ethylmethylhydroxypyridine succinate. At the end of the therapeutic course with this drug, the sum of anxiety scale scores in these participants began to increase and did not differ significantly from the corresponding data in Group 2.
In Group 3, a significant decrease in the number of anxiety scale scores was observed immediately after therapy, but then this index increased and reached its initial values after 12 months. At the same time, in Groups 1 and 2, where patients received PDT, the level of anxiety 12 months after treatment was lower than before treatment. The number of patients with subclinical anxiety scores at 6 and 12 months after treatment was 2 (6.7%), 2 (6.7%), 12 (40%) (p1=1, p2=0.002) and 3 (10%), 4 (13.3%), 19 (63.3%) (p1=0.69, p2<0.00001) for Groups 1, 2, and 3, respectively.
The sums of scores on the depression scale before the start of treatment did not differ between the groups (Table 2). The number of points corresponding to subclinical depression was 14 (46.7%) in Group 1, 13 (43.3%) in Group 2, and 12 (40%) in Group 3 (p1=0.33, p2=0.16) (Fig. 2).
Table 2
Hospital Anxiety and Depression Scale (HADS), Depression scale, scores, Me (Q1; Q3)
|
Visit |
Depression Scale |
||
|
Group 1 n=30 |
Group 2 n=30 |
Group 3 n=30 |
|
|
Before treatment |
7 (6; 8) |
7 (6; 8) p1=0.92 |
7 (7; 8) p2=0.7 |
|
After treatment |
5 (4; 5) |
5 (4; 6) p1=0.8 |
4.5 (4; 5) p2=0.07 |
|
1 month after treatment |
2 (2; 2) |
4 (3; 4) p1<0.00001 |
5 (5; 6) p2<0.00001 |
|
6 months after treatment |
5 (4; 5) |
6 (5; 6) p1=0.002 |
7 (7; 7) p2<0.00001 |
|
12 months after treatment |
6 (5; 6) p3<0.00001 |
7 (6; 7) p1=0.00016 p3=0.0269 |
7 (7; 8) p2<0.00001 p3=0.72 |
Note: Me — median; Q1 and Q3 — quartiles; n — sample size; p1 — significance of differences in comparison between Groups 1 and 2; p2 — significance of differences in comparison between Groups 1 and 3; p3 — significance of differences in comparison between data before treatment and 12 months after treatment within the same group.

Fig. 2. Patients with subclinical depression
Immediately after treatment, the patients of the three groups showed a decrease in the sum of depression scale scores, with no significant differences between the groups. One month after treatment, the participants of Group 1 who took ethylmethylhydroxypyridine succinate demonstrated the most pronounced dynamics of depression scale score reduction. At follow-up visits, these patients also scored statistically significantly lower depression scale scores than participants in the comparison groups.
At 6 months after treatment, 2 (6.7%), 1 (3.3%), and 7 (23.3%) (p1=0.55, p2=0.038) women from Groups 1, 2, and 3, respectively, and at 12 months – 2 (6.7%), 3 (10%), and 11 (36.7%) (p1=0.64, p2=0.007) participants from Groups 1, 2, and 3, respectively.
Discussion
There are very few studies describing changes in the emotional sphere of patients with vulvar craurosis in both domestic and international medical publications. All studies devoted to this topic note a pronounced negative impact of painful chronic symptoms of this disease on the psychological state of patients [7–12]. Having studied freely available publications covering aspects of etiopathogenesis, clinical course, diagnostics, and therapy of craurosis, the authors of the article did not find any scientific work devoted to the fact that, perhaps, different methods of treatment of this disease may have a different impact on the emotional background of patients. Thus, this study is the first to investigate and demonstrate the dependence of the emotional state of patients with vulvar craurosis on the method of therapy used.
The study showed that in comparison with a course of laser therapy, PDT demonstrated a slower, but at the same time more pronounced and persistent positive effect on the psycho-emotional sphere of women with vulvar craurosis. This effect was even more pronounced when combining PDT and course administration of ethylmethylhydroxypyridine succinate. A significant positive effect of the drug on mood is maintained as long as the patient continues to take it. Further, on completion of the course of antioxidant therapy, the positive effect of ethylmethylhydroxypyridine succinate on the level of depression slightly decreases, but persists for a long time. The effect of the drug on the level of anxiety is leveled off almost immediately after withdrawal of the drug.
It was noted that in Groups 1 and 2, where patients received PDT, the number of participants with subclinical forms of anxiety and depression at 6 and 12 months after treatment was significantly lower than in the group where laser therapy was performed. Administration of ethylmethylhydroxypyridine succinate had no significant effect on the incidence rate of subclinical forms of anxiety and depression both in the short- and long-term (up to 12 months of follow-up) period.
Scientific Novelty
This work has both practical and scientific components. For the first time, the influence of the method of treatment of vulvar craurosis on the emotional state of patients was considered. It was noted that the positive effect on the emotional sphere of the patients came quickly, but lasted for a short time. At the same time, PDT in comparison with laser therapy had a slowly developing but better long-term effect on anxiety and depression. Additional administration of ethylmethylhydroxypyridine succinate can significantly accelerate the stabilization of the emotional background of patients after PDT.
Hospital scale of anxiety and depression demonstrated its clinical significance for assessing the emotional state of patients with vulvar craurosis, including in dynamics against the background of treatment.
Practical Significance
From a practical point of view, the Hospital Anxiety and Depression Scale can be recommended in obstetric and gynecological practice for rapid dynamic assessment of the emotional status of patients with vulvar craurosis. The results of HADS can be used for the individualized choice of the optimal treatment of craurosis, taking into account in each case not only the effectiveness of the method of therapy in relation to lesions of vulvar tissues but also its impact on the psycho-emotional sphere of the patient.
Combined photodynamic and antioxidant therapy can be recommended for practical application. The method has a rapidly developing, pronounced positive effect on the levels of anxiety and depression of patients, which is achieved due to the high clinical efficacy of this treatment in relation to the manifestations of craurosis and good control of the symptoms of the disease, as well as due to the additional anxiolytic effect of the antioxidant used.
Conclusion
Stabilization of the emotional background of patients with vulvar craurosis is one of the aspects of the success of therapy and a guarantee of good adherence of the patient to this or that method of treatment. Despite the fact that obstetrician-gynecologists in their routine practice are engaged in the treatment of genital pathology, they cannot fail to note the special psycho-emotional state of women with craurosis, daily facing the painful symptoms of their disease.
Given the fact that, as a rule, women with craurosis do not address their emotional problems caused by somatic pathology to specialized specialists, the obstetrician-gynecologist often has the additional task of providing emotional support to patients. This emotional support can be provided not only by "words", informing the woman about the peculiarities of her disease but also by "deeds" – by selecting the optimal treatment, which effectively manages the symptoms of craurosis and gives the patient hope for a decent quality of life in the future.
This study found that combined photodynamic and antioxidant therapy compared to PDT and laser therapy demonstrated better short- and long-term results in terms of anxiety and depression levels in patients with vulvar craurosis. Ethylmethylhydroxypyridine succinate, administered after PDT as a pathogenetic antioxidant drug and as a means to improve the emotional background of the patients, can significantly improve treatment outcomes. Thus, ethylmethylhydroxypyridine succinate can be recommended for complex therapy of vulvar craurosis in combination with PDT.
References
1. Gagne H, Dalton V, Haefner H, Patel DA. Vulvar pain and sexual function in patients with lichen sclerosus. J Reprod Med. 2007;52:121-122.
2. Haefner HK, Aldrich NZ, Dalton VK, Gagné HM, Marcus SB, et al. The impact of vulvar lichen sclerosus on sexual dysfunction. J Womens Health (Larchmt). 2014;23(9):765-70. https://doi.org/10.1089/jwh.2014.4805
3. Krapf JM, Mitchell L, Holton MA, Goldstein AT. Vulvar Lichen Sclerosus: Current Perspectives. Int J Womens Health. 2020;12:11-20. https://doi.org/10.2147/IJWH.S191200
4. Lee A, Bradford J, Fischer G. Long-term Management of Adult Vulvar Lichen Sclerosus: A Prospective Cohort Study of 507 Women. JAMA Dermatol. 2015;151(10):1061-7. https://doi.org/10.1001/jamadermatol.2015.0643
5. Dzhangishieva A.K., Uvarova E.V., Batyrova Z.K. Lichen sclerosus: modern view on clinical manifestations, diagnosis and treatment methods (analytical review). Pediatric and Adolescent Reproductive Health. 2018;14(3):34-50. (In Russ.) https://doi.org/10.24411/1816-2134-2018-13003
6. Zarochentseva N.V., Dzhidzhikhia L.K. Lichen sclerosus et atrophicus: modern view on the problem. Russian bulletin of obstetrician-gynaecologist. 2018;18(6):41-50. (In Russ.) https://doi.org/10.17116/rosakush20181806141
7. Solopova A.G., Achkasov E.E., Makatsariya A.D., Moskvichyova V.S., Ivanov A.E. Psycho-emotional profile of patients with vulvar lichen sclerosus. Obstetrics, Gynecology and Reproduction. 2020;14(2):203-210. (In Russ.) https://doi.org/10.17749/2313-7347/ob.gyn.rep.2020.106
8. Iannaccone AM, Verrusio G, Iurassich S. Female lichen sclerosus genitalis: discomfort and adaptation. Clin Ter. 2016;167(4):113-20. https://doi.org/10.7417/CT.2016.1940
9. Nair PA. Vulvar Lichen Sclerosus et Atrophicus. J Midlife Health. 2017;8(2):55-62. https://doi.org/10.4103/jmh.JMH_13_17
10. Sharapova L.E., Shuldyakov A.A., Lyapina E.P., Filippov A.G. Life quality parameters in patients with chronic degenerative disease of the vulva, the improvement of treatment. Fundamental research. 2011;9-3:570-574. (in Russ.) eLIBRARY ID: 16754716
11. Kolitz E, Gammon L, Mauskar M. Vulvar lichen sclerosus in women of reproductive age. Proc (Bayl Univ Med Cent). 2021;34(3):349-351. https://doi.org/10.1080/08998280.2021.1885093
12. Rees S. Living with vulval lichen sclerosus: Unheard stories and silenced voices. Case Rep Womens Health. 2020;29:e00271. https://doi.org/10.1016/j.crwh.2020.e00271
13. Brauer M, van Lunsen R, Burger M, Laan E. Motives for Vulvar Surgery of Women with Lichen Sclerosus. J Sex Med. 2015;12(12):2462-73. https://doi.org/10.1111/jsm.13052
14. Burrows LJ, Creasey A, Goldstein AT. The treatment of vulvar lichen sclerosus and female sexual dysfunction. J Sex Med. 2011;8(1):219-22. https://doi.org/10.1111/j.1743-6109.2010.02077.x
15. Lansdorp CA, van den Hondel KE, Korfage IJ, van Gestel MJ, van der Meijden WI. Quality of life in Dutch women with lichen sclerosus. Br J Dermatol. 2013;168(4):787-93. https://doi.org/10.1111/bjd.12137
16. Pinelli S, D’Erme AM, Lotti T. Management of sexual dysfunction due to vulvar lichen sclerosus in postmenopausal women. Dermatol Ther. 2013;26(1):79-82. https://doi.org/10.1111/j.1529-8019.2012.01536.x
17. van Cranenburgh OD, Nijland SBW, Lindeboom R, de Korte J, de Rie MA, et al. Patients with lichen sclerosus experience moderate satisfaction with treatment and impairment of quality of life: results of a cross-sectional study. Br J Dermatol. 2017;176(6):1508-1515. https://doi.org/10.1111/bjd.15125
18. Murphy R. Lichen sclerosus. Dermatol Clin. 2010;28(4):707-15. https://doi.org/10.1016/j.det.2010.07.006
19. Pérez-López FR, Vieira-Baptista P. Lichen sclerosus in women: a review. Climacteric. 2017;20(4):339-347. https://doi.org/10.1080/13697137.2017.1343295
20. Borghi A, Corazza M. Novel Therapeutic Approaches and Targets for Treatment of Vulvar Lichen Sclerosus. Curr Pharm Biotechnol. 2021;22(1):99-114. https://doi.org/10.2174/1389201021666200516154310
21. Criscuolo AA, Schipani C, Cannizzaro MV, Messinese S, Chimenti S, et al. New therapeutic approaches in the treatment of anogenital lichen sclerosus: does photodynamic therapy represent a novel option? G Ital Dermatol Venereol. 2017;152(2):117-121. https://doi.org/10.23736/S0392-0488.16.05272-X
22. King M, Rubin R, Goldstein AT. Current uses of surgery in the treatment of genital pain. Current Sexual Health Rep. 2014;6(4):252-258. https://doi.org/10.1007/s11930-014-0032-8
23. Lewis FM, Tatnall FM, Velangi SS, Bunker CB, Kumar A, et al. British Association of Dermatologists guidelines for the management of lichen sclerosus, 2018. Br J Dermatol. 2018;178(4):839-853. https://doi.org/10.1111/bjd.16241. PMID: 29313888.
24. Maździarz A, Osuch B, Kowalska M, Nalewczyńska A, Śpiewankiewicz B. Photodynamic therapy in the treatment of vulvar lichen sclerosus. Photodiagnosis Photodyn Ther. 2017;19:135-139. https://doi.org/10.1016/j.pdpdt.2017.05.011
25. Osiecka BJ, Jurczyszyn K, Nockowski P, Murawski M, Ziółkowski P. Photodynamic therapy with green light for the treatment of vulvar lichen sclerosus - Preliminary results. Photodiagnosis Photodyn Ther. 2017;17:185-187. https://doi.org/10.1016/j.pdpdt.2016.11.015
26. Ozog DM, Rkein AM, Fabi SG, Gold MH, Goldman MP, et al. Photodynamic Therapy: A Clinical Consensus Guide. Dermatol Surg. 2016;42(7):804-27. Erratum in: Dermatol Surg. 2017;43(2):319. PMID: 27336945. https://doi.org/10.1097/DSS.0000000000000800
27. Tasker F, Kirby L, Grindlay DJC, Lewis F, Simpson RC. Laser therapy for genital lichen sclerosus: A systematic review of the current evidence base. Skin Health Dis. 2021;1(3):e52. https://doi.org/10.1002/ski2.52
28. Prodromidou A, Chatziioannou E, Daskalakis G, Stergios K, Pergialiotis V. Photodynamic Therapy for Vulvar Lichen Sclerosus-A Systematic Review. J Low Genit Tract Dis. 2018;22(1):58-65. https://doi.org/10.1097/LGT.0000000000000362
29. Pai VV, Shukla P, Kikkeri NN. Antioxidants in dermatology. Indian Dermatol Online J. 2014;5(2):210-4. https://doi.org/10.4103/2229-5178.131127
30. Smulevich A.B. Depressii v obshhej medicine. Moscow: MIA; 2007. (in Russ.)
About the Authors
E. A. KiselevaRussian Federation
Ekaterina A. Kiseleva, Assistant of the Department of Obstetrics and Gynecology
Tomsk
Competing Interests:
Authors declare no conflict of interest.
A. Sh. Makhmutkhodzhaev
Russian Federation
Alisher Sh. Makhmutkhodzhaev, Dr. Sci. (Med.), Professor of the Department of Obstetrics and Gynecology
Tomsk
Competing Interests:
Authors declare no conflict of interest.
G. A. Mikheenko
Russian Federation
Galina A. Mikheenko, Dr. Sci. (Med.), Professor of the Department of Obstetrics and Gynecology
Tomsk
Competing Interests:
Authors declare no conflict of interest.
Review
For citations:
Kiseleva E.A., Makhmutkhodzhaev A.Sh., Mikheenko G.A. Effect of combined antioxidant and photodynamic therapy on the emotional state of patients with vulvar craurosis. Medical Herald of the South of Russia. 2023;14(1):5-12. (In Russ.) https://doi.org/10.21886/2219-8075-2023-14-1-5-12







































