Scroll to:
Evaluation of treatment results in patients after surgical hemostasis using CT-angiography
https://doi.org/10.21886/2219-8075-2022-13-4-66-72
Abstract
Objective: to evaluate the results of treatment of patients after undergoing surgical hemostasis in obstetric hypotonic bleeding. Materials and methods: the 31 patients were examined, whose delivery was complicated by hypotonic uterine bleeding, and as a result, surgical hemostasis was performed in the amount of ligation of the ovarian and internal iliac artery. Anthropometric data were analyzed, as well as the dynamics of the results of laboratory and instrumental research methods before and after surgery. In the late postoperative period, the results of helical computed tomography (CT) under angiography conditions were evaluated in the period from 6 months to 5 years. Statistical processing was carried out using the IBM SPSS Statistics 25 program. Results: the age, anamnestic data, anatomical and physiological parameters of patients, terms of delivery and their outcome did not become predictors of developed hypotonic bleeding. Early postpartum bleeding was determined in 93,5% of cases. Extirpation of the uterus was performed in 9,7% of cases. The median blood loss was 1200,0 ml, blood loss of 45-50% of the BCC was determined in 19,4%, 35–45% of the BCC was also in 19,4%. The reduced level of erythrocytes persisted until the moment of discharge, and the reduced hemoglobin after the operation tended to increase. In the course of CT, in 100% of cases, defects in the contrasting of the internal iliac artery on both sides were determined. Collateral circulation was also developed in 100,0% of cases, despite the type of defect in the internal iliac artery. Conclusions: ligation of the ovarian and internal iliac artery is a reliable method of surgical hemostasis, which allows saving the uterus in 90,3% of cases. In the late postoperative period, all patients developed various degrees of arterial patency in the ligation zone, and collateral circulation developed on both sides.
Keywords
For citations:
Kantsurova M.R., Rymashevsky A.N., Sapronova N.G., Babaev M.V., Sapronov R.S. Evaluation of treatment results in patients after surgical hemostasis using CT-angiography. Medical Herald of the South of Russia. 2022;13(4):66-72. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-4-66-72
Introduction
Obstetric hypotonic bleeding is a frequent and severe complication that occurs during labor and in the postpartum period (50% of all obstetric bleeding) [1–2]. The outcome of this condition can threaten a woman's life and deprive her of her childbearing function after a hysterectomy. The existing methods for stopping bleeding are well known and described in detail in national guidelines and clinical recommendations [3]. However, the optimization of surgical hemostasis tactics continues to be a challenge of primary importance.
Internal iliac arteries ligation (IIAL) is one of the labor-intensive but effective methods of surgical hemostasis. This procedure was first introduced in 1984, but is not widely used in gynecological practice. On the contrary, in obstetrics, this surgical intervention was widely implemented. In 1902, Kronig performed OA and IIA ligation in one patient for uterine atony and in another for high cervical rupture [4]. The bleeding stopped in both cases. In 1968, Burchell [5] found that stopping bleeding was not associated with mechanical cessation of blood flow, but with a change in its nature and direction due to the connection of the system of anastomoses, which provides blood flow to the reproductive organ. Blood supply to the uterus starts to come from a network of small arteries, and subsequently, the uterus fully restores its function. Bunin and Gorbunov (1990) [6] believed that after IIAL, blood enters its lumen through anastomoses of the iliopsoas and lateral sacral artery, wherein the blood flow becomes reversed. After ligation, the anastomoses start functioning immediately, and the blood passing through the small collateral vessels loses its arterial rheological properties and approaches the venous one in its characteristics.
During IIAL surgery, there is a possibility of the iliac vein damage, ureters injury, and an erroneous ligation of the external iliac artery (EIA). The obstetrician-gynecologist performing this procedure must have the skills and competence of a vascular surgeon or it must be performed directly by a vascular surgeon. To date, there are still heated discussions about the consequences of IIAL, as some authors believe that complete cessation of the blood flow in the vessel leads to uterine ischemia and necrosis [7].
The study aimsto evaluate the results of the treatment of patients who underwent surgical hemostasis for obstetric hypotonic bleeding.
Materials and Methods
This work is a prospective case-control study and fully meets the requirements of biomedical ethics. It was approved by the local ethical committee of the Rostov State Medical University. The study was conducted in the facilities of the maternity department of City Hospital No. 7 (Maternity House No. 5) in Rostov-on-Don in 2017–2022. A total of 31 patients were examined, who were enrolled by the inclusion-exclusion criteria and had labor complicated by uterine hypotonic bleeding and who underwent surgical hemostasis in a form of OA and IIA ligation.
The operation was performed according to the conventional technique. After ligation of the OA, the uterus was pulled out into the wound and deflected to the pubic symphysis. The intestinal loops were separated with wet tissue and the parietal peritoneum was exposed above the common iliac artery (CIA) bifurcation site. Then, the parietal peritoneum sheet was dissected in the projection of the CIA bifurcation. After that, by blunt and sharp way, the IIA was separated from the fatty tissue and fascia, and the ureters were moved aside. Using a dissector, the IIA was carefully extracted from the surrounding fatty tissue, fascia, and the underlying internal iliac vein. Then, ligature with synthetic resorbable material (polyglycolide) was placed under the artery through the gap between the IIA and the vein using the dissector. After checking the pulsation of the EIA and peristalsis of the ureter, the ligature was tied directly at the bifurcation site with four knots, and the ends of the threads were cut off. The same procedure was performed on the opposite side.
All patients underwent a comprehensive clinical and laboratory examination, which included a collection of complaints, a study of obstetric and gynecological history, a physical examination, and an evaluation of the results of laboratory and instrumental diagnostic methods before and after surgical intervention. In the postoperative period, the required clinical and laboratory examination was performed; the results were also assessed by spiral computed tomography in angiography conditions on a Brilliance CT 64 slice machine at 6 months to 5 years after the surgical intervention.
Statistical analysis was performed using IBM SPSS Statistics 25. Before the statistical analysis of the data, the authors assessed the normality of the distribution of all quantitative indicators using the Shapiro-Wilk test, taking into account the sampling size. Statistical data of indicators with a distribution other than normal was described with median (Me) and 25th and 75th percentiles. For the normal distribution, the authors used mean and standard deviation for age, the height of patients, and term of delivery. The associations were examined before-post-during discharge using Friedman's test. The data was statistically significant at p<0.05.
Results
The mean age of the patients (n=31) was 34.3±6.3 years, the height was 167.9±6.1 cm, and the mean weight was 82.1±15.5 kg. The prevalence of obesity was determined in 9 (29.0%) women taking into account the height-weight ratio analysis.
The current pregnancy was the first in 2 women (6.5%), second in 7 (22.6%), third in 7 (22.6%), fourth in 3 (9.7%), fifth in 4 (12.9%), sixth in 4 (12.9%), seventh in 1 (3.2%), eighth in 1 (3.2%), ninth in 1 (3.2%), and tenth in 1 woman (3.2%). A history of abortions was recorded in 9 women (30%), and the number of abortions of more than 2 was determined in 7 women (22.6%).
A uniformly contracted pelvis was observed in 1 woman (3.2%). Placenta previa was observed in 11 patients (35.5%), while previa with hemorrhage was detected in 9.7% of cases. Placenta increta was detected in 5 women (16.1%). Only 1 patient (3.2%) had a premature placental abruption. Hydramnios was detected in 2 women (6.5%). The presence of postoperative uterine scar was detected in 17 cases (54.8%), and uterine myoma in 9 women (29.0%). The fetus was in the wrong position: breech presentation – in 1 (3.2%) case, transverse – in 1 (3.2%) case, and shoulder – in 3 (9.7%) women. Large fetal size was detected in 1 person (3.2%).
In the vast majority of cases (87.1%), the delivery occurred at term and averaged 38.26±1.27 weeks. Natural delivery occurred in 5 women (16.1%) and 26 women (83.9%) delivered by cesarean section. The outcome of all deliveries was live birth.
Early postpartum hemorrhage was detected in 93.5% of cases (19 women). Autologous hemotransfusion using the Cell Saver machine was performed in 3 women (9.7%). Uterine extirpation, as the maximum unfavorable outcome of hypotonic bleeding despite OA and IIA ligation, was performed in 9.7% of cases (3 women).
One of the stages of the study was the assessment of the blood loss volume. The median Me was 1200.0 ml [ 895.0–2000.0]. It should be noted that a severe degree of blood loss (45–50% of the CBV) was determined in 19.4% of cases (6 women) and the 4th degree of blood loss (35–45% of the CBV) – in 19.4% (6 women).
In addition to the volume of blood loss, the authors assessed the dynamics of the CBC parameters to analyze the possible development of anemic syndrome, as well as inflammatory and hemostatic changes. The analysis of the data included the values of the CBC parameters before surgery, on the first day after surgery, and at the time of discharge from the hospital in order to assess the recovery dynamics of the parameters (Table 1).
Table 1
Indicators of CBC before-after surgery and before discharge from the hospital
|
Indicator |
Group (n=31) |
||||||
|
Before surgery |
After surgery |
Before discharge |
p |
||||
|
Me |
Q1-Q3 |
Me |
Q1-Q3 |
Me |
Q1-Q3 |
||
|
Erythrocytes, х1012/L |
3.79 |
3.52-4.25 |
3.31 |
2.8-4.02 |
3.15 |
2.86-3.95 |
<0.001* |
|
Leukocytes, х109/L |
9.7 |
8.4-13.7 |
16.2 |
12.25-20.3 |
10.6 |
9.0-16.65 |
<0.001* |
|
Platelets, х109/L |
198.0 |
168.5-246.5 |
207.0 |
159.0-251.0 |
254.0 |
193.0-306.0 |
0.003* |
|
Hemoglobin, g/L |
110.0 |
105.0-123.0 |
94.0 |
80.5-108.0 |
98.0 |
83.5-106.0 |
<0.001* |
|
ESR, mm/hr |
20.0 |
18.0-22.0 |
26.0 |
23.5-30.0 |
25.0 |
22.0-27.5 |
<0.001* |
Note: * – The significance of the differences in the associated samplings was calculated by the Friedman’s test
The authors revealed a statistically significant decrease in erythrocyte count after the surgical intervention, which persisted even at the time of patients' discharge from the hospital (evaluation was performed using the Friedman test for related groups, p<0.001). There was also a significant depression in the hemoglobin levels with a tendency for the concentration to rise by the time of discharge, and the difference was statistically significant (p<0.001). Possible development of inflammatory changes in women after surgical intervention, which was manifested as increased leukocyte levels in the second compared association, is worth noting, but further rapid recovery of the indexes to normal values was noted (p<0.001). A statistically significant increase in platelet count is associated with the activation of the hemostasis system in response to hypotonic bleeding (p=0.003). Besides, an increase in ESR was observed after the operation, which can be explained by the development of anemic syndrome (p<0.001).
At 6 months to 5 years after the operation, the patients, with the deduction of 3 women who had uterine extirpation (n=28), underwent spiral CT angiography with contrasting of the abdominal part of the aorta and iliac arteries. All women were prepared for the study; creatinine and BUN levels were checked before the procedure; breastfeeding women were advised to express milk after the procedure. The following results are presented in Table 2.
Table 2
Results of a CT-angiographic study in patients
|
Indicator |
Group |
|
|
abs. |
% |
|
|
The abdominal aorta has a normal course and branching |
28 |
100.0 |
|
Aortic bifurcation is visualized at the level of L4-L5, the configuration is typical |
28 |
100.0 |
|
The common iliac artery on the right has a normal diameter, smooth contours, is homogeneously filled with a contrast agent |
28 |
100.0 |
|
The common iliac artery on the left has a normal diameter, smooth contours, is homogeneously filled with a contrast agent |
28 |
100.0 |
|
The external iliac artery on the right has a normal diameter, smooth contours, is homogeneously filled with a contrast agent |
28 |
100.0 |
|
The external iliac artery on the left has a normal diameter, smooth contours, is homogeneously filled with a contrast agent |
28 |
100.0 |
|
The internal iliac artery on the right has a normal diameter, smooth contours, is homogeneously filled with a contrast agent |
0 |
0 |
|
The internal iliac artery on the left has a normal diameter, smooth contours, is homogeneously filled with a contrast agent. |
0 |
0 |
|
Lack of contrast enhancement of the proximal right internal iliac artery (occlusion) |
25 |
89.3 |
|
Lack of contrast enhancement of the proximal left internal iliac artery (occlusion) |
26 |
92.9 |
|
The internal iliac artery on the right is narrowed in the proximal segment (stenosis) |
3 |
10.7 |
|
The internal iliac artery on the left is narrowed in the proximal segment (stenosis) |
2 |
7.1 |
|
Pronounced collaterals on the right |
28 |
100.0 |
|
Pronounced collaterals on the left |
28 |
100.0 |
Thus, in 100% of cases (28 patients), contrast defects were revealed in IIA on both sides (occlusion and stenosis). IIA occlusion on both sides was detected in 25 patients (89.3%) with a length from 5.0 to 18.0 mm (Figure 1 (A, B)). In one patient, there were signs of left IIA occlusion, and the IIA lumen with irregular stenosis was visualized on the right side (Figure 2).
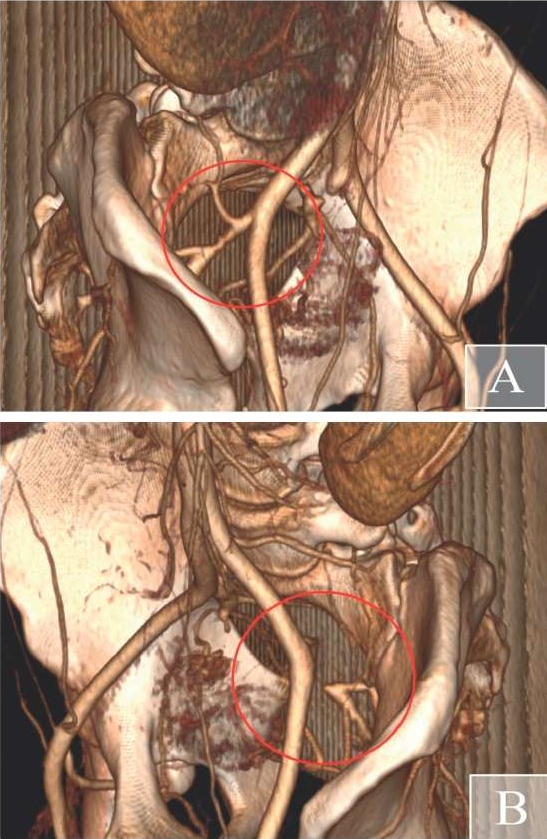
Figure 1. CT-angiogram of patient G., 39 years old. A - irregularity of the lumen of the right internal iliac artery with the presence of an intraluminal defect in its contrasting in the proximal section (stenosis). B - occlusion of the left internal iliac artery from the mouth
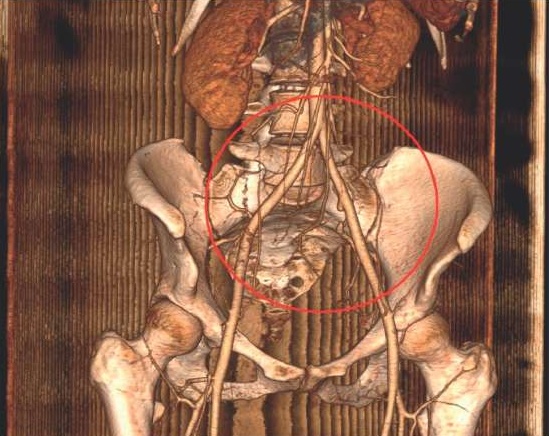
Figure 2. CT-angiogram of patient M., 31 years old. Occlusion of both iliac arteries. Pronounced collateral circulation, better developed on the left
Collateral circulation also developed in 100.0% of cases regardless of the type of IIA defect (occlusion or stenosis). Only in 2 observations (7.1%), the left and right IIA were traced along the entire length with the signs of stenosis in the ligation zone and with the development of collateral circulation as well.
Discussion
In the present study, the authors analyzed the results of the treatment of patients after uterine hypotonic bleeding, which was stopped after OA and IIA ligation.
Age, anamnestic data, anatomical and physiological parameters of the patients, terms of delivery, and their outcome were not predictors of the complication. The authors revealed that early postpartum hemorrhage occurred in 93.5% of cases. Uterine extirpation, as the maximum unfavorable outcome, was performed in 9.7% of cases.
Median blood loss was 1200.0 ml, blood loss of 45–50% of the CBV was revealed in 19.4%, 35–45% of the CBV – in 19.4%.
A decrease in the erythrocyte count after the operation was still observed at discharge (p<0.001); a significant depression of the hemoglobin level was revealed with the tendency of its increase to the time of discharge (p<0.001).
The novelty of the study was the performance of spiral CT angiography with contrast of the abdominal portion of the aorta and iliac arteries in 28 patients 6 months to 5 years after the surgery. The results revealed IIA patency abnormalities in 89.3% of both sides in the form of persistent occlusion of the proximal arteries. Only 3.6% of patients had a combination of occlusion on one side and stenosis on the other side. In 7.1%, the IIA patency disorders were stenotic on both sides. A developed collateral circulation on both sides was detected in 100.0% of observations.
Conclusions
The performed ligation of OA and IIA is a reliable method of surgical hemostasis allowing for the sparing of the reproductive organ in 90.3% of cases of hypotonic bleeding. In the follow-up period after the operation, all 100% of patients had various degrees of arterial patency disorders in the ligation zone (7.1% stenosis and 92.9% occlusion). In 100% of cases, collateral circulation on both sides developed.
The contribution of the authors is equivalent.
Conflict of interests. Authors declare no conflict of interests.
References
1. Rymashevsky A.N., Volkov A.E. Surgical hemostasis for obstetric hemorrhage: a monograph. Germany; 2015. (in Russ.)
2. Radzinsky V.E. Obstetric aggression, v.2.0. Moscow; 2017. (in Russ.)
3. Savelyeva G.M., Sukhikh G.T., Serova V.N., Radzinsky V.E., eds. Obstetrics. Moscow: GEOTAR-Media; 2019. (in Russ.)
4. Breslav I.Yu. Bleeding during late pregnancy and labor. Possibilities of organ-sparing surgery. Akusherstvo i Ginekologiya/ Obstetrics and Gynecology. 2016;(10):52-8. (in Russ.) https://doi.org/10.18565/aig.2016.10.52-8
5. Haylamazyan E.K. Gynecology: a textbook for medical schools. St. Petersburg; 2013. (In Russ.)
6. Bunin A.T., Gorbunov A.JI. Ligation of the internal iliac arteries as a stage in the surgical treatment of obstetric bleeding. Obstetrics and Gynecology. 1990;(10):67-70. (in Russ.)
7. Kantsurova M.R., Rymashevsky A.N. Surgical hemostasis for obstetric hemorrhage: experimental and clinical studies. Medical Herald of the South of Russia. 2020;11(3):20-26. (In Russ.) https://doi.org/10.21886/2219-8075-2020-11-3-20-26
About the Authors
M. R. KantsurovaRussian Federation
Maria R. Kantsurova - assistant of the Department of obstetrics and gynecology №1, Rostov State Medical University.
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest
A. N. Rymashevsky
Russian Federation
Alexander N. Rymashevsky - Dr. Sci. (Med.), Professor, head of the Department of obstetrics and gynecology №1, Rostov State Medical University.
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest
N. G. Sapronova
Russian Federation
Natalia G. Sapronova - Dr. Sci. (Med.), docent, head of the Department of surgical diseases №1, Rostov State Medical University.
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest
M. V. Babaev
Russian Federation
Michail V. Babaev - Dr. Sci. (Med.), Professor, head of Department of radiation diagnostics and radiation therapy, Rostov State Medical University.
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest
R. S. Sapronov
Russian Federation
Ruslan S. Sapronov - obstetrician-gynecologist, city Hospital №7.
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest
Review
For citations:
Kantsurova M.R., Rymashevsky A.N., Sapronova N.G., Babaev M.V., Sapronov R.S. Evaluation of treatment results in patients after surgical hemostasis using CT-angiography. Medical Herald of the South of Russia. 2022;13(4):66-72. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-4-66-72







































