Scroll to:
The profile of comorbid conditions and the structure of mortality in patients with rheumatoid arthritis in the Stavropol Territory: preliminary results
https://doi.org/10.21886/2219-8075-2022-13-3-173-182
Abstract
Objective: to study the comorbid background and mortality structure of patients with rheumatoid arthritis (RA) in the Stavropol region in a cohort of patients of the Stavropol Regional Clinical Hospital (SRCH) within the period 2015–2021. Materials and methods: There was carried out systematic review of the literature. There was carried out the analysis of the protocols of autopsies in the pathoanatomical department of the SRCH within 2015-2021. There were studied the comorbidity component and lethal outcomes of patients with RA in the pathoanatomical diagnosis. Results: the structure of the comorbid pathology of RA patients in the SRCH cohort included coronary heart disease (CHD), autoimmune thyroiditis (AT), respiratory diseases (RD), hypertension (HT), “Blastomatosis”, diabetes mellitus (DM), COVID-19 infection. The comorbidity profile of patients with RA in decreasing order of the incidence of the pathological condition was as follows: CHD (35.29%) > RD (29.41%) > (“Blastomatosis”, СOVID-19 by 11.75%) > (AT, HT, DM by 5.88%). The structure of the conditions that led to the death of patients with RA included: acute myocardial infarction (40.0%), hemorrhagic stroke (6.67%), breast cancer (13.33%), thyroid cancer (6.67%), viral pneumonia (20.0%), sepsis (13.33%). Conclusions: the data obtained provide information that can be used by rheumatologists to optimize the strategy for managing RA and the risk of comorbid conditions.
For citations:
Shchendrigin I.N., Mazharov V.N. The profile of comorbid conditions and the structure of mortality in patients with rheumatoid arthritis in the Stavropol Territory: preliminary results. Medical Herald of the South of Russia. 2022;13(3):173-182. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-3-173-182
Introduction
Rheumatoid arthritis (RA) continues to be associated with high mortality rates. The increased mortality of patients with RA is mainly due to concomitant diseases, among which a special place is occupied by cardiovascular diseases (CVDs) [1], infections [2], kidney pathology [3], respiratory diseases [4], and oncopathology [5]. Despite significant progress in the management of RA, the burden of comorbid pathology for these patients remains a serious problem.
The last decade has brought a new understanding of comorbidity associated with RA [1]. Comorbid pathologies are considered independent predictors of increased mortality in RA [6]. Convincing evidence demonstrates that people with RA are 80% at high risk of developing one or more comorbid conditions [7][8]. These pathologies may have atypical signs, are difficult to diagnose and poorly treatable [9][10]. Comorbid conditions can affect the activity of RA, become an obstacle to optimal control of the disease, and lead to an increased risk of death of patients [11][12].
Today, there is information confirming a decrease in the frequency of deaths of patients with RA [13][14]. There is even evidence that the mortality rate in RA patients is similar to that in patients in the general population [15]. At the same time, other studies continue to show that mortality in patients with RA is significantly higher or that the mortality gap with the total population tends to increase [16]. The reasons for the differences in mortality rates can be explained by the change in the principles and tactics of treatment of patients with RA over the past decade, as well as the peculiarities of ethnicity [17][18] and the different structure of the analyzed cohorts of patients [19], which requires an assessment of the risk of mortality in patients with RA in real clinical practice.
Given the significant spread of digital data, the lack of clear national and regional registers characterizing the state of the problem of comorbidity and mortality of patients with RA, including in dynamics, a key role in this regard should be given to periodic epidemiological studies, including a description of how the disease manifests itself in a particular cohort (incidence, comorbidity, mortality, trends in time, and regional features).
The purpose of the study was to study the comorbid background and mortality structure of RA patients in the Stavropol Territory in a cohort of patients of the Stavropol Regional Clinical Hospital in the period of 2015–2021.
Materials and methods
The study included 998 patients (107 men and 891 women, average age – 54.1±1.41 years) with a reliable diagnosis of RA, established according to the classification criteria ACR/EULAR (2010) [20]. All patients were treated at the rheumatology center of the Stavropol Territory State Budgetary Healthcare Institution “Stavropol Regional Clinical Hospital” (SRCH) in the period of 2015–2021. All patients received voluntary informed consent to participate in the study according to the Helsinki Declaration of the World Medical Association (WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects, 2013) and the processing of personal data.
After the formation of the register of patients with RA, the next endpoint was evaluated — the onset of a fatal outcome from any cause. Autopsy protocols for 2015–2021 in the pathology department of the SRCH were analyzed. The fatal outcomes of patients with RA in the pathoanatomic diagnosis were studied. The results were qualitative data in the form of relative frequencies (%).
To compare the results obtained with the data of modern literature, a search and a systematic review of sources of 2018–2022 was conducted using various combinations of keywords (“rheumatoid arthritis”, “comorbid conditions”, “epidemiology”, “cohort study”). Online search of literary data was carried out in available databases, such as Elibrary, Pubmed, Scopus, and ScienceDirect.
Results
The results of the analysis of the frequency and structure of comorbid pathology of patients with RA, conducted on the basis of data from a systematic review of literature sources (2018–2022), are summarized in Table 1.
Table 1
Summary of the comorbid background of patients with rheumatoid arthritis (literature data)
|
Reference |
Year |
CVD |
Hypertonic disease |
Respiratory diseases |
Diabetes |
Diseases of the gastrointestinal tract |
Kidney disease |
Osteoporosis |
Malignancy |
Infections |
|
Kalinina E.V. et al. [21] |
2018 |
87.6% |
58.97% |
3.41% |
11.11% |
61.53% |
- |
- |
- |
1.7% |
|
Kasimova, M.B., Pulatova, S.B. [22] |
2018 |
48.8% |
- |
14.4% |
- |
25.3% |
35.1% |
- |
- |
- |
|
An J. et al. [23] |
2019 |
79.4% |
- |
35.4% |
29.0% |
- |
- |
- |
17.8% |
1.4% |
|
Batko B. et al. [24] |
2019 |
24.2% |
46.9% |
7.0% |
14.4% |
2.3% |
- |
- |
- |
- |
|
Козлова В.И., Скрынник Е.И. [25] |
2019 |
42.0% |
- |
- |
11.2% |
38.0% |
- |
- |
- |
- |
|
Raskina T. et al. [26] |
2020 |
48.5% |
36.9% |
- |
- |
79.2% |
27.6% |
20.0% |
- |
- |
|
Almutairi K. et al. [14] |
2021 |
26.6% |
- |
5.5% |
2.6% |
- |
- |
- |
16.8% |
- |
|
Figus F.A. et al. [1] |
2021 |
50% |
- |
30.0-40.0% |
- |
- |
- |
- |
- |
- |
|
Gutierrez J.C. et al. [27] |
2021 |
35.1% |
- |
- |
- |
- |
26.2% |
39.1% |
- |
45.2% |
|
Tekaya A.B. et al. [28] |
2021 |
16.8% |
31.4% |
27.1% |
19.6% |
9.2% |
- |
- |
- |
- |
|
Hannech E. et al. [29] |
2022 |
6-7% |
30.0-31.0% |
27.0-28.0% |
18.0-26.0% |
11.0% |
- |
- |
- |
- |
|
Miura T. et al. [30] |
2022 |
8.0% |
37.3% |
12.2% |
8.1% |
- |
25.2% |
- |
5.7% |
- |
|
Naimova S.A. [3] |
2022 |
- |
- |
- |
- |
- |
43.0% |
- |
- |
- |
|
Laila D. et al. |
2022 |
11.1% |
- |
5.8% |
- |
- |
- |
- |
12.9% |
- |
|
Varela D. C. et al. [31] |
2022 |
- |
27.7% |
- |
- |
- |
- |
19.3% |
5.5% |
14.3% |
|
Lala V. et al. [18] |
2022 |
7.5% |
70.0% |
|
15.3% |
60.0% |
6.3% |
58.0% |
1.5% |
20.7% |
The spectrum of comorbid conditions registered by researchers in patients with RA is quite wide and includes heart disease, hypertension, respiratory diseases, diabetes mellitus, gastrointestinal diseases, kidney pathology, osteoporosis, malignant neoplasms and infections.
The table clearly shows that the data on the occurrence of comorbid conditions in patients with RA vary in a very wide range from different sources. In the bulk of the sources, the leading position in terms of prevalence is occupied by either acute respiratory infections or respiratory pathologies. At the same time, the spread of data on the occurrence of these comorbid conditions is significant and ranges from 11.1% to 87.6% and from 3.41% to 40.0%, respectively.
The nature of comorbidity of patients diagnosed with RA in the Stavropol Territory is presented in the form of a diagram in Figure 1.
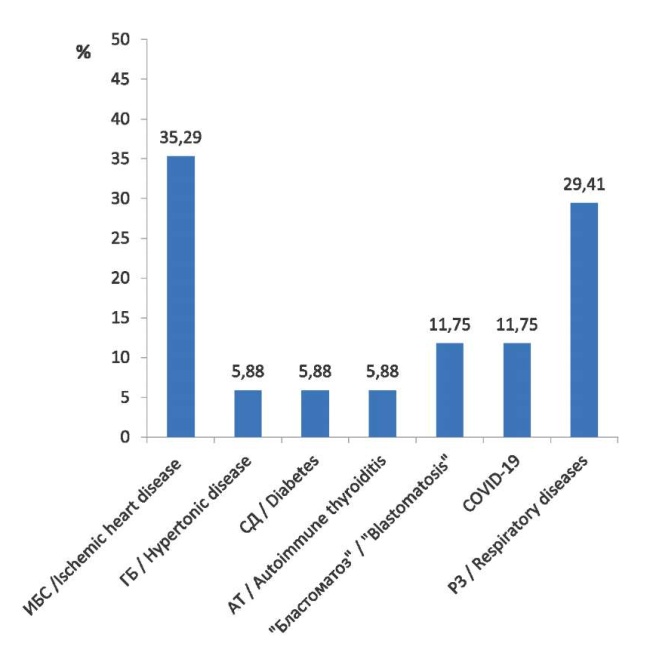
Figure 1. Profile of comorbid pathologies in SRCH patients with RA.
Note: CHD — coronary heart disease; HT — hypertension; DM — diabetes mellitus; RH — respiratory diseases.
The leading place in the structure of comorbidity of RA patients in the cohort of SRCH patients was occupied by coronary heart disease (35.29%). Respiratory diseases were registered in the second place in this sample (29.41%). The representation of “Blastomatosis” and COVID-19 in comorbidity was 11.75% of patients each. The share of pathologies such as hypertension, diabetes mellitus, and autoimmune thyroiditis accounted for 5.88% of patients.
The frequency of determining causes of deaths was calculated for the number of patients with a verified cause. The structure of the conditions of fatal patients with RA is shown in the diagram (Figure 2).
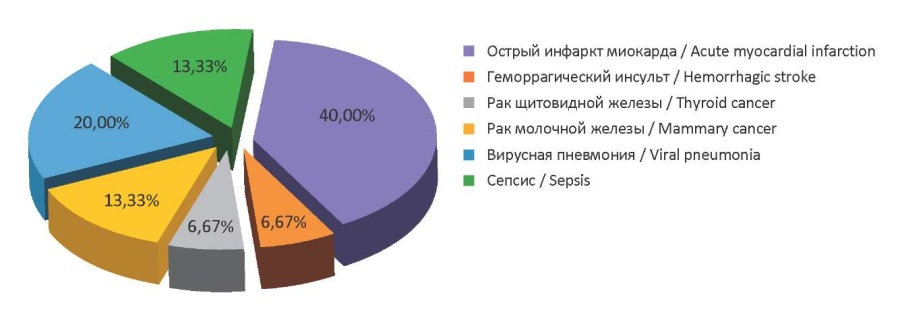
Figure 2. Diagram of a number of final clinical diagnoses of SRCH patients with RA, established post-mortem, with autopsy.
Acute myocardial infarction (40.0%) was registered as the leading cause of deterioration of the condition of patients with RA in the SRCH cohort, which led to death. The remaining documented pathologies in this aspect, in order of decreasing frequency of their occurrence, were distributed as follows: viral pneumonia (20.0%) > breast cancer (13.3%), sepsis (13.3%) > thyroid cancer (6.67%), hemorrhagic stroke (6.67%).
Discussion
RA is a severe progressive disease that leads to deterioration of the functional status of the patient, disability, and an increase in the mortality rate. The prevalence of this pathology implies the presence of concomitant pathologies in patients and, accordingly, a burdened comorbid background. Concomitant diseases may appear before the development of RA, during exacerbation or remission, and may also be a complication of chronic inflammation or its drug treatment [32]. The comorbid background is an important aspect of observation and correction in patients with RA due to its significant influence on the course of the disease and its outcome [33]. Comorbid conditions should be taken into account due to a known or suspected association with certain classes of drugs. In clinical practice, it is extremely important to balance the potential benefits of RA treatment with the possible risk of concomitant diseases [2]. Therefore, an adequate and timely assessment, identification, and correction of comorbid risk components are required.
The authors’ review of the latest scientific data indicated a high percentage of cardiovascular and respiratory pathologies, gastrointestinal diseases, metabolic disorders (diabetes mellitus, osteoporosis), oncological and infectious load in patients with RA. At the same time, there is no common uniform regular structure of the comorbid profile in RA. The occurrence and structure of comorbid conditions vary in a very wide range of indicators. There is a pronounced geographical dependence, ethnic, cohort, and age characteristics.
The structure of comorbidity of patients with RA in the Stavropol Territory in the cohort of SRCH patients included coronary heart disease (CHD), autoimmune thyroiditis (AT), respiratory diseases, hypertension (HT), “Blastomatosis”, diabetes mellitus (DM), and COVID-19 infection. The comorbidity profile of patients with RA, in order of decreasing frequency of occurrence of the pathological condition, had the following form: CHD > RH > (“Blastomatosis”, COVID-19) > (AT, HT, DM) and logically determined the structure and frequency of the onset of conditions that led to the fatal outcome of patients with RA.
The problem of studying the mortality of RA patients is a difficult task, since the registration of the causes of death of these patients often occurs without a diagnosis of RA. In practice, only a part of pathological conditions requiring therapeutic and diagnostic measures are included in the main diagnosis, the rest are registered as concomitant, and often are not included in clinical and pathoanatomic diagnoses at all. This is especially true for long-term chronic processes, which are rheumatic diseases, in particular RA [34].
Taking this into account and the availability of not always unambiguous literature data, there is an obvious need to assess the risk of mortality in patients with RA in real clinical practice.
For the Stavropol Territory, almost 50% of the conditions that led to the fatal outcome of patients with RA were cardiovascular pathologies (acute myocardial infarction – 40.0%; hemorrhagic stroke – 6.67%). These data turned out to be relatively comparable with the current assessment in this regard in other regions of Russia and countries. According to the results of large cohort studies, cardiovascular mortality in RA ranges from 15 to 50% [6][35]. The magnitude of the risks of death from CVDs varies in different studies, which may be related both to the characteristics of the studied cohorts of patients and the effectiveness of achieving or not achieving the goal of treatment, as well as to the characteristics of the therapy performed.
New CVD treatment strategies have a positive effect on reducing the mortality of patients with RA [36]. Today, a number of researchers [13][14] have revealed a reduction in the risk of death of RA patients from CVDs.
The results of this study contrast somewhat with these empirical data. The share of CVD in the structure of conditions that led to the mortality of RA patients is in the first place and is relatively high. The trend towards a decrease in the mortality of patients with RA in the Stavropol Territory of the SRCH cohort has not yet been expressed, which suggests that the development and implementation of updated guidelines on cardiovascular risk management in this aspect could be beneficial.
Other conditions that led to the death of patients with RA in the SRCH cohort were neoplasms, viral pneumonia, and sepsis.
The given results on the mortality rate of RA patients caused by oncopathology did not fall out of the range of data from cohort studies and meta-analytical reviews of the last five years [5][14][23]. At the same time, in the cohort of RA patients studied by the authors, in 6.67% of cases, death occurred due to thyroid cancer, and in 13.3% of cases, it was caused by breast cancer. This to some extent goes against a number of data [1], according to which patients with RA differ in reducing the risk of breast cancer.
The relatively high frequency of deaths of patients with RA due to viral pneumonia documented in the authors’ retrospective analysis (20.0%) fits into the range of data from other researchers and logically agrees with the above data of the comorbid background, in the structure of which COVID-19 infection ranked third along with oncopathologies. The revealed fact to some extent echoes the data of Varela et al. [31], according to which, in the cohort of patients with established RA, the main causes of death were CVDs and COVID-19 infection.
Sepsis was registered as the fourth leading cause of death of patients with RA in the SRCH cohort. RA itself is known to be independently associated with increased mortality from sepsis. In the structure of the causes of deaths in RA patients, a high proportion of sepsis (31.4%) is distinguished with its pronounced tendency to increase in recent years [37][38]. This may be quite logical due to the high infectious risk characteristic of RA, due to a general violation of the immune system characteristic of autoimmune diseases, combined with the iatrogenic effect of corticosteroids and immunosuppressive drugs. Cohort studies often report the development of severe infections and septic shock in patients with RA against the background of the use of anti-rheumatoid medicines [39].
At the same time, the authors of this particular study registered a relatively low proportion of deaths of patients with RA due to sepsis (13.33%). Interpreting the obtained results in the light of the available literature over the past few years, the authors found only one study [40] involving patients with RA and showing a mortality rate caused by sepsis (14%), almost similar to that in the cohort of patients studied by the authors. This difference in results is probably due to the peculiarities of therapeutic tactics in severe infections and the appointment of basic disease-modifying antirheumatic medicines (DMAMs). There is evidence [40, 41] that the use of biological DMAMs in comparison with synthetic DMAMs significantly reduces the risk of sepsis and death after severe infection in patients with RA. However, this can only partially explain the features of the data obtained in this study, since the authors were unable to obtain complete information about the number of patients receiving biological DMAMs, in particular information about the timing of the appointment and duration of use of these medicines.
Conclusion
Thus, in this particular research, the authors attempted to obtain and analyze fresh information on the prevalence and spectrum of comorbid conditions, as well as data on the structure of mortality in patients of the Stavropol Territory SRCH cohort with an established diagnosis of RA. The data obtained carry information that can be used by rheumatologists to optimize the management strategy of RA and the risk of comorbid conditions.
The main advantage of the study was that the study included patients with a reliably established diagnosis of RA. This approach prevented the omission of deaths of patients with undiagnosed RA. In addition, information from surveys and self-reports of patients was not processed, but accurate data from medical databases and documentation were used. The weak side of this work was the costs of the retrospective nature of the study. It was not possible to get the full range of necessary information. In particular, information about bad habits, stress, employment status, and socio-demographic factors, which, according to a number of opinions [6][42], can influence the outcome of RA and are considered independent predictors of mortality in this pathology, were not taken into account. This placed the results of this research in the rank of preliminary and determined the tasks of further research.
References
1. Figus F.A., Piga M., Azzolin I., McConnell R., Iagnocco A. Rheumatoid arthritis: Extra-articular manifestations and comorbidities. Autoimmunity reviews. 2021;20(4):102776. DOI:10.1016/j.autrev.2021.102776
2. Taylor P.C., Atzeni F., Balsa A., Gossec L., Müller-Ladner U., Pope J. The key comorbidities in patients with rheumatoid arthritis: a narrative review. Journal of clinical medicine. 2021;10(3):509. DOI:10.3390/jcm10030509
3. Naimova S.A. Renal comorbidity in rheumatoid arthritis. Web of Scientist: International Scientific Research Journal. 2022;3(6):774-781. DOI:10.17605/OSF.IO/VG4R3
4. Hannech E., Tekaya A.B., Saidane O., Leila R., Bouden S., et al. AB0309 Association between rheumatic disease comorbidity index and pulmonary involvement in rheumatoid arthritis. Annals of the Rheumatic Diseases. 2022;81:1280. DOI:10.1136/annrheumdis-2022-eular.3884
5. Laila D., Jain K., Nandagudi A., Bharadwaj A. AB0165 Malignancy as predominant cause of death in rheumatoid arthritis: review of data from ‘Basildon early arthritis cohort. Annals of the Rheumatic Diseases. 2022;81:1212. DOI: 10.1136/annrheumdis-2022-eular.1572
6. Pedersen J.K., Holst R., Primdahl J., Svendsen A.J., Hørslev-Petersen K. Mortality and its predictors in patients with rheumatoid arthritis: a Danish population-based inception cohort study. Scandinavian Journal of Rheumatology. 2018;47(5):371-377. DOI: 10.1080/03009742.2017.1420223
7. Gordeev A., Galushko E. AB0328 Assessing the multimorbid profile (CIRS) in refractory rheumatoid arthritis. Annals of the Rheumatic Diseases. 2022;81:1288. DOI:10.1136/annrheumdis-2022-eular.3084
8. Uzun G.S., Bahap M., Yucel O., Kaygusuz Y., Bilgin E., et al. AB0282 Comorbidities are more important than jak inhibitors: venous thromboembolism in rheumatoid arthritis. Annals of the Rheumatic Diseases. 2022;81:1267-1268. DOI: 10.1136/annrheumdis-2022-eular.3084
9. Abdrakhmanova A.I., Amirov NB., Tsibulkin N.A. Painless myocardial ischemia as a manifestation of coronary heart disease in patients with rheumatoid arthritis. Bulletin of modern clinical medicine. 2020;13(2):50-55. (In Russ). DOI: 10.20969/VSKM.2020.13(2).50-55
10. Yu K.H., Chen H.H., Cheng T.T., Jan Y.J., Weng M.Y., et al. Consensus recommendations on managing the selected comorbidities including cardiovascular disease, osteoporosis, and interstitial lung disease in rheumatoid arthritis. Medicine. 2022;101(1):e28501. DOI:10.1097/MD.0000000000028501
11. Dougados M. Comorbidities in rheumatoid arthritis. Current opinion in rheumatology. 2016;28(3):282-288. DOI: 10.1097/BOR.0000000000000267
12. Díaz Cuña C., Consani S., Rostan S., Fernández L., Moreira E., Sanmartí R. Artritis reumatoide: manifestaciones extraarticulares y comorbilidades. Rev Colomb Reumatol. 2022. DOI:10.1016/j.rcreu.2021.03.015
13. Abhishek A., Nakafero G., Kuo C.F., Mallen C., Zhang W., et al. Rheumatoid arthritis and excess mortality: down but not out. A primary care cohort study using data from Clinical Practice Research Datalink. Rheumatology. 2018;57(6):977-981. DOI: 10.1093/rheumatology/key013
14. Almutairi K., Nossent J., Preen D., Keen H., Inderjeeth C. OP0100-HPR The influence of comorbidity on mortality in patients with rheumatoid arthritis 1980-2015: a longitudinal population-based study in western Australia. Annals of the Rheumatic Diseases. 2021;80:55-56. DOI:10.1136/annrheumdis-2021-eular.340
15. Poppelaars P.B., Van Tuyl L.H., Boers M. Normal mortality of the COBRA early rheumatoid arthritis trial cohort after 23 years of follow-up. Annals of the rheumatic diseases. 2019;78(5), 586-589. DOI:10.1136/annrheumdis-2018-214618
16. Sparks J.A., Chang S.-C., Liao K.P., Lu B., Fine A.R., et al. Rheumatoid Arthritis and Mortality Among Women During 36 Years of Prospective Follow-Up: Results From the Nurses’ Health Study. Arthritis Care & Research. 2016;68(6):753–762. DOI:10.1002/acr.22752
17. Daniel C.M., Davila L., Makris U.E., Mayo H., Caplan L., et al. Ethnic disparities in atherosclerotic cardiovascular disease incidence and prevalence among rheumatoid arthritis patients in the United States: A systematic review. ACR open rheumatology.2020;2(9):525-532. DOI:10.1002/acr2.11170
18. Lala V., Tikly M., Musenge E., Govind N. Comorbidities in Black South Africans with established rheumatoid arthritis. International Journal of Rheumatic Diseases. 2022;25(6):699-704.DOI:10.1111/1756-185X.14328
19. Jagpal A., Navarro-Millán I. Cardiovascular co-morbidity in patients with rheumatoid arthritis: a narrative review of risk factors, cardiovascular risk assessment and treatment. BMC rheumatology. 2018;2(10):1-14. DOI: 10.1186/s41927-018-0014-y
20. Aletaha D., Neogi T., Silman A.J., Funovits J., Felson D.T., et al. Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62:2569-2581. DOI: 10.1002/art.27584
21. Kalinina E.V., Babaeva A.R., Levitskaya A.V., Zvonorenko M.S. Otsenka komorbidnosti u bol'nykh revmatoidnym artritom. Vserossiiskii kongress s mezhdunarodnym uchastiem «Dni revmatologii v Sankt-Peterburge-2018»; Noyabr' 01-03, 2018; St. Petersburg. (In Russ). eLIBRARY ID: 36909194
22. Kasimova M.B., Pulatova Sh.B. Sochetaemost' revmatoidnogo artrita s drugimi zabolevaniyami. Vserossiiskii kongress s mezhdunarodnym uchastiem «Dni revmatologii v Sankt-Peterburge-2018»; Noyabr' 01-03, 2018; St. Petersburg. (In Russ). eLIBRARY ID: 36909194.
23. An J., Nyarko E., Hamad M.A. Prevalence of comorbidities and their associations with health-related quality of life and healthcare expenditures in patients with rheumatoid arthritis. Clinical rheumatology.2019;38(10):2717-2726. DOI:10.1007/s10067-019-04613-2
24. Batko B., Urbański K., Świerkot J., Wiland P., Raciborski F., et al. Comorbidity burden and clinical characteristics of patients with difficult-to-control rheumatoid arthritis. Clinical Rheumatology. 2019;38(9):2473-2481. DOI:10.1007/s10067-019-04579-1
25. Kozlova V.I., Skrynnik E.I. Komorbidnost' u patsientov s revmatoidnym artritom. Sbornik tezisov mezhdunarodnoi nauchno-prakticheskoi konferentsii studentov i molodykh uchenykh «Aktual'nye problemy sovremennoi meditsiny i farmatsii»; 2019; Minsk. (In Russ).
26. Raskina T., Malyshenko O., Usova E., Letaeva M., Averkieva J. AB1228 COMPARATIVE Analysis of comorbid pathology in patients with rheumatoid arthritis and ankylosing spondylitis. Annals of the Rheumatic Diseases. 2020;79:1905 DOI: 10.1136/annrheumdis-2020-eular.5650
27. Gutierrez J.C., Jiménez B.R., Pineda M.L., Rojas-Giménez, M., Castro R.O., et al. AB0166 Mortality and comorbidities in a cohort of pacients with established rheumatoid arthritis. Annals of the Rheumatic Diseases. 2021;80:1109-1110. DOI:10.1136/annrheumdis-2021-eular.3082
28. Tekaya A.B, Hannech E., Saidane O., Bouden S., Leila R., et al. POS0620 Rheumatic disease comorbidity index: it is a predictor of outcomes in rheumatoid arthritis? Annals of the Rheumatic Diseases. 2022;81:578 DOI:10.1136/annrheumdis-2022-eular.3778
29. Hannech E., Tekaya A.B., Saidane O., Bouden S., Leila R., et al. AB0291 Comorbidities profiles in seropositive rheumatoid arthritis versus seronegative rheumatoid arthritis. Annals of the Rheumatic Diseases. 2022;81:271-1272. DOI:10.1136/annrheumdis-2022-eular.3336
30. Miura T., Miyakoshi N., Kashiwagura T. et al. The association between comorbidities and disease activity in patients with rheumatoid arthritis: a multicenter, cross-sectional cohort study in Japan with the highest proportion of elderly individuals. Egypt Rheumatol Rehabil.2022;49:7. DOI:10.1186/s43166-021-00109-7
31. Varela D.C., Monroy J.S., Ribero M.M., Villota C., Rodriguez-Jimenez M., Hernández R.M. AB0314 Multimorbidity burden in rheumatoid arthritis. Annals of the Rheumatic Diseases. 2022;81:1282. DOI: 10.1136/annrheumdis-2022-eular.4180
32. Savushkina N.M., Demidova N.V., Galushko E.A., Gordeev A.V. Vliyanie mul'timorbidnosti na aktivnost' revmatoidnogo artrita. Vserossiiskii kongress s mezhdunarodnym uchastiem «Dni revmatologii v Sankt-Peterburge-2018»; Noyabr' 01-03, 2018; St. Petersburg. (In Russ). eLIBRARY ID: 36909194.
33. Trubnikova N.S., Shilova L.N., Aleksandrov A.V. Comorbid background problems in patients with rheumatoid arthritis. Bulletin of the Volgograd State Medical University. 2019;2(70):12-16. (In Russ). DOI:10.19163/1994-9480-2019-2(70)-12-16
34. Demina A.B., Radenska-Lopovok S.G., Folomeeva O.M., Erdes Sh.F. Analysis of the structure of lethal outcomes and causes of death in rheumatic diseases in Moscow. Scientific and practical rheumatology. 2004;(2):6. (In Russ).
35. Trukhan D.I., Ivanova D.S., Belus K.D. Rheumatoid arthritis and traditional cardiovascular risk factors: current aspects of real clinical practice. Consilium Medicum, 2020;22(1):19-25. (In Russ). DOI:10.26442/20751753.2020.1.200052
36. Provan S.A., Lillegraven S., Sexton J., Angel K., Austad C., et al. Trends in all-cause and cardiovascular mortality in patients with incident rheumatoid arthritis: a 20-year follow-up matched case-cohort study. Rheumatology. 2020;59(3):505-512. DOI:10.1093/rheumatology/kez371
37. Krasselt M., Baerwald C., Petros S., Seifert O. Mortality of sepsis in patients with rheumatoid arthritis: A single-center retrospective analysis and comparison with a control group. Journal of Intensive Care Medicine. 2021;36(7):766-774. DOI: 10.1177/0885066620917588
38. Iyer P., Gao Y., Field E.H., Curtis J.R., Lynch C.F., Vaughan-Sarrazin M., Singh N. Trends in Hospitalization Rates, Major Causes of Hospitalization, and In Hospital Mortality in Rheumatoid Arthritis in the United States From 2000 to 2014. ACR open rheumatology. 2020;2(12):715-724. DOI: 10.1002/acr2.11200
39. Favalli E.G., Ingegnoli F., De Lucia O., Cincinelli G., Cimaz R., Caporali R. COVID-19 infection and rheumatoid arthritis: Faraway, so close! Autoimmunity reviews. 2020;19(5):102523. DOI: 10.1016/j.autrev.2020.102523
40. Tzagkarakis E., Flouri I., Facondi I., Kalogiannaki E., Ilia S., Briassoulis G., Sidiropoulos P. AB0265 Rheumatoid arthritis patients hospitalized for a serious infection have high incidence of sepsis while those on bDMARDs HAVE lower mortality compared to those on csDMARDs. Annals of the Rheumatic Diseases. 2022;81:1259. DOI: 10.1136/annrheumdis-2022-eular.2064
41. Richter A., Listing J., Schneider M., Klopsch T., Kapelle A., et al. Impact of treatment with biologic DMARDs on the risk of sepsis or mortality after serious infection in patients with rheumatoid arthritis. Annals of the rheumatic diseases. 2016;75(9):1667-1673. DOI: 10.1136/annrheumdis-2015-207838
42. Busby A.D., Wason J., Pratt A.G., Young A., Isaacs J.D., Nikiphorou E. The role of comorbidities alongside patient and disease characteristics in long-term disease activity in RA using UK inception cohort data. Rheumatology. 2022; DOI: 10.1093/rheumatology/keac139
About the Authors
I. N. ShchendriginRussian Federation
Ivan N. Shchendrigin - Cand. Sci. (Med.), Chief Physician, Stavropol Regional Clinical Hospital.
Stavropol.
Competing Interests:
None
V. N. Mazharov
Russian Federation
Viktor N. Mazharov - Cand. Sci. (Med.), Rector, State Medical University.
Stavropol.
Competing Interests:
None
Review
For citations:
Shchendrigin I.N., Mazharov V.N. The profile of comorbid conditions and the structure of mortality in patients with rheumatoid arthritis in the Stavropol Territory: preliminary results. Medical Herald of the South of Russia. 2022;13(3):173-182. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-3-173-182







































