Scroll to:
Estimation of vascular stiffness in patients with arterial hypertension and atherosclerosis of the lower limb arteries taking into account hypolipidemic therapy
https://doi.org/10.21886/2219-8075-2022-13-3-127-136
Abstract
Objective: estimation of parameters of vascular stiffness in patients with arterial hypertension (AH) and atherosclerosis of the arteries of the lower extremities (AALE) taking into account statin therapy. Materials and methods: 120 patients with AH were divided into 3 groups: group 1 — 46 patients with AH and clinically manifested AALE, group 2 — 39 patients with AH and asymptomatic AALE, group 3 — 35 patients with AH without AALE. The patients of each group were divided into 2 subgroups: the 1st subgroup — not receiving statins, the 2nd subgroup — taking statins. All patients underwent laboratory and instrumental studies, including the determination of vascular stiffness parameters using the Vasotens software («Peter Telegin», Nizhny Novgorod) and ultrasonic triplex scanning of the arteries of the lower extremities. Statistical data processing was carried out using Microsoft Office Excel 16 (2015, Microsoft, USA), Statistica 10.0 (StatSoft, USA), IBM SPSS Statistica 26.0 (IBM, USA). Results: lower values of total cholesterol were found in patients of the 2nd subgroup of all studied groups (p<0,05), as well as lower values of low-density lipoprotein cholesterol (LDLС) among patients of the 2nd subgroup of the second and third groups (<0,05). In patients of all groups, when using statins, the target values of LDLC were not achieved. Lower values of the arterial stiffness index (ASI) and augmentation index (AIx) were found in patients of the first group of the 2nd subgroup receiving statins in comparison with patients of the 1st subgroup (p<0,05). In patients of the second group of the 2nd subgroup, while taking statins, there was a clear trend towards a lower ASI value compared to the 1st subgroup (p=0.07). Conclusions: the use of statins in patients with hypertension and AALE of varying severity, despite the lack of achievement of target levels of LDLC, contributed to a decrease in vascular stiffness, and, consequently, a decrease in cardiovascular risk.
Keywords
For citations:
Sementsova N.A., Chesnikova A.I., Safronenko V.A., Skarzhinskaya N.S. Estimation of vascular stiffness in patients with arterial hypertension and atherosclerosis of the lower limb arteries taking into account hypolipidemic therapy. Medical Herald of the South of Russia. 2022;13(3):127-136. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-3-127-136
Introduction
Cardiovascular diseases (CVDs) are among the main causes of death in the world [1]. Significant risk factors for the development of cardiovascular pathology include arterial hypertension (AH) and atherosclerosis.
It is widely known that hypertension and atherosclerotic lesions of vascular walls are often components of comorbid pathology [2]. Hypertension is one of the factors contributing to the development of atherosclerosis, while atherosclerosis contributes to the progression of hypertension [3]. The combination of hypertension and atherosclerosis of various vascular basins leads to more rapid development of such CVDs as coronary heart disease, cerebral circulatory disorders, and ischemia of the lower extremities.
The results of numerous studies indicate the effect of increased blood pressure on lipid metabolism [4, 5]. Therefore, the activation of the renin-angiotensin-aldosterone system occurs with an increase in blood pressure, which leads to an additional acceleration of the processes of atherogenesis due to the stimulating effect on angiotensin type 1 (AT-1) receptors [6–9].
An increase in the level of low-density lipoprotein (LDL) cholesterol is associated with an increase in the content of free radicals, which are important in the development of both hypertension and atherosclerosis [10]. As a rule, endothelial dysfunction associated with impaired nitric oxide synthesis, an increase in endothelin-1 production and vasoconstriction lead to an increase in vascular wall stiffness [11–13].
Recently, special attention has been paid to the assessment of vascular stiffness, which is considered an independent marker of arterial damage as a target organ [14]. In clinical practice, the determination of arterial wall stiffness parameters, especially in comorbid AH patients, allows the timely identification of patients with a high risk of cardiovascular events [15].
As is known, antihypertensive and hypolipidemic therapy has a significant effect on the parameters of arterial rigidity. In this regard, one of the criteria for the effectiveness of therapy in patients with hypertension and atherosclerosis of the arteries of various basins is to achieve the target values of blood pressure and LDL cholesterol. Unfortunately, in real practice, not all patients with hypertension and peripheral atherosclerosis receive lipid-lowering therapy, primarily statins, and in a smaller percentage of cases, the achievement of target values of LDL cholesterol is monitored.
The purpose of the study was to evaluate the parameters of vascular stiffness in patients with AH and atherosclerosis of the arteries of the lower extremities (AALE), taking into account statin therapy.
Materials and methods
The study included 120 patients suffering from hypertension; the average age was 62.1±3.12. The duration of hypertension and the degree of hypertension did not significantly differ in all patients of the study (p>0.05). The exclusion criteria from the study were acute coronary syndrome, transient ischemic attack or acute cerebrovascular accident during the last six months, secondary forms of hypertension, severe cardiac arrhythmias, congenital and acquired heart defects, and decompensation of renal or hepatic insufficiency. The study was conducted in the conditions of the Rostov Regional Clinical Hospital of Rostov-on-Don.
The work was carried out in accordance with the standards of the Helsinki Declaration, approved by the independent ethics Committee of the Federal State Budgetary Educational Institution of Higher Education “Rostov State Medical University” of the Ministry of Health of the Russian Federation, Protocol No. 20/14 dated December 25, 2014. All the people included in the study signed a written informed voluntary consent.
All patients were divided into three main groups depending on the presence and clinical manifestations of AALE. The first group included 46 patients with hypertension and clinically manifested AALE, the average age was 61.7±5.5 years, the second group included 39 patients with hypertension and asymptomatic AALE, the average age was 63.8±8.1 years, and the third group consisted of 35 patients with hypertension without AALE, the average age was 60.8±8 years.
Each group of patients was divided into two subgroups taking into account statin intake: in the 1st subgroup, patients did not receive hypolipidemic therapy, and in the 2nd subgroup they received statins, while there were no significant differences in the frequency of statin use between the groups (30%, 48%, and 37% in the 1st, the 2nd and the 3rd groups, respectively, p = 0.22). Patients were assigned to the 2nd subgroup in the cases when the duration of statin intake at the time of hospitalization was more than one year. The first group of patients received atorvastatin at an average dose of 17.7 ± 4.4 mg, rosuvastatin at a dose of 10 mg, in the second group the average dose of simvastatin was 15±7 mg, atorvastatin — 20±7.7 mg, rosuvastatin — 11.67 ±4 mg, and in the third group atorvastatin was prescribed at an average dose of 21 ± 7.4 mg, rosuvastatin — 6.67±2.9 mg.
The groups of patients did not differ statistically significantly in the degree of hypertension determined by the office measurement of blood pressure (p>0.05). In the first group, in 22% of patients, blood pressure corresponded to the 1st degree of hypertension, in 39% – the 2nd and in 39% — the 3rd degree of hypertension. In the second group, 31% of patients had the 1st degree of hypertension, 36% had the 2nd degree, and 33% had the 3rd degree of hypertension. In patients of the third group, the 1st and 2nd degrees of hypertension were established in 34% of cases, and the 3rd degree of hypertension was established in 32% of patients. When determining the stage of essential hypertension (EH), it was revealed that among the patients of the first group, all the patients had stage III of EH (100%), and among the patients of the 2nd group, stage III (90%) was established in 90% of cases and stage II of EH – in 10%. The third group consisted of 37% of patients with stage II and 63% with stage III of EH; the differences between the groups were statistically significant (p=0.007). Taking into account the anamnesis data and the results of the studies, 16.2% of the study patients were classified as having high cardiovascular risk, and 83.8% – very high.
All the patients with hypertension received antihypertensive therapy in accordance with clinical recommendations [16], while the frequency of prescribing different classes of drugs did not significantly differ. Despite the ongoing antihypertensive therapy, the target values of blood pressure were not achieved in all patients included in the study.
The severity of atherosclerotic lesions of the arteries of the lower extremities was assessed according to ultrasound triplex scanning. According to the generally accepted Fontaine-Pokrovsky classification [17], based on the clinical manifestations of the disease, almost half (45.9%) of patients with AALE were diagnosed with stage I of pelvic limbs chronic ischemia, which allowed them to be assigned to the second group — with hypertension and asymptomatic AALE. In the first group, stage II was registered in 27.1% of cases, stage III in 15.3% of cases, and stage IV in 11.7% of patients.
Among the patients with hypertension and concomitant AALE, there were significantly more men than women (p<0.001). In the group of patients with hypertension and severe AALE, smokers were more common (61%), which significantly differed from the indicators in the second (31%, p=0.006) and third (26%, p=0.002) groups.
The patients underwent standard laboratory and instrumental methods of research. When performing laboratory tests, lipid profile parameters were evaluated with an assessment of the values of total cholesterol (TCH), LDL cholesterol, high-density lipoprotein (HDL) cholesterol, and triglycerides (TG).
Vascular stiffness parameters were determined during the 24-hour blood pressure monitoring on the BP Lab device (Peter Telegin, Moscow, Nizhny Novgorod) by means of using the Vasotens software. The following indicators were evaluated: reflected wave transit time (RWTT), pulse wave velocity in the aorta (PWVao), arterial stiffness index (ASI), augmentation index (AIx), the maximum rate of increase in blood pressure (dP/dtmax), and ambulatory arterial stiffness index (AASI).
Statistical processing of the results was carried out using Microsoft Office Excel 16 (2015, Microsoft, USA), Statistica 10.0 (StatSoft, USA), and IBM SPSS Statistica 26.0 (IBM, USA). To determine statistically significant differences in quantitative data, a comparative analysis was performed using parametric (Student's t-test, ANOVA method) and nonparametric (Mann-Whitney, Kruskal-Wallis) criteria. It was believed that at p>0.05, there were no statistically significant differences. In the intergroup comparison, a posteriori analysis was carried out with the Bonferroni correction. Statistically significant differences in values were recognized at the level of p<0.017 in the case of comparison of 3 groups. Correlation analysis was performed using Spearman's rank correlation coefficient.
Results
Comparative characteristics of lipid profile values in patients of the studied groups are shown in Figure 1.
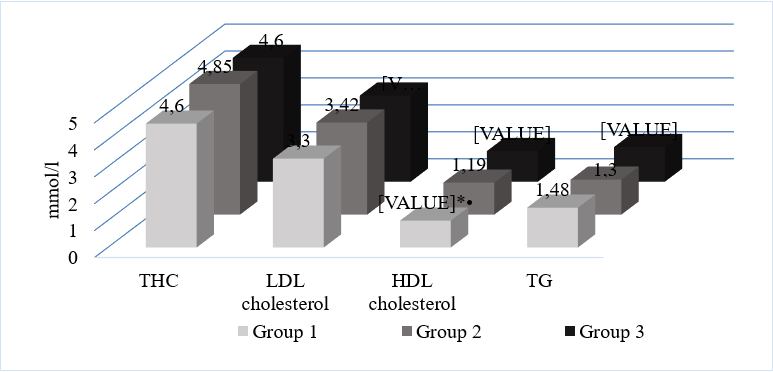
Figure 1. Comparative characteristics of lipid profile values in patients of the studied groups.
Note: THC — total cholesterol; LDL cholesterol — low density lipoprotein cholesterol; HDL cholesterol — high density lipoprotein cholesterol; TG — triglycerides; * — p<0,05 in comparison with the 2nd group; • — p<0,05 in comparison with the 3rd group; post hoc analyzes were performed with Bonferroni correction.
The values of THC, LDL cholesterol, and TG did not differ statistically significantly when compared between the groups (p>0.05). The level of HDL cholesterol in patients with hypertension and severe AALE (1±0.3 mmol/l) was significantly lower than in patients of the second (1.19±0.3 mmol/l, p=0.009) and third (1.14±0.26 mmol/l, p=0.04) groups.
The comparative analysis of the intake of different classes of statins and their doses in the studied groups of patients is presented in Figure 2.
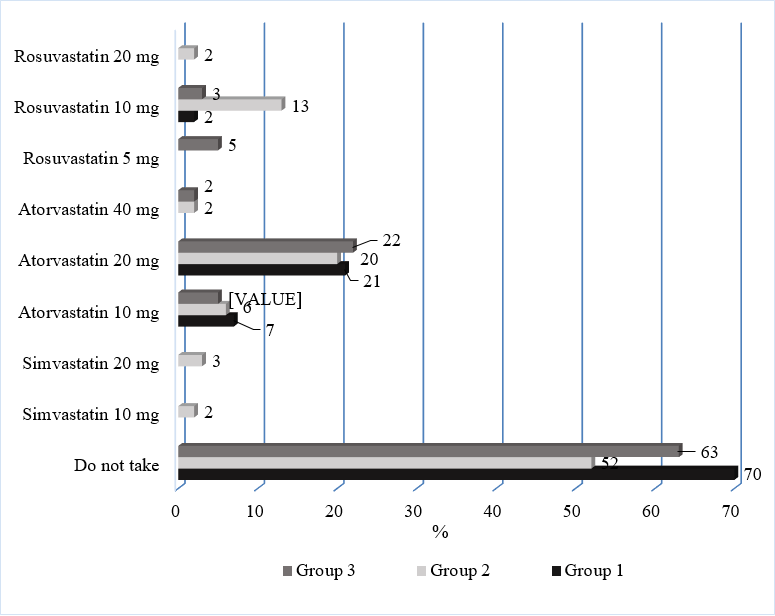
Figure 2. Distribution of patients taking into account the use of different classes of statins and their doses in patients of the study groups.
The assessment of lipid profile indicators in patients suffering from hypertension and AALE of varying severity is of particular interest, taking into account statin intake.
The comparative characteristics of the lipid profile indicators of the 1st and 2nd subgroups of the studied groups are shown in Figure 3.
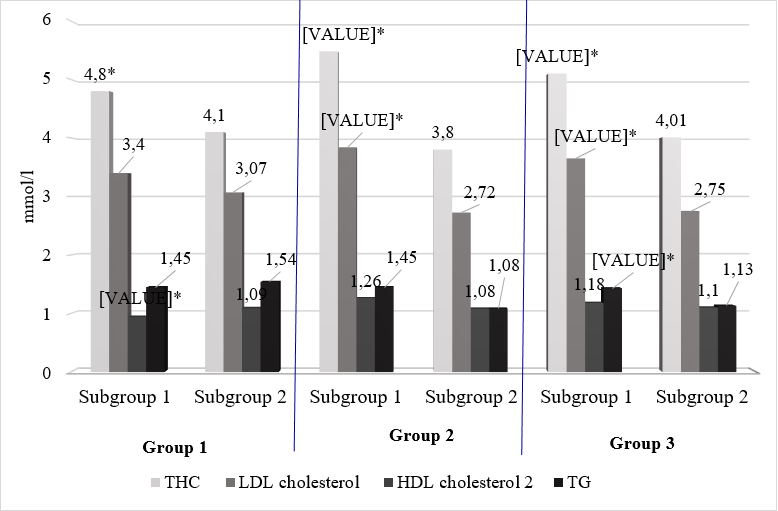
Figure 3. Comparative characteristics of lipid profile values in patients of the 1st and 2nd subgroups of the studied groups.
Note: THC — total cholesterol; LDL cholesterol — low density lipoprotein cholesterol; HDL cholesterol — high density lipoprotein cholesterol; TG — triglycerides; * — p<0,05 in comparison with the 2nd subgroup
The analysis of the obtained data indicates statistically significantly higher values of THC (mmol/l) in the 1st subgroup in comparison with the indicators in the 2nd subgroup in patients of all the groups (p<0.05). The level of LDL cholesterol (mmol/l) was significantly lower in patients of the 2nd subgroup compared with patients not taking statins, among patients of the second (3.84 mmol/l vs. 2.72 mmol/l, p=0.001) and the third (3.65 mmol/l vs. 2.75 mmol/l, p=0.004) groups. Statistically significant differences in HDL cholesterol values between the subgroups were found in patients with hypertension and severe AALE (0.94 mmol/l vs. 1.09 mmol/l, p=0.031). The significantly lower level of TG (mmol/l) while taking statins was determined in a group of patients with hypertension without peripheral atherosclerosis (1.43 mmol/l vs. 1.13 mmol/l, p =0.041).
Despite the ongoing therapy, the target values of LDL cholesterol for patients with high and very high cardiovascular risk (1.8 mmol/L and 1.4 mmol/L, respectively) were not achieved in all patients of the study, due to the appointment of low doses of statins, lack of control over the achievement of target values, as well as, possibly, low adherence to hypolipidemic therapy.
The comparative characteristics of vascular stiffness parameters in patients of the 1st and 2nd subgroups of the first group are presented in Table 1.
Table 1
Comparative characteristics of vascular stiffness parameters in patients of the first and second subgroups of the first group
|
No. |
Parameter |
1st subgroup |
2nd subgroup |
р |
|
1. |
RWTT, ms |
119 [ 109;133] |
120 [ 114;130] |
0.06 |
|
2. |
PWVao, m/s |
10.9[ 10.3;11.8] |
11 [ 10.2;12.4] |
0.59 |
|
3. |
ASI, mmHg. |
186.5 [ 151;220] |
168 [ 139;191] |
0.03 |
|
4. |
AIX, % |
14 [ -0.75;31] |
6 [ -11.7;23.5] |
0.02 |
|
5. |
dP/dtmax, mmHg /s |
564 [ 462;701] |
537 [ 461;633] |
0.27 |
|
6. |
AASI |
0.49 [ 0.43;0.63] |
0.46 [ 0.28;0.59] |
0.14 |
Analysis of the data obtained indicates statistically significantly lower values of ASI and Ip in patients of the 2nd subgroup in comparison with patients not receiving statins (p<0.05). When comparing RWTT (ms) in patients of the 1st and 2nd subgroups, a distinct positive trend was revealed to register higher values in patients of the 2nd subgroup (p=0.06). The revealed changes in PASI, AIx and RWTT indicators may indicate a positive effect of statin therapy on vascular stiffness. There were no statistically significant differences between the subgroups when comparing the values of PWVao, dP/dtmax, and AASI (p>0.05).
The comparative characteristics of vascular stiffness parameters in patients of the 1st and 2nd subgroups of the second group are presented in Table 2.
Table 2
Comparative characteristics of vascular stiffness parameters in patients of the first and second subgroups of the second group
|
No. |
Parameter |
1st subgroup |
2nd subgroup |
р |
|
1. |
RWTT, ms |
126.5 [ 122;132] |
127 [ 120;137] |
0.77 |
|
2. |
PWVao, m/s |
10.1 [ 9,4;11,3] |
11.2 [ 9.8;12.2] |
0.17 |
|
3. |
ASI, mmHg. |
165 [ 125;222] |
149 [ 138;175] |
0.07 |
|
4. |
AIX, % |
-5 [ -13.5;11.5] |
-11 [ -19;-3] |
0.25 |
|
5. |
dP/dtmax, mmHg /s |
650.5 [ 488.5;743] |
585 [ 502;681] |
0.56 |
|
6. |
AASI |
0.44 [ 0.32;0.55] |
0.39 [ 0.31;0.49] |
0.39 |
When evaluating the data obtained in patients with hypertension and concomitant asymptomatic AALE, there were no statistically significant differences in vascular stiffness between patients of the 1st and 2nd subgroups (p>0.05). However, after the analysis of the ASI (mmHg) values, a distinct tendency to a lower value of the indicator in patients receiving statins in comparison with patients of the 1st subgroup (p=0.07) was revealed.
The comparative characteristics of vascular stiffness parameters in patients of the 1st and 2nd subgroups of the third group are presented in Table 3.
Table 3
Comparative characteristics of vascular stiffness parameters in patients of the first and second subgroups of the third group
|
No. |
Parameter |
1st subgroup |
2nd subgroup |
р |
|
1. |
RWTT, ms |
125 [ 113;128] |
125.5[ 123;129] |
0.044 |
|
2. |
PWVao, m/s |
11.3[ 10.3;11.7] |
10 [ 9.3;10.9] |
0.004 |
|
3. |
ASI, mmHg. |
173[ 139;187] |
169[ 127;199] |
0.99 |
|
4. |
AIX, % |
-11 [ -28;4.2] |
-14 [ -20;-2.5] |
0.77 |
|
5. |
dP/dtmax, mmHg /s |
655[ 574;760] |
603,5[ 522;814] |
0.96 |
|
6. |
AASI |
0.49 [ 0.37;0.55] |
0.35 [ 0.3;0.46] |
0.07 |
The presented data indicate that patients with hypertension without AALE who do not receive statins have higher vascular wall stiffness, as evidenced by statistically significantly lower values of RWTT (p=0.044) and higher values of PWVao (p=0.004) in comparison with patients receiving lipid-lowering therapy.
Discussion
Recently, great attention has been paid to the primary prevention of CVDs. In this regard, it is important to assess subclinical lesions of target organs, one of which is the vascular wall. An increase in vascular stiffness is a marker of a high risk of cardiovascular events. The analysis of such parameters of arterial rigidity as RWTT (ms), PWVao (m/s), ASI (mmHg), AIx (%), AASI, and dp/dtmax (mmHg/s) allows evaluating not only the state of the arterial bed but also the effectiveness of the therapy.
In recent years, some domestic and foreign studies have demonstrated the positive effect of statins on endothelial function and arterial stiffness [18–22]. The results of these studies indicate that there is a direct correlation between the degree of decrease in LDL cholesterol levels against the background of a high-intensity statin therapy regimen and the severity of slowing down of atherosclerotic processes in various vascular basins.
In the present study, the analysis of vascular stiffness parameters taking into account statin intake demonstrated that the highest values of ASI and AIx were recorded among patients of the first group with hypertension and clinically manifested AALE who were not taking statins. The results obtained suggest that, despite the lack of achievement of the target levels of LDL cholesterol and the preservation of dyslipidemia, the use of statins contributed to a decrease in vascular wall stiffness, and consequently, a decrease in cardiovascular risk in patients with hypertension and clinically manifested AALE. Discussing the positive effect of statins on the parameters of arterial rigidity in patients of the first group, it is necessary to take into account the pleiotropic effects of statins, which are associated with stabilization of atherosclerotic plaques, reduction of their tendency to rupture, improvement of endothelial function, suppression of inflammatory activity in the vascular wall, reduction of platelet aggregation and proliferative activity of smooth muscle cells in the artery wall [23, 24]. At the same time, there were no significant differences in arterial rigidity in patients with hypertension and asymptomatic AALE while taking statins.
In patients of the third group with hypertension without peripheral atherosclerosis, significantly lower values of PWVao and higher values of RWTT were revealed against the background of taking statins, which, apparently, is due not only to the effect on the stiffness of the vascular wall even in the absence of atherosclerotic lesion but also to their pleiotropic effect of statins.
It should be noted that the revealed differences in only some parameters of vascular stiffness against the background of statin therapy in patients included in the study are due to the appointment of low-intensity therapy with the failure to achieve the target values of LDL cholesterol, as well as, possibly, discrete intake of lipid-lowering drugs.
Thus, the results of the analysis indicate a low percentage of statin prescribing in patients with hypertension and AALE, the use of low doses of statins and the lack of control over the achievement of the target value of LDL cholesterol in real clinical practice. At the same time, against the background of even low-intensity statin therapy, there is a decrease in vascular stiffness, which is important for reducing the risk of cardiovascular events.
Conclusions
The use of statins as part of the complex therapy of patients with hypertension and concomitant AALE of varying severity helps to reduce the stiffness of the vascular wall, which is due to both the positive effect on the parameters of the lipid profile and the pleiotropic effects of statins.
References
1. Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227-3337. DOI: 10.1093/eurheartj/ehab484
2. Itoga NK, Tawfik DS, Lee CK, Maruyama S, Leeper NJ, Chang TI. Association of Blood Pressure Measurements With Peripheral Artery Disease Events. Circulation. 2018;138(17):1805-1814. DOI: 10.1161/CIRCULATIONAHA.118.033348
3. Evsikov E.M., Vechorko V.I., Teplova N.V., Zhapueva M.H., Artamonova N.G. Factors and mechanisms of arterial hypertension development in patients with atherosclerosis of lower limb arteries. Cardiovascular Therapy and Prevention. 2019;18(1):150-155. (In Russ.) DOI: 10.15829/1728-8800-2019-1-150-155
4. Chen H, Chen Y, Wu W, Cai Z, Chen Z, et al. Total cholesterol, arterial stiffness, and systolic blood pressure: a mediation analysis. Sci Rep. 2021;11(1):1330. DOI: 10.1038/s41598-020-79368-x
5. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137(12):e67-e492. DOI: 10.1161/CIR.0000000000000558
6. Tsioufis C, Andrikou I, Siasos G, Filis K, Tousoulis D. Anti-hypertensive treatment in peripheral artery disease. Curr Opin Pharmacol. 2018;39:35-42. DOI: 10.1016/j.coph.2018.01.009
7. Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, et al. 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(12):e686-e725. DOI: 10.1161/CIR.0000000000000470
8. Barbarash O.L., Kashtalap V.V. Atherosclerosis of peripheral arteries and arterial hypertension. Features of antihypertensive therapy. Medical alphabet. 2019;1(3):12-16. (In Russ.) DOI: 10.33667/2078-5631-2019-1-3(378)-12-16
9. Clement DL. Treatment of hypertension in patients with peripheral arterial disease: an update. Curr Hypertens Rep. 2009;11(4):271-6. DOI: 10.1007/s11906-009-0046-1
10. Zykov MV, Kashtalap VV, Bykova IS, German AI, Karetnikova VN, Barbarash OL. The relationship between multimorbidity and cardiovascular risk in patients with acute coronary syndrome. Russian Cardiology Bulletin. 2018;13(2):59‑65. (In Russ.). DOI: 10.17116/Cardiobulletin201813259
11. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269-1324. DOI: 10.1161/HYP.0000000000000066
12. Abedin M, Tintut Y, Demer LL. Vascular calcification: mechanisms and clinical ramifications. Arterioscler Thromb Vasc Biol. 2004;24(7):1161-70. DOI: 10.1161/01.ATV.0000133194.94939.42
13. Yasmin, McEniery CM, Wallace S, Dakham Z, Pulsalkar P, et al. Matrix metalloproteinase-9 (MMP-9), MMP-2, and serum elastase activity are associated with systolic hypertension and arterial stiffness. Arterioscler Thromb Vasc Biol. 2005;25(2):372. DOI: 10.1161/01.ATV.0000151373.33830.41
14. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041. DOI: 10.1097/HJH.0000000000001940.
15. Karpov Yu.A., Kukharchuk V.V., Boytsov S.A., Voevoda M.I., Gafarov V.V. et al. Consensus statement of the Russian national atherosclerosis society (RNAS). Familial hypercholesterolemia in Russia: outstanding issues in diagnosis and management. The Journal of Atherosclerosis and Dyslipidemias. 2015;2(19):5–16. eLIBRARY ID: 23790210
16. Kobalava Z.D., Konradi A.O., Nedogoda S.V., Shlyakhto E.V., Arutyunov G.P., et al. Arterial hypertension in adults. Clinical guidelines 2020. Russian Journal of Cardiology. 2020;25(3):3786. (In Russ.) DOI: 10.15829/1560-4071-2020-3-3786
17. 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the european society for vascular surgery (ESVS). Russian Journal of Cardiology. 2018;(8):164-221. (In Russ.) DOI; 10.15829/1560-4071-2018-8-164-221
18. Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, et al. Recommendations for Improving and Standardizing Vascular Research on Arterial Stiffness: A Scientific Statement From the American Heart Association. Hypertension. 2015;66(3):698-722. DOI: 10.1161/HYP.0000000000000033
19. Hadi HA, Mahmeed WA, Suwaidi JA, Ellahham S. Pleiotropic effects of statins in atrial fibrillation patients: the evidence. Vasc Health Risk Manag. 2009;5(3):533-51. DOI: 10.2147/vhrm.s4841.
20. Fesenko E.V., Proschaev K.I., Polyakov V.I. Pleiotropic effects of statins therapy and their role in overcoming polymorbidity. Modern problems of science and education. 2012;2:48. eLIBRARY ID: 17689122.
21. Alidadi M, Montecucco F, Jamialahmadi T, Al-Rasadi K, Johnston TP, Sahebkar A. Beneficial Effect of Statin Therapy on Arterial Stiffness. Biomed Res Int. 2021;2021:5548310. DOI: 10.1155/2021/5548310
22. Sahebkar A, Pećin I, Tedeschi-Reiner E, Derosa G, Maffioli P, Reiner Ž. Effects of statin therapy on augmentation index as a measure of arterial stiffness: A systematic review and meta-analysis. Int J Cardiol. 2016;212:160-8. DOI: 10.1016/j.ijcard.2016.03.010
23. Upala S, Wirunsawanya K, Jaruvongvanich V, Sanguankeo A. Effects of statin therapy on arterial stiffness: A systematic review and meta-analysis of randomized controlled trial. Int J Cardiol. 2017;227:338-341. DOI: 10.1016/j.ijcard.2016.11.073
24. Martínez-Vizcaíno V, Cavero-Redondo I, Saz-Lara A, Pozuelo-Carrascosa DP, Notario-Pacheco B, et al. Comparative effect of statins and types of physical exercise on arterial stiffness: Protocol for network meta-analysis. Medicine (Baltimore). 2019;98(20):e15484. DOI: 10.1097/MD.0000000000015484
About the Authors
N. A. SementsovaРоссия
Nadezda A. Sementsova - postgraduate of Department of internal medicine №1, Rostov State Medical University.
Rostov-on-Don.
Competing Interests:
None
A. I. Chesnikova
Россия
Anna I. Chesnikova - Dr. Sci. (Med.), Professor, professor of Department of internal medicine №1, Rostov State Medical University.
Rostov-on-Don.
Competing Interests:
None
V. A. Safronenko
Россия
Victoria A. Safronenko - Ph.D. in Medicine, associate professor at the Department of internal medicine № 1, Rostov State Medical University.
Rostov-on-Don.
Competing Interests:
None
N. S. Skarzhinskaya
Россия
Natal’a S. Skarzhinskaya - Ph.D. in Medicine, associate professor at the Department of internal medicine № 1, Rostov State Medical University.
Rostov-on-Don.
Competing Interests:
None
Review
For citations:
Sementsova N.A., Chesnikova A.I., Safronenko V.A., Skarzhinskaya N.S. Estimation of vascular stiffness in patients with arterial hypertension and atherosclerosis of the lower limb arteries taking into account hypolipidemic therapy. Medical Herald of the South of Russia. 2022;13(3):127-136. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-3-127-136
JATS XML







































