Scroll to:
Risk factors for the development of discoordinated general activities as one of the variety of anomalies of uterus contractility during labor
https://doi.org/10.21886/2219-8075-2023-14-2-18-25
Abstract
Objective: to identify risk factors for the occurrence of discoordinated labor activity (DRD) and to conduct a comparative analysis of them in first- and repeat-bearing women.
Materials and methods: the analysis of the course of pregnancy and the outcome of childbirth in 175 women with DRD was carried out. The cases of DRD over five years have been analyzed. All women underwent general clinical studies, ultrasound diagnostics (ultrasound), dopplerometry (DPM), cardiotocography (CTG).
Results: functional disorders of the autonomic nervous system, morphological changes in the cervix, transferred FGM, as well as a combination of these types of pathology can be predictors of the development of DDD. There were no significant differences in the number of pregnant women suffering from NCD, having FGM, who suffered complications during pregnancy, as well as in the number of patients with prenatal and early discharge of amniotic fluid in the two groups. There are significant differences in the number of women with morphological changes in the cervix, they are significantly more in the second group. In women of the second group, significantly more often than in the first, delivery was performed by caesarean section.
Conclusions: to reduce DRD in childbirth, in the process of pre-pregnancy preparation, it is necessary to identify risk groups, which will include pregnancy-planning patients with VSD, morphological changes in the cervix, VZHPO. These women should be recommended correction of the existing genital pathology. At the onset of pregnancy, patients with VSD should be recommended to undergo psychoprophylactic preparation for childbirth. These measures, in our opinion, will help to reduce the percentage of DRD, and reduce the overall percentage of delivery by caesarean section.
For citations:
Borshcheva A.A., Pertseva G.M., Alekseeva N.A. Risk factors for the development of discoordinated general activities as one of the variety of anomalies of uterus contractility during labor. Medical Herald of the South of Russia. 2023;14(2):18-25. (In Russ.) https://doi.org/10.21886/2219-8075-2023-14-2-18-25
Introduction
Childbirth is a complex, physiological, and multi-link process that begins and completes as a result of the interconnection of many body systems. It is believed that the development of labor activity requires the formation of the labor dominant, where the leading role belongs to the central nervous system.
There is no doubt that for a favorable childbirth course, adequate contractility of the uterus is necessary. However, in the structure of possible complications in childbirth, anomalies of labor activity take one of the leading places (from 40 to 50%) [1–4]. There are different variants of labor anomalies [1][2] including weak, ineffective, excessive, and discoordinated contractions. In the authors’ opinion, such an anomaly of uterine contractility as discoordinated labor activity (DLA) is of particular interest. In recent years, a number of authors noted an increase in the tendency of this pathology during childbirth [3][5][6][7].
Many negative factors lead to the development of pathological labor activity. DLA is characterized by an inadequate increase in the basalis tone of the uterus that results in alterations in the rhythm, frequency, and amplitude of each contraction. A number of authors consider [2][4][6][7] that one of the reasons for the development of DLA is the alteration of the functional balance between the uterus tone and the activity of the sympathetic and parasympathetic nervous systems, which creates the preconditions for the emergence of several foci of excitation in the uterus. In this case, the synchronization of individual sections of the uterus gets frustrated. There are diverse factors that can provoke DLA [8-11]. They include a burdened history, namely infertility, unfavorable course of previous deliveries, and inflammatory processes in the female genital organs. In addition, the uterus contractility is affected by various malformations of the uterus itself including a saddle uterus, a bicornuate uterus, as well as its innervation disturbance. Furthermore, any dysfunction of the fetoplacental system, as well as gestosis, untimely discharge of amniotic fluid, incorrect position of the fetus, and narrow pelvis can provoke the discoordination of labor forces [10][11]. Some authors [4][5][8] claim that an extragenital pathology, namely autonomic disorders, also takes a certain place in the development of uterine contraction disturbances.
According to the clinical course, three degrees of severity of DLA are distinguished [12]. The first severity degree of DLA, namely cervical dystonia, is characterized by the predominance in contraction of the upper sections of the uterus over the lower segment. In this case, the opening of the cervix is slow, and the cervix thickens during contractions. In the second severity degree of DLA, namely segmental dystonia of the cervix, the neurogenic and myogenic regulation of uterine contraction is disturbed; spasm predominates not only in the region of the internal os but also in the overlying sections of the uterus. The third severity degree of DLA, that is complete dystocia of the uterus, is characterized by a total spasm in the cervix, a lower segment, and tubal angles; each segment of the uterus contracts in its own rhythm, and as a result, the labor slows down and stops.
A distinctive symptom complex of DLA is sharp pains both in the lower abdomen and in the lumbar region. Particular areas of the uterus contract asynchronously and asymmetrically; labor activity slows down, and the advancement of the presenting part of the fetus does not occur. The data of the vaginal examination indicate that the cervix is dense, rigid, and thickens during the contraction; its opening does not increase. Clarifying the nature of disturbances in uterine contractility is carried out with external hysterography and internal tocography [3][4]. The method of external multichannel hysterography reveals hypertonicity of the lower segment of the uterus, irregular contractions, and a decrease in their amplitude. Internal tocography gives an accurate assessment of the duration and frequency of each contraction.
DLA aggravates the course of the normal labor process [11], wherein blood circulation in the functional system “mother – placenta – fetus” gets altered and results in serious consequences for both the mother and the fetus. Discoordinated contractions can cause birth trauma including cervical ruptures, premature detachment of a normally located placenta, and uterine ruptures. Furthermore, complications are supplemented with the increase in birth act duration and the possibility of bleeding in the afterbirth and early postpartum periods.
It is assumed [2][4] that children born with DLA belong to the risk group. In particular, fetal hypoxia and antenatal fetal death are often encountered; in addition, children can be born with signs of birth trauma. Moreover, in the structure of the reasons for operative delivery, DLA is not the last one. Taking into account that DLA is a starting point for the development of some complications related to childbirth, there is a demand to have effective treatment methods for this pathology with the drug therapy arsenal. Many various profile scientists of the past have been involved and are involved currently in solving this problem. Various medications have been used to correct DLA. At the present stage, one of the main methods of treating this pathology is epidural analgesia and internal tocolysis with β-agonists. However, they do not always lead to the desired result. It is worth noting that currently there are no clear parameters for identifying the risk group of pregnant women upon DLA development, and there are no specific standards for its prevention. That prompts obstetricians to search for causes, the identification of which will help prevent this pathology [13]. With this consideration in mind, it gets clear why DLA still remains the focus of attention of obstetricians, neonatologists, and anesthesiologists.
The purpose of the study is to identify risk factors for the emergence of DLA and conduct their comparative analysis in primiparous and multiparous women.
Materials and methods
The course of pregnancy, delivery, and fetal outcomes were studied in 175 women with DLA based on the data of birth histories and exchange cards. The study was conducted in one of the maternity units in Rostov-on-Don. The criteria for selecting women for analysis were desired pregnancy, upcoming first and second births, spontaneous onset of labor, and singleton pregnancy with a biomechanism in the anterior position of vertex occipital.
A detailed medical history was collected from all women, and general clinical and special obstetric examinations were performed including bimanual examination, examination of the cervix in mirrors in order to identify anatomical features, visible pathological changes, cicatricial deformities, and discharge characteristics. Ultrasound diagnostics were performed for the female genital organs, including ultrasound of the cervix to determine its size, shape, length, condition of the internal os, location relative to the axis of the uterus; signs of cervical erosion; the presence of a polyp and cyst in the cervix; scars and cervical ruptures not sutured in previous births producing its deformity. In addition, dopplerometry, external cardiotocography (CTG), and the biophysical profile of the fetus were determined. Based on the materials of the exchange cards, the results of the examination of the cervix during pregnancy were also investigated including a bacterioscopic and bacteriological examination of the discharge from the cervical canal and the posterior fornix of the vagina to bring to light an infectious process, as well as a cytological study that can reveal the morphological features of cells characterizing a specific pathological process in the cervix.
To clarify the nature of the pathological process, some women were subjected to a colposcopic examination. Based on the above history data and examination results, women with morphological changes in the cervix were identified. Age, gestational age, anamnesis, extragenital pathology, and pathology during pregnancy in the examined groups were comparable. The diagnosis of DLA was made on the basis of the patient's complaints, the severity of vegetative disorders, the parameters of the cervix state, and the data of the instrumental research method CTG. CTG was performed in a continuous mode in the case of suspected DLA. All the above parameters were not analyzed in women with severe obstetric and extragenital pathology, multifetal pregnancy, and uterine scar after any surgical interventions, as well as in patients with uterine myoma, cervical dysplasia, and the suspected neoplastic process. Examination of all pregnant women was carried out in accordance with the Order of the Ministry of Health of the Russian Federation dated November 1, 2012 No. 572 n “Procedure for the provision of medical care in the field of obstetrics and gynecology (with the exception of using assisted reproductive technologies)”, as well as in accordance with the Order of the Ministry of Health of the Russian Federation dated October 20, 2020 No 1130 n “On approval of the Procedure for the provision of medical care in the field of obstetrics and gynecology”.
Ultrasound and Doppler examinations of the pelvic organs with the determination of the fetus mass and size; the placenta location and its structure; the amniotic fluid index; the speed and characteristics of blood flow in the placenta and umbilical cord; and other standard parameters were performed using the APLIO MX ultrasound diagnostic system manufactured by TOSHIBA MEDICAL SISTEM, Japan, 2015, with transvaginal and abdominal transducers, under a frequency of 5 and 6.5 MHz in gray scale modes. The CTG examination was carried out using medical fetal monitors for the mother and fetus G6B Plus (2017). The analysis of all the above parameters was carried out according to the data of birth histories for 2017–2021. The documentation under study contained informed consent signed by the woman for processing personal data.
Statistical processing of the obtained results was carried out using the software Statistica 10 and Microsoft Excel 2013. The rate of occurrence of signs was calculated as %. The statistical significance of differences in the rate of sign occurrence was assessed by Pearson's chi-square test. Differences between groups were considered significant at a significance level of p<0.05.
To conduct a comparative analysis of the emergence of DLA in primiparous and multiparous women, two clinical groups were composed. The first clinical group included 86 primiparous women; the second group included 89 multiparous women.
Results
Over the investigation period, 21,996 women gave birth, of which 401 (1.82%) had anomalies in labor during childbirth. Out of 401 parturient women with labor anomalies, 175 (43.64%) were diagnosed with DLA. Of the 175 women with DLA, 86 (49.14%) were primiparous (the first clinical group), and 89 (50.86%) were multiparous (the second clinical group). It was found that 52 (60.47%) women in the first group had neurocirculatory dystonia (NCD) before their pregnancy; 6 (6.98%) had morphological changes in the cervix as a consequence of the cervical erosion treatment; 8 (9.30%) women had a history of inflammatory diseases of the female genital organs (IDFGO) including endometritis, salpingitis, and bartholinitis; 20 (23.24%) women did not note the genital or extragenital pathology (Fig. 1).
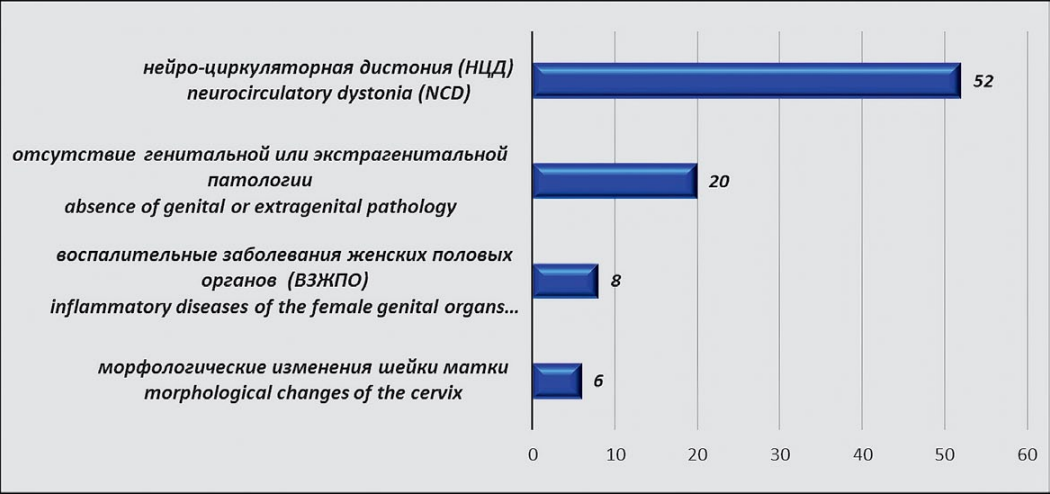
Figure 1. Anamnesis data in women of the first group
In 37 (43.02%) patients of this clinical group, pregnancy proceeded without complications, while 49 (56.98%) patients encountered complications including the abortion threat in the first and second trimesters, fetoplacental insufficiency (FPI), and mild anemia. Pre-delivery and premature discharge of amniotic fluid among primiparas was revealed in 17 (19.77%) women (Fig. 2).
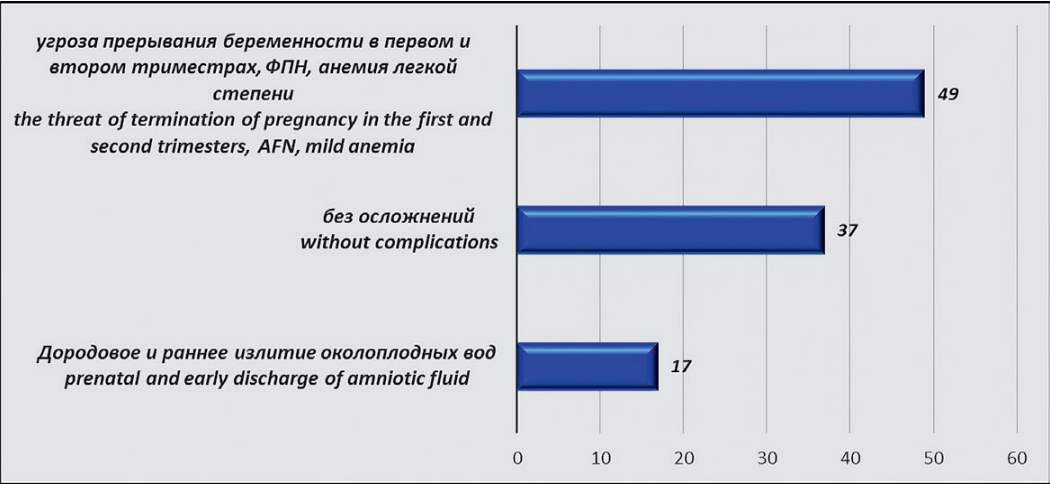
Figure 2. Features of the course of pregnancy in women of the first group
It is worth noting that the majority (78 (90.70%)) of women during pregnancy worried about the childbirth outcome and complained of anxiety, poor sleep, increased irritability, recurrent headaches (not associated with rises in blood pressure), and rapid fatigue. All women in the first group underwent epidural analgesia (EA) after the detection of DLA for the purpose of its correction. Normalization of labor activity against the background of EA occurred in 62 (72.10%) of parturient women, and their childbirths were completed through the natural birth canal. The total duration of labor in this group of women ranged from 12 to 16 hours. In 24 (27.90%) patients, against the background of EA, the normalization of labor activity did not occur, they were delivered by a cesarean section in the first stage of labor. It should be noted that among 24 patients in whom childbirth was completed by a cesarean section, all women had morphological changes in the cervix and inflammatory processes in the genital organs in history. In the period of 37–40 weeks, 72 (83.72%) women were delivered, and 14 (16.28%) were delivered in the 41st week. All children were born with Apgar scores of 7–7 and 7–8. No complications were revealed in the neonatal period course in children for the time of their staying in the maternity hospital. The postpartum period in women also proceeded without complications associated with delivery; however, 37 (43.02%) women had increased anxiety and uneasiness about caring for the child and the course of the lactation period, etc. Additional conversations were held with these women in the maternity hospital, and in order to correct their condition after discharge from the hospital, they were recommended to consult with a neurologist and a psychologist. The anamnesis of 89 multiparous patients (the second clinical group) showed that 63 (70.79%) women in this group had neurocirculatory dystonia before the pregnancy, 32 (35.96%) had morphological changes in the cervix as a consequence of pathology of the cervix and ruptures of the cervix in previous births, and 16 (17.98%) had a history of inflammatory diseases of the female genital organs including endometritis, salpingitis, and bartholinitis) (Fig. 3).
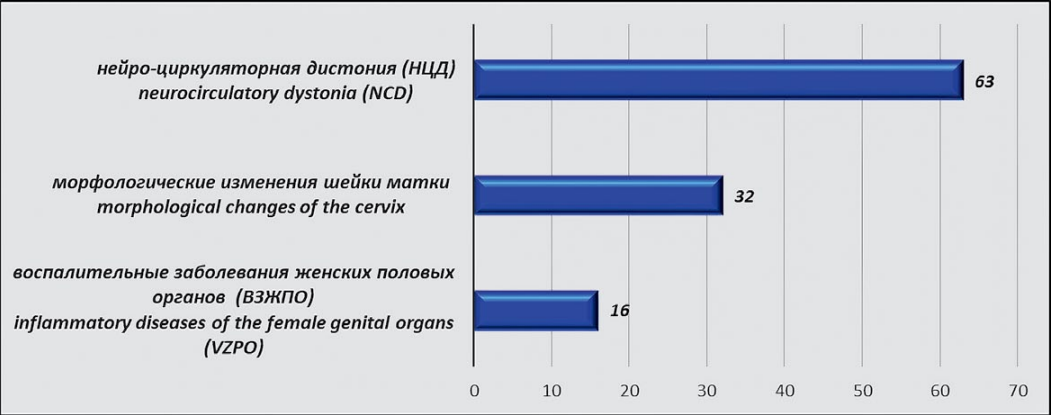
Figure 3. Anamnesis data in women of the second group
In 29 (32.58%) patients of the second clinical group, the pregnancy proceeded without complications, while the remaining 60 (67.42%) manifested complications including the abortion threat in the first and second trimesters, toxicosis of the first half of pregnancy (vomiting) of mild degree, chronic FPI, and mild anemia. Prenatal and premature discharge of amniotic fluid were revealed in 12 (13.49%) women (Fig. 4).
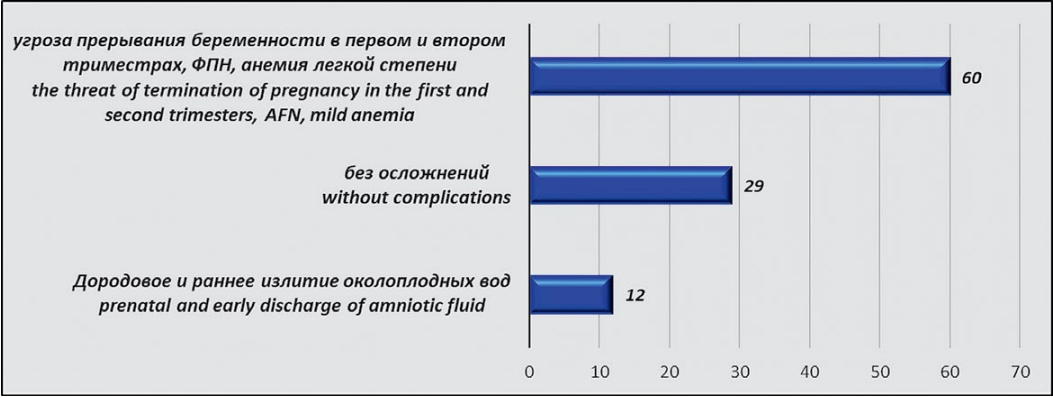
Figure 4. Features of the course of pregnancy in women of the second group
All patients in this group underwent EA during childbirth for the treatment of DLA. A good effect was observed in 24 (26.97%) women, their childbirth was completed through the natural birth canal. The total duration of labor in the second group of women was from 7 to 9 hours. In the remaining 65 (73.03%), the proper effect was not obtained, and for completing the delivery, they underwent a cesarean section. In 71 (79.78%) women, childbirth occurred at the term of 37–40 weeks, and in 18 (20.22%) women at 41 weeks. All children were born with an Apgar score of 7–7, 7–8 points. The postpartum period in both women and their newborns, similar to the first group, proceeded without complications. It should be noted that none of the women of both the first and second clinical groups underwent labor induction. All women went into labor spontaneously. All women and their children in both groups (1 and 2) were discharged from the hospital on time under the supervision of doctors from children's and women's clinics.
Discussion
Comparative data of the anamnesis investigation, the course of pregnancy, and the outcome of childbirth are presented in Table 1.
Table 1
Comparative results of anamnesis, the course of pregnancy and childbirth in women of the first and second clinical groups
|
|
Primiparous women (the first clinical group) |
Multiparous women (the second clinical group)
|
Significance level for comparison groups |
The statistical difference |
|
Number of women in groups |
86 (49.14%) |
89 (50.86%) |
p= .9571 |
Insignificant |
|
NCD in the anamnesis |
52 (60.47%) |
63 (70.79%) |
p= .4668 |
Insignificant |
|
IDFGO |
8 (9.30%) |
16 (17.98%) |
p= .3798 |
Insignificant |
|
Morphological changes in the cervix |
6 (6.98%) |
32 (35.96%) |
p= .0034 |
Significant |
|
Complications of pregnancy |
49 (56.98%) |
60 (67.42%) |
p= .4619 |
Insignificant |
|
Prenatal and early discharge of amniotic fluid |
17 (19.77%) |
12 (13.49%) |
p= .5064 |
Insignificant |
|
The number of births through the natural birth canal |
62 (72.10%) |
24 (27.90%) |
p= .0049 |
Significant |
|
Delivery by cesarean section |
24 (26.97%) |
65 (73.03%) |
p= .0034 |
Significant |
After assessing the data obtained during the investigation, one can finalize the following results. Between the two clinical groups, no significant differences were detected in the number of pregnant women suffering from cardiopsychoneurosis or IDFGO, experiencing complications over pregnancy including abortion threat in the first and second trimesters; mild toxicosis of the first half of pregnancy (vomiting); chronic FPI, and mild anemia, as well as in the number of patients with the prenatal and premature discharge of amniotic fluid. Significant differences were revealed only in the number of women with morphological changes in the cervix; their number was significantly higher in the second clinical group, that is, in multiparous women. This can be explained by traumatization of the cervix in previous births in multiparous women, followed by the formation of cicatricial deformity of the cervix (CDC). CDC could also be formed as a result of leaving unsutured or an improper technique for suturing cervical ruptures during childbirth, divergence of sutures on the cervix, operative delivery, and other reasons. The patients of this group also had abortions, IDFGO, diagnostic curettage, and other manipulations, which also impacted the CDC formation. These morphological changes in the structure of the cervix in women of the second group, apparently, were the dominant factors in the development of DLA, which led to the completion of labor by a cesarean section. In women of the second clinical group (multiparous), delivery by a cesarean section was performed significantly more often than in the first clinical group.
Conclusion
From the above, it follows that risk factors for the development of DLA during childbirth can arise from functional disorders of the autonomic nervous system, morphological changes in the cervix, past inflammatory processes of the female genital organs, as well as a combination of all these types of pathology. Notably, using EA in childbirth, normalization of labor activity and completion of childbirth through the natural birth canal can be achieved in women with an impaired autonomic nervous system and a favorable obstetric and gynecological history.
In cases with the development of DLA in patients with pathology of the genital organs and impaired autonomic nervous activity, it is expedient to raise the question of completing the birth by a cesarean section straightaway. It is attested by the fact that in parturients with a combination of morphological changes in the cervix or chronic inflammatory processes in the genital organs with disorders of the autonomic nervous system, an attempt to correct labor activity with EA does not lead to its normalization.
To reduce the emergence of DLA during childbirth, it is imperative to identify risk groups during the pregravid preparation process, which will include patients planning pregnancy when they have inflammatory diseases of the pelvic organs, erosion, ectropion, scars, and cicatricial deformity of the cervix. These women should be recommended a possible correction of the existing genital pathology and disorders of the autonomic nervous system.
In cases of pathological processes of the cervix, for their correction (before the onset of pregnancy), effective and simultaneously gentle methods of treatment should be used in order to restore the anatomical and functional healthfulness of the cervix. At this rate, radio wave resection, cryo- or laser destruction under surgical interventions on the cervix erosion and dysplasia of the cervix give better results for future pregnancy.
In the case of severe cicatricial deformity of the cervix resulting from its ruptures in previous births, women should be recommended surgical correction (plastics) of the shape and position of the cervix and the uterus body through transvaginal or abdominal routes. In the future, such treatment will allow this group of women to fully use their reproductive system and, in some cases, may prevent the development of DLA and complete the pregnancy through the natural birth canal.
At the onset of pregnancy, patients with vegetovascular dystonia should be advised to undergo psychoprophylactic preparation for childbirth at an antenatal clinic, since the lack of awareness among the pregnant about the birth act and changes in the body after childbirth prevents them from adequately perceiving the birth process and creates favorable grounds for its disturbances.
The implementation of the above recommendations, in the authors’ opinion, can help reduce the percentage of this serious pathology, namely DLA, and thereby reduce the overall percentage of deliveries by a cesarean section.
References
1. Kozonov G. R., Kuzminykh T. U., Tolibova G. H. Clinikal couses ot chictirth and pathyomor0phological fea 5 tures ofr the myornetrium in discoorrdinated labor activity. Journal of Obetetrics and Wormens Diseases. 2015; 64; 4: 39-48. (In Russ). doi: 10.17816/JOwD64439-48
2. Bologov M. A., Penjhoyan G. A. Effect of stress on development of abnormalities of labor. Kuban scientific medical bulletin. 2018; 25 (1): 46-53. (In Russ). doi: 10.25207/1608-6228-2018-25-1-46-53
3. Bologov M. A., Penihoyan G. A. Stability Estmation of the pregnant woman to stress factors inpredicting the course of labor. Modern problemis of science and education. 2015; 6: 169. (In Russ).
4. Zlobina A. V., Karahalis L. Y., Penyhoyan G. A., Lebedenko E. S., Mezugok S. H. The anomalies of the birth activity by hypotonic and hypertensive types: the causes of their origin and their effect on the fetus. Kuban scientific medical bulletin. 2011; (5): 54 -58. (In Russ). eLIBRARY ID: 17317824
5. Zlobina A. B., Karahalis L. Y., Khachak S. N. Prediction (prognostication) of the delivery'' incoordination. Sistemnyi analizi upraviente biomjedickisi sistemaqkti. 2013; 12 (3): 42-53. (In Russ). eLIBRARY ID: 20261614
6. Savitskaya E. V., Goncharova O. Yu. Anomalies of labor activity. Enigma. 2019. (In Russ).
7. Pavlov R. V. Anomalies of labor activity. Astrakhan; 2020. (In Russ).
8. Clinical protocol for the diagnosis and treatment of labor anomalies. Ministry of Health of the Russian Federation. Letter; 2017. (In Russ).
9. Kozonov G. R. Discoordination of labor activity: theory and practice. The Scientific Notes of the Pavlov University. 2014; 21 (1): 79-81. (In Russ.) doi: 10.24884/1607-4181-2014-21-1-79-81
10. Kabisova E. N., Khadaeva D. N. Prevention of labor anomalies (literature review). A young scientist. 2021; 33 (375): 98-100. (In Russ.) eLIBRARY ID: 46445878
11. Petrich L. N., Novikova O. N. Risk factors of abnormal uterine activity. Fundamental and Clinical Medicine. 2021; 6 (2): 59-65. (In Russ.) doi: 10.23946/2500-0764-2021-6-2-59-65
12. Streltsova V. L. Dystocia of labor based on the theory of adaptive reactions. Pacific Medical Journal. 2012; 4: 51-54. (In Russ.). eLIBRARY ID: 22743356
13. Mudrov V. A. Possibilities of forecasting anomalies of labor activity. Journal of Obstetrics and women's diseases. 2020; 5 (69): 13-26. (In Russ.). doi: 10.17816/JOwD69513-26
About the Authors
A. A. BorshchevaRussian Federation
Alla A. Borshcheva, P. h. D, associate Professor, associate Professor of the Department
Department of obstetrics and gynecology No. 1
Rostov-on-Don
G. M. Pertseva
Russian Federation
Galina M. Pertseva, P. h. D., assistant
Department of obstetrics and gynecology No. 1
Rostov-on-Don
N. A. Alekseeva
Russian Federation
Natalia A. Alekseeva, P. h. D, associate Professor, associate Professor of the Department
Department of Health Organization and Public Health No. 2
Rostov-on-Don
Review
For citations:
Borshcheva A.A., Pertseva G.M., Alekseeva N.A. Risk factors for the development of discoordinated general activities as one of the variety of anomalies of uterus contractility during labor. Medical Herald of the South of Russia. 2023;14(2):18-25. (In Russ.) https://doi.org/10.21886/2219-8075-2023-14-2-18-25







































