Scroll to:
Possibilities of predicting purulent-inflammatory complications after cesarean section
https://doi.org/10.21886/2219-8075-2022-13-4-73-87
Abstract
Objective: identify the main risk factors in the development of purulent-inflammatory complications after cesarean section. Materials and methods: puerperal women after cesarean section (n = 90): 24 patients with a complication of puerperia in the form of endometritis (group I), 16 — with the insolvency of the suture on the uterus (group II) and 50 — with a physiologically occurring postoperative period (group (III) of control). An analysis of anamnestic, clinical and laboratory studies of puerperal women after abdominal delivery with a complicated postoperative period was carried out. With the help of logistic regression with the construction of an ROC-curve, a rank correlation analysis of the influence of adverse factors with the calculation of diagnostic coefficients (DC) was performed. Results: based on the assessment of the identified main clinical-anamnestic and laboratory predictors, using mathematical modeling methods, a scale for predicting the risk of purulent-inflammatory complications in early puerperia after abdominal delivery has been developed. Conclusion: prognostic mathematical scale for assessing the risk of purulent-inflammatory complications in puerperal women after abdominal delivery makes it possible to identify the main predictors of infectious diseases in these patients, which contributes to their timely prevention and, thereby, reducing the frequency of severe forms of postpartum infection.
Keywords
For citations:
Kutsenko I.I., Borovikov I.O., Galustyan M.V., Magay A.S., Borovikova O.I. Possibilities of predicting purulent-inflammatory complications after cesarean section. Medical Herald of the South of Russia. 2022;13(4):73-87. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-4-73-87
Introduction
The share of septic complications in the structure of maternal mortality is 6.7–12.1%, of which 4.3–5.4% is obstetric sepsis (in the Russian Federation, maternal mortality reaches 3.6%)1 [1][2][3]. At the same time, endometritis is one of the main causes of puerperium infection and accounts for 3–5% of vaginal deliveries and up to 27–30% after cesarean section [4][5][6].
Physiological, immunological, and mechanical changes during pregnancy predispose to the development of purulent-septic complications; especially this applies to urogenital infections and factors associated with medical care, namely, operative childbirth [3][7][8]. According to modern data, the main reasons for the increase in the frequency of postpartum endometritis are chronic diseases, immunosuppressive disorders in the pregnant woman's body, leading to a change in the species composition of microbial flora, the emergence of aggressive forms of bacterial infection, the redistribution of the importance of predisposing factors due to an increase in the number of surgical interventions in childbirth, the widespread introduction of antibiotics and often their irrational use [9][10][11].
The effective prevention, early detection, and adequate management of patients, starting from the pre-gravidar stage and ending with the technique of abdominal delivery, can contribute to reducing the number of infectious complications of puerperium, while their prediction and early diagnosis are the basis for timely therapy and organ-preserving treatment methods [7][12][13][14].
The purpose of this particular study was to assess the most significant risk factors in the development of purulent-inflammatory complications after cesarean section.
Materials and methods
A retrospective non-randomized study. The base of the event was the Department of Obstetrics, Gynecology and Perinatology of the Kuban State Medical University of the Ministry of Health of the Russian Federation, two regional perinatal centers (GBUZ DKKB and KKB No. 2) and GBUZ Maternity Hospital of Krasnodar (period: 01.2020 – 01.2022). Risk factors for postpartum purulent-inflammatory complications of puerperium were determined (analysis of 90 cards of pregnant and maternity women and birth histories of patients delivered by cesarean section). The main two groups were postpartum women with purulent-inflammatory complications of puerperium (n=40): 24 patients (group I) who were diagnosed with “Metroendometritis after cesarean section”, 16 (group II) — with the diagnosis “Metroendometritis after cesarean section. Failure of sutures on the uterus” (ICD10 “O86.0 Infection of surgical obstetric wound”, “O86.8 Other specified postpartum infections”) and the control (III) comparison group (n=50) — maternity women with a physiological course of puerperium after cesarean section.
In order to identify risk factors, a rank correlation analysis was performed, the strength of the influence of the found adverse factors on the outcome was evaluated using logistic regression, sensitivity and selectivity were determined by constructing a ROC curve. The diagnostic coefficient (DC) of each of the identified predictors was calculated (Kulbach's formula using sequential Wald analysis): (DC =10 Lg P1/P2), where P1 is the relative frequency of the trait in the first verified state, expressed in decimal quantity (DQ), P2 is the relative frequency of the trait in the second verified state. Based on the data obtained, a scale for assessing the degree of infection risk was developed.
The ethical principles presented by the Helsinki Declaration of the World Medical Association “Ethical Principles of Scientific and Medical Research with Human Participation” (as amended in 2008), “Rules of Clinical Practice in the Russian Federation” (Order of the Ministry of Health and Social Development of the Russian Federation No. 266 dated June 19, 2003) were observed in the study. It is noted in the Protocol No. 12 of February 19, 2020 of the meeting of the Ethical Committee for conducting scientific research of KubSMU.
The obtained results were subjected to statistical processing with the calculation of the arithmetic mean (M) and standard deviation (s) taking into account the reliable probability according to the Student-Fisher criterion using software (R, version 3.1.1 for Windows, R Foundation, http://www.r-project.org/). The permissible percentage of errors of the first and second kinds was set no more than 5% (p<0.05).
Results
The patients included in the study (n=90) aged 19–38 years (average age — 27.5±5.9 years) differed depending on the group of complications of the postoperative period (Table 1, Figures 1–3). Thus, in group I (metroendometritis after cesarean section), the average age was 26.9±4.6 years, while the age of 25–29 years prevailed (37.5%, CI — 95%, 29.7–40.1%), in group II (metroendometritis after cesarean section, failure of sutures on the uterus) — 32.1± 4.3 years with the predominance of the age group 30–35 years (50.0%, DI — 95%, 43.9–55.0%). In the control group, the average age was 26.2±4.8 years with a predominance of postpartum women aged 25–29 years (46.0%, CI — 95%, 38.1–48.3%) ( p=0.946).
Table 1
Postpartum women age
|
Group |
Age (years) |
|||||||
|
18–24 |
25–29 |
30–35 |
36–38 |
|||||
|
n |
% |
n |
% |
n |
% |
n |
% |
|
|
I (n=24) |
6 |
25,0 |
9 |
37,5 |
7 |
29,2 |
2 |
8,3 |
|
II (n=16) |
2 |
12,5 |
5 |
31,2 |
8 |
50,0 |
1 |
6,3 |
|
III (n=50) |
11 |
22,0 |
23 |
46,0 |
12 |
24,0 |
4 |
8,0 |
|
χ²; p1-2 |
4,296; >0,05 |
2,886; >0,05 |
11,004; <0,01 |
0,308; >0,01 |
||||
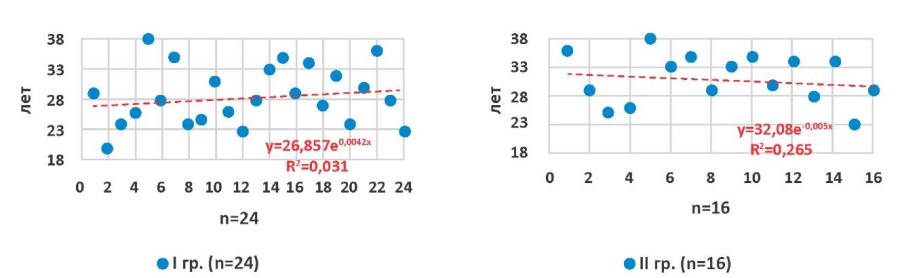
Figure 1. Age parameters of groups with complications after cesarean section
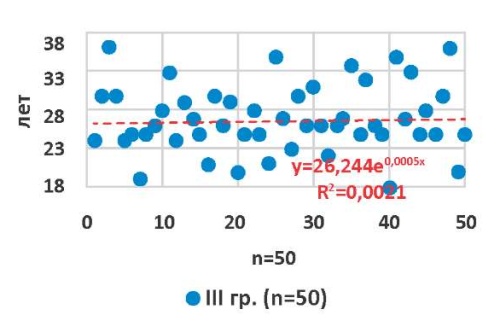
Figure 2. Age parameters of the group with normal course of puerperia (control)
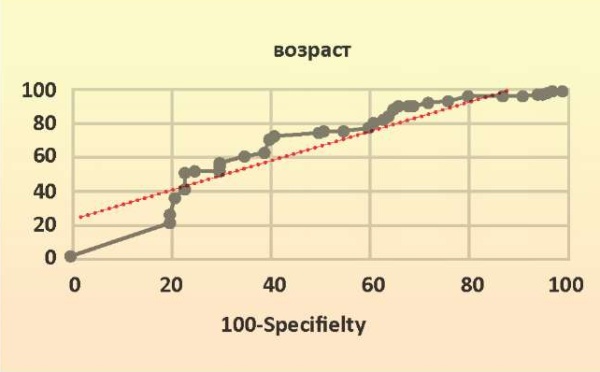
Figure 3. ROC curve (dotted 95%CI AUC) constructed by analyzing the prognostic sensitivity and selectivity of postpartum women age
The data obtained using rank correlation, ROC analysis, and logistic regression determine anamnestic and clinical signs, on the basis of which it is possible to predict the outcome of the postpartum period with a high degree of reliability in women delivered by cesarean section, showed that with respect to the age indicators of maternity hospitals, the ROC curve and the analysis of the area under the curve (AUC), constructed by analyzing the sensitivity and specificity of age for predicting the outcome: AUC=0.62 (CI — 95%, 0.53–0.71%), p=0.014, cut-off threshold — >35 years, sensitivity — 50% (CI — 95% 38.5–61.5%), specificity — 73.5% (CI — 95% 58.9–85.1%). The majority of the operated women (51/90; 56.7%) were housewives and had a specialized secondary (36/90; 40.0%) or secondary (19/90; 21.1%) education (no reliable (p>0.05) correlation between social status, level of education, place of work, and the appearance of purulent-inflammatory complications after abdominal delivery was revealed).
The parity analysis revealed that 29.2% (7/24) of patients of group I and 25.0% (4/16) of group II were first-time pregnant, 25.0% (6/24) and 12.5% (2/16) of patients in groups I and II were primiparous, respectively (absence of statistically significant differences from the control group — 40.0% (20/50); p>0.05) (Table 2). Almost a third (20.8%; 5/24) of postpartum women of group I and 43.75% (7/16) of group II had a history of artificial abortions (in the control (III) group there were 10.0%; 5/50) and spontaneous — 12.5% (3/24) in group I and 37.5% (6/16) in group II (in group III — 8.0%) (p<0.01). The presence of abortions and miscarriages in the anamnesis was a prognostically strong unfavorable sign of the implementation of purulent-inflammatory complications: DI — 95%, 0.63 (0.54–0.72; OR>1); sensitivity — 47.4% (36–59.1), specificity — 79.6% (65.7–89.9), p=0.008.
The number of pregnancies per 1 person in groups I and II was 2.3±1.4 and 2.1±1.2, respectively, in the control group — 1.9±1.1; births 1.5±0.8 and 1.6±0.5 (group III — 1.6±0.7); artificial abortions — 1.1± 0.2 and 0.9±0.2 (group III — 0.9± 0.3); spontaneous miscarriages — 0.7± 0.5 and 0.9± 0.3 (group III — 0.3±0.6); ectopic pregnancies — 0.03±0.03 and 0.04±0.03 (group III — 0.02±0.03). There were no statistically significant differences in parity between the groups — p>0.05. Operative deliveries in the anamnesis were present in 16.7% (4/24) of patients of group I and 18.75% (3/16) of group II (in the control group, a scar on the uterus after a previous cesarean section was in 22.0% (11/50) of women).
Table 2
Postpartum women parity
|
Parity Group |
I gr. (n=24) |
II gr. (n=16) |
III gr. (n=50) |
Pearson's criterion |
||||
|
n |
% |
n |
% |
n |
% |
χ² |
p1-2 |
|
|
Number of pregnancies |
||||||||
|
1 |
7 |
29,2 |
4 |
25,0 |
20 |
40,0 |
3,813 |
>0,05 |
|
2 |
12 |
50,0 |
7 |
43,75 |
21 |
42,0 |
0,782 |
>0,05 |
|
3 and more |
5 |
20,8 |
5 |
31,25 |
9 |
18,0 |
4,177 |
>0,05 |
|
Delivery |
||||||||
|
1 |
6 |
25,0 |
2 |
12,5 |
14 |
28,0 |
6,192 |
<0,05 |
|
2 |
16 |
66,7 |
12 |
75,0 |
31 |
62,0 |
1,276 |
>0,05 |
|
3 and more |
2 |
8,3 |
2 |
12,5 |
5 |
10,0 |
0,869 |
>0,05 |
|
Caesarean section |
4 |
16,7 |
3 |
18,75 |
11 |
22,0 |
0,745 |
>0,05 |
|
Abortion |
||||||||
|
artifical |
5 |
20,8 |
7 |
43,75 |
5 |
10,0 |
23,909 |
<0,01 |
|
spontaneous |
3 |
12,5 |
6 |
37,5 |
4 |
8,0 |
26,134 |
<0,01 |
|
ectopic pregnancy |
2 |
8,3 |
1 |
6,25 |
3 |
6,0 |
0,465 |
>0,05 |
The anamnestic data of the analysis of the somatic status of the patients allowed the authors of the study to establish that the background for the development of endometritis after cesarean section surgery was often chronic extragenital pathology: anemia (37.5–43.7% in groups I–II), varicose veins of the lower extremities and pelvic organs (41.7 and 43.75%, respectively), diseases of the urinary system (33.3 and 31.3%) (p<0.01). Attention is drawn to the relatively high percentage of diseases associated with connective tissue dysplasia (myopia, mitral prolapse, etc.) (Table 3).
Table 3
Somatic diseases of postpartum women
|
Somatic disease |
I gr. (n=24) |
II gr. (n=16) |
III gr. (n=50) |
Pearson's criterion |
||||
|
n |
% |
n |
% |
n |
% |
χ² |
p1-2 |
|
|
Gastroduodenitis |
4 |
16,7 |
2 |
12,5 |
5 |
10,0 |
1,753 |
>0,05 |
|
Cholecystopancreatitis |
3 |
12,5 |
2 |
12,5 |
4 |
8,0 |
1,228 |
>0,05 |
|
Tonsillitis |
5 |
20,8 |
3 |
18,7 |
3 |
6,0 |
8,454 |
<0,05 |
|
Sinusitis |
4 |
16,7 |
2 |
12,5 |
4 |
8,0 |
3,053 |
>0,05 |
|
Bronchitis |
2 |
8,3 |
1 |
6,25 |
1 |
2,0 |
3,741 |
>0,05 |
|
Pyelonephritis |
8 |
33,3 |
5 |
31,3 |
5 |
10,0 |
13,41 |
<0,01 |
|
Myopia |
6 |
25,0 |
4 |
25,0 |
8 |
16,0 |
2,454 |
>0,05 |
|
Varicose veins |
10 |
41,7 |
7 |
43,75 |
5 |
10,0 |
22,504 |
<0,01 |
|
Mitral valves prolapse |
2 |
8,3 |
1 |
6,25 |
2 |
4,0 |
1,496 |
>0,05 |
|
Anemia |
9 |
37,5 |
7 |
43,7 |
7 |
14,0 |
15,472 |
<0,01 |
Endocrine diseases are factors that, in addition to affecting various parts of the reproductive system, can create unfavorable conditions for reparative processes. The structure of this pathology in patients of groups I and II was dominated by diseases associated with relative hyperestrogenism: endometriosis — 22.5± 2.1% (9/40), uterine fibroids — 27.5±2.1% (11/40). The dominant gynecological pathology in postpartum women with purulent-inflammatory complications after abdominal delivery were infectious diseases: ectopia of the cervix — 42.5±1.1% (17/40), chronic endometritis — 47.5±1.1% (19/40) and salpingoophoritis — 35.0±2.1% (14/40) (p<0.01) (Table 4).
Table 4
Gynecological pathology of postpartum women
|
Gynecological pathology |
I gr. (n=24) |
II gr. (n=16) |
III gr. (n=50) |
Pearson's criterion |
||||
|
n |
% |
n |
% |
n |
% |
χ² |
p1-2 |
|
|
Endocrine-dependent diseases |
||||||||
|
Endometrial polyps |
2 |
8,3 |
1 |
6,3 |
2 |
5,0 |
0,845 |
>0,05 |
|
Endometrial hyperplasia |
4 |
16,7 |
2 |
12,5 |
3 |
6,0 |
4,955 |
>0,05 |
|
Endometriosis |
5 |
20,8 |
4 |
25,0 |
9 |
18,0 |
1,167 |
>0,05 |
|
Uterine fibroids |
7 |
29,2 |
4 |
25,0 |
10 |
20,0 |
1,716 |
>0,05 |
|
Mastopathy |
3 |
12,5 |
2 |
12,5 |
6 |
12,0 |
0,013 |
>0,05 |
|
Metabolic syndrome |
13 |
54,2 |
9 |
56,3 |
10 |
20,0 |
19,093 |
<0,01 |
|
Menstrual disorders |
6 |
25,0 |
3 |
18,7 |
8 |
16,0 |
2,143 |
>0,05 |
|
Ovarian cysts |
2 |
8,3 |
1 |
6,3 |
2 |
5,0 |
0,845 |
>0,05 |
|
Diseases associated with infectious factors |
||||||||
|
Cervix ectopia |
10 |
41,7 |
7 |
43,7 |
9 |
18,0 |
11,856 |
<0,01 |
|
Chronic endometritis |
11 |
45,8 |
8 |
50,0 |
6 |
12,0 |
24,159 |
<0,01 |
|
Chronic salpingooophoritis |
8 |
33,3 |
6 |
37,5 |
5 |
10,0 |
16,299 |
<0,01 |
Metabolic syndrome, which may be one of the frequent causes of difficulties in operative delivery, changes in uterine contractile activity, immune status and interfere with the normal healing of the surgical wound, was 1.75 times more common in patients with a complicated course of postoperative puerperium: 55.0±1.1% (22/40) in groups I and II versus 20.0% (10/50) in еру control group (p<0.01) (Table 4, Figures 4–6). The median body mass index (BMI) of all the examined postpartum women was 26.2±3.4 (CI — 95%, 19.0–36.0; p=0.005). The average BMI in group I was 27.0±2.7 (CI – 95%, 21.0–34.0; p=0.005), in II — 29.8±2.3 (CI — 95%, 22.0–36.0; p=0.005) (in the control group, the BMI was 25.1±3.1) (Figures 4–5).
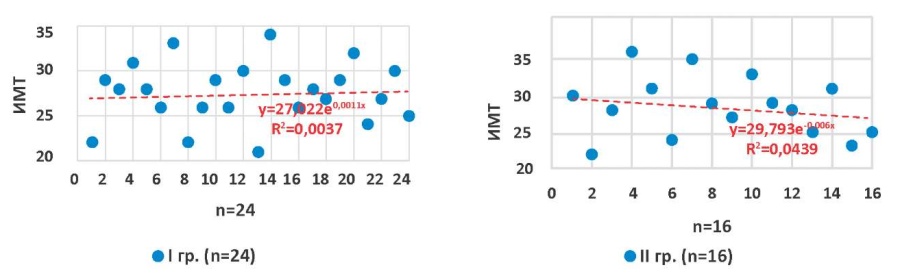
Figure 4. Body mass index in groups with complications after cesarean section

Figure 5. Body mass index in group with normal course of puerperia (control)
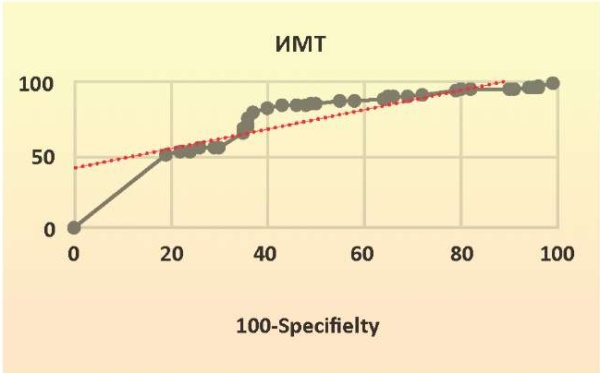
Figure 6. ROC curve (dotted 95%CI AUC) — prognostic sensitivity and selectivity of postpartum women BMI analyzing
Among sexually transmitted infections in patients with complicated puerperium after operative delivery (groups I–II), the most common were nonspecific vulvovaginitis — 70.0±4.8% (28/40) (p<0.01), vulvovaginal candidiasis — 75.0±5.2% (30/40) (p<0.01), herpetic — 25.0±3.4% (10/40) (p<0.01), papillomavirus — 15.0±2.1% (6/40), chlamydia and mycoplasma infections — 15.0±2.0% (6/40) each (Table 5).
Table 5
Prevalence of sexually transmitted infections of postpartum women
|
Genital infections |
I gr. (n=24) |
II gr. (n=16) |
III gr. (n=50) |
Pearson's criterion |
||||
|
n |
% |
n |
% |
n |
% |
χ² |
p1-2 |
|
|
Trichomoniasis |
2 |
8,3 |
1 |
6,25 |
1 |
2,0 |
3,741 |
>0,05 |
|
Gonorrhea |
1 |
4,2 |
- |
- |
- |
- |
- |
- |
|
Chlamydial, mycoplasma infections |
4 |
16,7 |
2 |
12,5 |
4 |
8,0 |
3,053 |
>0,05 |
|
HPV |
5 |
20,8 |
4 |
25,0 |
9 |
18,0 |
1,167 |
>0,05 |
|
Genital HSV |
5 |
20,8 |
5 |
31,3 |
4 |
8,0 |
13,595 |
<0,01 |
|
Vulvovaginal candidiasis |
17 |
70,8 |
13 |
81,2 |
14 |
28,0 |
26,502 |
<0,01 |
|
Nonspecific vulvovaginitis |
16 |
66,7 |
12 |
75,0 |
9 |
22,0 |
29,98 |
<0,01 |
Thus, in patients with advanced endometritis and uterine suture failure after abdominal delivery, the frequency of concomitant gynecological (inflammatory and hormonal) and extragenital pathology (СI – 95%, 0.77 (0.68–0.84)) was higher than in the population and control group; sensitivity was 57.7% (46.0–68.8), specificity — 89.8% (77.8–96.6); p=0.018), which predisposes to violations of involution, changes in reparative processes in the tissues of the operated uterus, the realization of chronic persistent foci of infection and serves as predisposing factors for the development of purulent-septic processes in the postpartum period.
The analysis of the course of the present pregnancy revealed that in 66.7% (16/24) of patients of group I and 56.25% (9/16) of group II, it proceeded against the threat of termination at various times. The most common pathology of gestation was anemia of mild to moderate degree (72.9±2.1% (29/40)) and gestational diabetes mellitus (30.0±1.1% (12/40)) in total, in groups I and II (p<0.01) (Table 6). The exacerbation of extragenital pathology in the form of exacerbation of chronic diseases of the genitourinary system (cystitis and pyelonephritis) was noted in 37.5% (9/24) of pregnant women of group I and 43.8% (7/16) of group II (p<0.01).
Table 6
Pregnancy complications
|
Complications of gestation |
I gr. (n=24) |
II gr. (n=16) |
III gr. (n=50) |
Pearson's criterion |
||||
|
n |
% |
n |
% |
n |
% |
χ² |
p1-2 |
|
|
Early toxicosis |
3 |
12,5 |
3 |
18,7 |
5 |
10,0 |
2,922 |
>0,05 |
|
Threat of spontaneous abortion |
11 |
45,8 |
7 |
43,8 |
6 |
12,0 |
21,235 |
<0,01 |
|
Threat of preterm birth |
8 |
33,3 |
5 |
31,3 |
7 |
14,0 |
8,598 |
<0,05 |
|
Anemia |
17 |
70,8 |
12 |
75,0 |
19 |
38,0 |
13,397 |
<0,01 |
|
Preeclampsia |
3 |
12,5 |
2 |
12,5 |
4 |
8,0 |
1,228 |
>0,05 |
|
Placental insufficiency |
6 |
25,0 |
5 |
31,3 |
8 |
16,0 |
4,907 |
>0,05 |
|
Gestational diabetes mellitus |
7 |
29,2 |
5 |
31,3 |
6 |
12,0 |
9,278 |
<0,05 |
|
Cystitis and pyelonephritis |
9 |
37,5 |
7 |
43,8 |
6 |
12,0 |
18,233 |
<0,01 |
Therefore, 41.7% (10/24) of women of group I and 43.75% (7/16) of group II reported acute respiratory viral infections during pregnancy, and 8.3% (2/24) and 12.5% (2/16) of herpes infections, respectively, were aggravated (in the control group, viral respiratory infections were noted in 12.0%, and exacerbation of herpes infection in 8.0% of postpartum women). Laboratory-confirmed inflammatory diseases of the reproductive tract in the form of vulvovaginitis and cervicitis were diagnosed in 20/24 (83.3%) pregnant women of group I and 15/16 (93.75%) of group II, vaginal sanitation was performed in 17/24 (70.8%) and 11/16 (68.75%) women of these groups (in the comparison group, vulvovaginitis and cervicitis occurred in 22.0% of patients) (p<0.05).
Bacterioscopy of vaginal smears showed differences in the leukocyte response of vaginal contents in groups I–II compared with the control group (14.15±2.95% vs. 9.8±1.2%), the content of coccoid microflora (29.4±1.6% vs. 15.6± 0.7%; p<0.01), in other parameters there were no differences between patients with a complicated course of the postoperative period and the control group (Table 7).
Table 7
Bacterioscopic picture of vaginal smears (M±s)
|
Indicators |
I gr. (n=24) |
II gr. (n=16) |
III gr. (n=50) |
p1-2 |
|||
|
M |
s |
M |
s |
M |
s |
||
|
Leukocytes |
13,4 |
2,7 |
14,9 |
3,2 |
9,8 |
1,2 |
>0,05 |
|
Epithelial cells |
14,1 |
2,2 |
14,6 |
3,9 |
10,3 |
1,7 |
>0,05 |
|
Fungi cells |
28,6 |
3,4 |
30,1 |
4,1 |
30,0 |
0,9 |
>0,05 |
|
«Key cells» |
4,8 |
0,6 |
5,3 |
0,9 |
4,7 |
0,4 |
>0,05 |
|
Trichomonas |
- |
- |
- |
- |
- |
- |
|
|
Diplococci |
- |
- |
- |
- |
- |
- |
|
|
Microflora nature |
|||||||
|
Rod |
4,8 |
0,7 |
4,6 |
0,5 |
18,7 |
0,7 |
<0,01 |
|
Coccal |
28,5 |
1,4 |
30,3 |
1,8 |
15,6 |
0,6 |
<0,01 |
|
Mixed |
66,7 |
1,5 |
65,1 |
2,0 |
65,5 |
1,1 |
>0,05 |
Bacteriological analysis of the microbial “picture” showed the prevalence of aerobic-anaerobic microbial associations, and isolated flora more often included associations of microaerophilic, facultative, and obligate anaerobic groups (Table 8).
Table 8
Microbial «landscape»
|
Microflora |
I gr. (n=24) |
II gr. (n=16) |
III gr. (n=50) |
Pearson's criterion |
||||
|
n |
% |
n |
% |
n |
% |
χ² |
p1-2 |
|
|
Staphylococcus aureus |
2 |
8,3 |
2 |
12,5 |
1 |
2,0 |
7,349 |
<0,05 |
|
Staphylococcus epidermidis |
8 |
33,3 |
6 |
37,5 |
4 |
8,0 |
19,388 |
<0,01 |
|
Staphylococcus haemolyticus |
2 |
8,3 |
2 |
12,5 |
1 |
2,0 |
||
|
Enterococcus faecalis |
7 |
29,2 |
5 |
31,25 |
3 |
6,0 |
17,758 |
<0,01 |
|
Streptococcus agalactia |
3 |
12,5 |
3 |
18,75 |
2 |
4,0 |
9,329 |
<0,01 |
|
Streptococcus faecium |
2 |
8,3 |
1 |
6,25 |
- |
- |
||
|
Escherichia coli |
9 |
37,5 |
7 |
43,75 |
6 |
12,0 |
18,204 |
<0,01 |
|
Proteus mirabilis |
1 |
4,2 |
1 |
6,25 |
- |
- |
||
|
Enterobacter spp. |
6 |
25,0 |
3 |
18,75 |
3 |
6,0 |
||
|
Pseudomonas aeruginosa |
- |
- |
1 |
6,25 |
- |
- |
||
|
Bacteroides spp. |
3 |
12,5 |
2 |
12,5 |
4 |
8,0 |
||
|
Peptostreptococcus / Peptococcus spp. |
4 |
16,7 |
4 |
25,0 |
- |
- |
||
|
Propionibacterium spp. |
1 |
4,2 |
- |
- |
7 |
14,0 |
||
|
Fusobacteium spp. |
1 |
4,2 |
- |
- |
4 |
8,0 |
||
|
Candida spp. |
13 |
54,2 |
10 |
62,5 |
16 |
32,0 |
10,034 |
<0,01 |
|
Lactobacillus spp. |
11 |
45,8 |
5 |
31,25 |
36 |
72,0 |
17,168 |
<0,01 |
|
Lack of microflora growth |
3 |
12,5 |
1 |
6,25 |
14 |
28,0 |
||
|
% capacity sowing |
87,5 |
93,75 |
72,0 |
|||||
Microorganisms in the form of aerobic-anaerobic associations in patients with complicated postpartum endometritis and uterine suture failure (groups I–II) were significantly (p<0.01) more common than in women with physiologically occurring postoperative puerperium (group III) (22.4±1.6% vs. 10.0%). In monoculture, facultative anaerobes were isolated in 5/24 (20.8%) of group I and 3/16 (12.5%) of group II, and obligate anaerobes — in 2/24 (8.3%) of group I and 2/16 (12.5%) of group II. Facultative anaerobes of groups I–II were most often represented by Staphylococcus (22/40; 55.0%), Streptococcus (9/40; 22.5%), and Enterococcus (12/40; 30.0%), in addition, Enterobacteria Escherichia coli — 40.0% (16/40), Enterobacter spp. — 22.5% (9/40) were often sown. There were no differences between the main and control groups among obligate non–clostridial anaerobes (Bacteroides spp., Fusobacterium spp., Peptostreptococcus spp., Peptococcus spp.), while in groups I–II there was a decrease in the proportion of gram-positive rods (Eubacterium spp., Propionibacterium spp. and especially Lactobacillus spp.). Peptostreptococcus spp. and Peptococcus spp. occupy a special place among the pathogens involved in the implementation of postpartum purulent-septic complications, which were isolated from the birth canal of patients of groups I–II in 20.0% (8/40), and did not occur in the control group. There was no growth of pathogenic microflora in 16.7% of patients of group I and 18.75% of group II. Thus, during the analysis of the microbiota of the birth canal, the polymicrobial etiology of endometritis after cesarean section was established, where the leading place belongs to conditionally pathogenic microorganisms: enterococci, enterobacteria (Enterococcus faecalis and Proteus mirabilis) and non-spore-forming anaerobes (Peptostreptococcus spp. and Bacteroides spp.).
The gestation period at the time of delivery of pregnant and parturient women of group I averaged 37.8±3.3 weeks (CI — 95%, 26.4–41.3; p=0.005), at the gestation period of 26.0–36.6 weeks, 20.8% (5/24) of patients were surgically delivered, over 41.1 weeks — 8.3% (2/24). In group II, the median term of delivery was 37.4±3.4 weeks (CI — 95%, 26.2–41.1; p=0.005), at the gestation period of 26.2–36.6 weeks, cesarean section was performed by 18.75% (3/16) of women in labor, over 41.1 weeks — 6.25% (1/16).
Cesarean section was performed in groups with complicated puerperium, most often for emergency and urgent indications (72.5±2.3% (29/40)), in the control group, emergency indications were 1.4 times less (52.0% (26/50)), most operations in groups I and II were performed intranatally (57.5±2.1% (23/40)). The most frequent indications for abdominal delivery in groups I and II were a scar on the uterus after operations on it (30.0±3.1% (12/40)), fetal distress (17.5±1.1% (7/40)) and uterine contractile abnormalities (20.0±5.1% (8/40)) (Table 9). At the same time, a statistically significant difference between the two main and control groups was revealed with such indications for cesarean section as a clinically narrow pelvis (χ²=6.546; p<0.05) and labor anomalies (χ²=8.16; p<0.05).
Table 9
Evidence for abdominal delivery
|
Positions |
I gr. (n=24) |
II gr. (n=16) |
III gr. (n=50) |
Pearson's criterion |
||||
|
n |
% |
n |
% |
n |
% |
χ² |
p1-2 |
|
|
Placenta previa |
1 |
4,2 |
1 |
6,25 |
3 |
6,0 |
||
|
Placenta premature abruption |
2 |
8,3 |
1 |
6,25 |
2 |
4,0 |
1,496 |
>0,05 |
|
Fetus incorrect position and presentation |
2 |
8,3 |
- |
- |
4 |
8,0 |
||
|
Prolonged or post-term pregnancy |
2 |
8,3 |
- |
- |
3 |
6,0 |
||
|
Anatomical obstructions in childbirth |
4 |
16,7 |
3 |
18,7 |
3 |
6,0 |
6,546 |
<0,05 |
|
Uterus scar |
7 |
29,2 |
5 |
31,3 |
11 |
22,0 |
1,030 |
>0,05 |
|
Preeclampsia |
2 |
8,3 |
2 |
12,5 |
4 |
8,0 |
1,319 |
>0,05 |
|
Fetal distress |
4 |
16,7 |
3 |
18,7 |
7 |
14,0 |
2,655 |
>0,05 |
|
Labor activity anomalies |
4 |
16,7 |
4 |
25,0 |
5 |
10,0 |
8,160 |
<0,05 |
|
Somatic pathology that excludes attempts |
1 |
4,2 |
- |
- |
4 |
8,0 |
||
Therefore, 20.8% (5/24) of patients of group I and 18.75% (3/16) of group II were delivered with an entire fetal bladder. The median anhydrous period was 8.1±182 hours (CI — 95%, 0–364; p=0.005) in group I and 10.4±125 hours (CI — 95%, 0–251; p=0.005) in group II. An anhydrous period of more than 12 hours before cesarean section was recorded in 25.0% (6/24) of women of group I and 31.25% (5/16) of group II.
Among the technical features of abdominal delivery, Pfannenstiel laparotomy was performed most often in groups I and II (65.0±1.1% (26/40)) with a horizontal incision in the lower segment of the uterus (82.5±6.25% (33/40)) and suturing of the uterus with a single-row synthetic suture (62.5±0.1% (25/40)). In most cases, prolonged antibiotic prophylaxis was carried out (82.5±1.1% (33/40)) (Table 10). Information about technical difficulties in removing the adjacent part of the fetus, accompanied by traumatization of the uterus (ruptures of the lower segment, ruptures passing to the uterine rib) was noted in 3/40 cases (7.5%). Besides, 6/40 (15%) operations were accompanied by pathological blood loss (1000 ml or more): in women, the ascending branches of a. uterinae were ligated, in 2/40 (5.0%), compression hemostatic sutures were applied to the uterus (according to B-Linch or Pereyr).
The average surgery duration in groups I and II was 38.1±7.4 minutes, in 27.5±2.1% (11/40) of cases, the surgery duration was more than 60 minutes (in the control group, the average duration of the operation was 34.4±6.8 minutes). The average intraoperative blood loss in the main groups was 578±134 ml (6.9±3.1 ml/kg body weight), in the control group — 549±75 ml (7.5±2.8 ml/kg body weight).
Table 10
Technical features of the cesarean section
|
Features |
I gr. (n=24) |
II gr. (n=16) |
III gr. (n=50) |
Pearson's criterion |
||||
|
n |
% |
n |
% |
n |
% |
χ² |
p1-2 |
|
|
Laparotomy Pfannenstiel |
16 |
66,7 |
11 |
68,8 |
20 |
40,0 |
8,799 |
<0,05 |
|
Laparotomy Joel-Cohen |
6 |
25,0 |
3 |
18,7 |
26 |
52,0 |
19,566 |
<0,01 |
|
Lower median laparotomy |
2 |
8,3 |
2 |
12,5 |
4 |
8,0 |
1,319 |
>0,05 |
|
Uterus transverse incision |
21 |
87,5 |
12 |
75,0 |
44 |
88,0 |
1,300 |
>0,05 |
|
Uterus isthmic-corporal incision |
3 |
12,5 |
3 |
18,7 |
4 |
8,0 |
4,457 |
>0,05 |
|
Uterus corporal incision |
- |
- |
1 |
6,25 |
2 |
4,0 |
||
|
Bottom caesarean section |
- |
- |
- |
- |
- |
- |
||
|
Uterus exteriorization |
19 |
79,2 |
11 |
68,8 |
36 |
72,0 |
0,780 |
>0,05 |
|
Single-row synthetic suture on the uterus |
15 |
62,5 |
10 |
62,5 |
28 |
56,0 |
0,467 |
>0,05 |
|
Two-row synthetic suture on the uterus |
9 |
37,5 |
6 |
37,5 |
22 |
44,0 |
0,711 |
>0,05 |
|
Catgut suture on the uterus |
- |
- |
- |
- |
- |
- |
||
|
Abdominal drainage |
2 |
8,3 |
2 |
12,5 |
3 |
6,0 |
||
|
Ligation of ascending branches a. uterinae |
3 |
12,5 |
3 |
18,7 |
4 |
8,0 |
4,457 |
>0,05 |
|
Compression sutures on the uterus |
1 |
4,2 |
1 |
6,25 |
1 |
2,0 |
||
|
Intraoperative antibiotic prophylaxis |
4 |
16,7 |
3 |
18,7 |
17 |
34,0 |
7,718 |
<0,05 |
|
Prolonged antibiotic prophylaxis |
20 |
83,3 |
13 |
81,3 |
33 |
66,0 |
2,325 |
>0,05 |
The average score of newborns on the Apgar scale at the 5th minute of delivery in the main groups was 7.8±1.2 points. The presence of perinatal losses was noted in patients of groups I and II (12.5%; 5/40): two had antenatal fetal death (detachment of the normally located placenta) and three newborns (all premature less than 34 weeks) died before the 8th day of the neonatal period.
The Spearman rank correlation analysis established predictors that disrupt the process of scar repair on the uterus after cesarean section and contribute to the implementation of purulent-septic complications (outcome, dependent binary sign: yes/no). According to the results of logistic regression, they can be divided into 4 groups (p<0.05): factors related to the technique of suturing (the technique of suturing the uterine wall and suture materials used, exteriorization of the uterus for suturing); related to changes in the lower segment of the uterus (gestation period, period of delivery, level of incision of the uterus); factors possibly related to scar healing (maternal: age, BMI, parity, number of cesarean sections, extragenital pathology; fetal: newborn weight, number of fetuses; intraoperative: method of anesthesia, duration of surgery, blood loss); genetic — related to connective tissue dysplasia and tissue repair ability. Ten parameters presented in Table 11 were determined to be prognostically strong, and ROC analysis with the construction of the ROC curve and the analysis of the area under the curve (AUC) allowed determining the sensitivity and specificity for these predictors.
Table 11
ROC-analysis results of predictors of purulent-inflammatory complications
|
Indicators |
AUG (CI95%) |
p-level |
Sensitivity (CI) % |
Specificity (CI) % |
|
Age ≥35 years |
0,62 (0,53–0,71) |
0,014 |
50,0 (38,5–61,5) |
73,5 (58,9–85,1) |
|
Anamnesis abortion |
0,63 (0,54–0,72) |
0,008 |
47,4 (36,0–59,1) |
74,9 (60,7–89,1) |
|
Chronic extragenital and genital infection |
0,67 (0,56–0,76) |
0,003 |
62,7 (49,1–75,0) |
77,4 (58,9–90,4) |
|
Body mass index ≥30 |
0,70 (0,51–0,89) |
0,016 |
61,3 (47,9–74,7) |
78,4 (64,5–92,3) |
|
Vaginal dysbiosis |
0,77 (0,68–0,84) |
<0,0001 |
57,7 (46,0–68,8) |
89,8 (77,8–96,6) |
|
Waterless period ≥12 hours |
0,71 (0,65–0,76) |
<0,0001 |
56,7 (49,1–64,1) |
96,3 (94,0–98,6) |
|
Delivery at gestation earlier than 34 and later 42 weeks |
0,62 (0,51–0,72) |
0,018 |
77,1 (60,0–90,0) |
56,4 (42,2–70,5) |
|
Delivery close to the beginning of the II period of labor |
0,76 (0,64–0,88) |
<0,0001 |
61,6 (49,3–73,9) |
87,7 (78,2–97,1) |
|
Intraoperative blood loss ≥1000 ml |
0,73 (0,60–0,85) |
<0,0001 |
64,7 (51,1–78,3) |
85,3 (74,7–95,9) |
|
CS duration ≥60 minutes |
0,65 (0,51–0,80) |
0,016 |
56,9 (44,5–69,3) |
81,1 (68,9–93,3) |
Based on the systematization of anamnestic and clinical data of maternity hospitals with endometritis and uterine suture failure after abdominal delivery, the main risk factors for the development of purulent-inflammatory complications were grouped and a diagnostic table was developed (Table 12).
Table 12
Prognostic criteria for the risk of developing purulent-septic complications after cesarean section
|
№№ |
Symptom |
Abnormal puerperium (DU) |
Complicated puerperium (DU) |
DC |
|
Anamnestic signs |
||||
|
1 |
Age (years) |
|||
|
18–25 |
0,65 |
0,21 |
-3,1 |
|
|
25–30 |
0,52 |
0,45 |
-1,6 |
|
|
30–35 |
0,20 |
0,63 |
+3,2 |
|
|
>35 |
0,13 |
0,99 |
+7,6 |
|
|
2 |
Chronic somatic and gynecological pathology |
|||
|
Extragenital infection |
0,12 |
0,71 |
+5,9 |
|
|
Gynecological pathology |
0,18 |
0,65 |
+3,6 |
|
|
Metabolic syndrome |
0,10 |
0,76 |
+7,6 |
|
|
Connective tissue dysplasia |
0,21 |
0,69 |
+3,3 |
|
|
3 |
The course of a real pregnancy |
|||
|
Threat of abortion |
0,31 |
0,69 |
+3,4 |
|
|
Gestational diabetes mellitus |
0,13 |
0,90 |
+8,9 |
|
|
Anemia |
0,18 |
0,92 |
+9,1 |
|
|
Preeclampsia |
0,12 |
0,55 |
+4,3 |
|
|
Vaginal infections |
0,14 |
0,86 |
+8,6 |
|
|
Acute respiratory infections |
0,16 |
0,77 |
+4,8 |
|
|
Vaginal smear inflammatory nature |
0,20 |
0,84 |
+4,2 |
|
|
Abundant (>104) growth of pathogenic and/or conditionally pathogenic microflora |
0,11 |
0,89 |
+8,1 |
|
|
4 |
Number of pregnancies |
|||
|
Abortions (artifical, spontaneous) |
0,09 |
0,67 |
+6,3 |
|
|
1 births |
0,61 |
0,14 |
-1,2 |
|
|
2 births |
0,25 |
0,53 |
-0,9 |
|
|
3 births |
0,19 |
0,61 |
+4,6 |
|
|
5 |
Gestational delivery period (weeks) |
|||
|
22–28 |
0,21 |
0,52 |
+5,8 |
|
|
29–37 |
0,24 |
0,46 |
+2,5 |
|
|
≥37 |
0,46 |
0,22 |
-1,8 |
|
|
6 |
Caesarean section |
|||
|
Antenatally |
0,26 |
0,32 |
+1,4 |
|
|
Intranatally |
0,33 |
0,25 |
-0,9 |
|
|
Scheduled |
0,78 |
0,13 |
-2,2 |
|
|
Emergency |
0,21 |
0,56 |
+2,4 |
|
|
7 |
Indications for caesarean section |
|||
|
Labor activity anomalies |
0,13 |
0,79 |
+6,0 |
|
|
Clinically narrow pelvis |
0,11 |
0,81 |
+6,3 |
|
|
Preeclampsia |
0,28 |
0,71 |
+4,2 |
|
|
Placenta previa |
0,27 |
0,56 |
+3,1 |
|
|
Placental premature abruption |
0,18 |
0,29 |
+1,6 |
|
|
Fetal distress |
0,20 |
0,24 |
+1,2 |
|
|
Multiple pregnancies |
0,21 |
0,72 |
+4,3 |
|
|
Uterus scar |
0,26 |
0,85 |
+4,8 |
|
|
8 |
Anhydrous interval before delivery |
|||
|
Up to 12 hours |
0,48 |
0,34 |
-1,2 |
|
|
Over 12 hours |
0,19 |
0,88 |
+7,6 |
|
|
9 |
Cesarean section-technique and features |
|||
|
Laparotomy |
||||
|
Pfannenstiel |
0,32 |
0,48 |
+0,8 |
|
|
Joel-Cohen |
0,82 |
0,13 |
-2,5 |
|
|
Lower median |
0,14 |
0,42 |
+3,0 |
|
|
Uterus incision |
||||
|
Transverse |
0,76 |
0,14 |
-5,4 |
|
|
Isthmic-corporal |
0,19 |
0,54 |
+2,2 |
|
|
Corporal |
0,16 |
0,78 |
+4,9 |
|
|
Suturing a postoperative wound on the uterus method |
||||
|
Polyglycolid (vicryl) single row |
0,51 |
0,42 |
-0,8 |
|
|
Polyglycolide (vicryl) two row |
0,64 |
0,32 |
-2,0 |
|
|
Intraoperative blood loss |
||||
|
≤1000 ml |
0,54 |
0,22 |
-1,4 |
|
|
≥1000 ml |
0,13 |
0,65 |
+5,0 |
|
|
≥1500 ml |
0,10 |
0,84 |
+8,4 |
|
|
Duration of the operation |
||||
|
≤60 min |
0,77 |
0,23 |
-3,3 |
|
|
≥60 min |
0,16 |
0,91 |
+5,7 |
|
The analysis made it possible to identify the most informative indicators for assessing the prognosis of the development of purulent-inflammatory complications after abdominal delivery. DC up to +16 bits with a high probability suggested the normal development of the postoperative period, with DC +17 bits or more, the probability of postoperative endometritis was 75%. The calculation of DC allows assessing the risk of postoperative purulent-septic complications with a high degree of probability and developing measures for their prevention. The sensitivity of the forecast was 76.9%, specificity — 95.1% (accuracy — 86.0%).
Discussion
Therefore, prognosis and prevention of purulent-septic diseases in the postpartum period (and especially in the postoperative period) is one of the most urgent and still unresolved problems in obstetrics [1][3][12][14][15]. Nowadays, many risk factors for postpartum infectious complications have been established and their number continues to increase, while there are no unified objective methods for predicting postpartum endometritis and uniform criteria for assessing the degree of infectious risk [1][4][12][14]. In this study, the main clinical and anamnestic predictors of the risk of infectious complications after cesarean section surgery were identified. With the help of mathematical modeling methods, a scale for predicting the risk of purulent-inflammatory complications in early puerperium after abdominal parturition has been developed.
Conclusion
Thus, the prognostic mathematical clinical and anamnestic scale for assessing the risk of purulent-inflammatory complications in maternity patients after abdominal delivery allows identifying the main predictors of infectious diseases in patients after cesarean section, which contributes to their timely prevention and thereby reducing the frequency of severe forms of postpartum infection.
An application has been submitted for registration of the software “Scale for assessing the risk of purulent-inflammatory complications in maternity patients after abdominal delivery”.
Authors’ contribution:
Irina I. Kutsenko — research of the concept and design development (formation of the idea; formulation and development of key goals and objectives), conducting research (analysis and interpretation of the data obtained), approval of the final version of the article (taking responsibility for all aspects of the work, the integrity of all parts of the article and its final version);
Igor O. Borovikov — development of the concept and design of the study, obtaining and analyzing data, reviewing publications on the topic of the article, writing the text of the manuscript final approval of the version for publication;
Marina V. Galustyan — data acquisition and analysis, visualization (preparation, creation of published work in terms of visualization and display of data), statistical analysis, resource support of the study;
Anton S. Magay — review of publications on the topic of the article, statistical analysis;
Olga I. Borovikova — data acquisition and analysis, visualization, statistical analysis.
Conflict of interest. Authors declares no conflict of interest.
1. Maternal mortality in the Russian Federation in 2018 (methodical letter) / edited by E.N. Baibarina. M. 2019:73.
References
1. Savelyeva G.M., Sukhikh G.T., Serov V.N., Radzinsky V.E., eds. Obstetrics: national leadership. Moscow: GEOTAR-Media; 2018. (In Russ.).
2. Bonet M, Souza JP, Abalos E, Fawole B, Knight M, et al. The global maternal sepsis study and awareness campaign (GLOSS): study protocol. Reprod Health. 2018;15(1):16. https://doi.org/10.1186/s12978-017-0437-8
3. Menacker F, Hamilton BE. Recent trends in cesarean delivery in the United States. NCHS Data Brief. 2010;(35):1-8. PMID: 20334736.
4. Chou D, Tunçalp Ö, Firoz T, Barreix M, Filippi V, et al. Constructing maternal morbidity - towards a standard tool to measure and monitor maternal health beyond mortality. BMC Pregnancy Childbirth. 2016;16:45. https://doi.org/10.1186/s12884-015-0789-4
5. McCauley M, White S, Bar-Zeev S, Godia P, Mittal P, et al. Physical morbidity and psychological and social comorbidities at five stages during pregnancy and after childbirth: a multicountry cross-sectional survey. BMJ Open. 2022;12(4):e050287. https://doi.org/10.1136/bmjopen-2021-050287
6. Say L, Barreix M, Chou D, Tunçalp Ö, Cottler S, et al. Maternal morbidity measurement tool pilot: study protocol. Reprod Health. 2016;13(1):69. https://doi.org/10.1186/s12978-016-0164-6
7. Rodgers SK, Kirby CL, Smith RJ, Horrow MM. Imaging after cesarean delivery: acute and chronic complications. Radiographics. 2012;32(6):1693-712. https://doi.org/10.1148/rg.326125516
8. Heitkamp A, Meulenbroek A, van Roosmalen J, Gebhardt S, Vollmer L, et al. Maternal mortality: near-miss events in middle-income countries, a systematic review. Bull World Health Organ. 2021;99(10):693-707F. https://doi.org/10.2471/BLT.21.285945
9. Krasnopol'skiĭ VI, Buianova SN, Shchukina NA. Pyoseptic complications in obstetrics and gynecology: the specific features of their course at the present stage. Management tactics. Russian Bulletin of Obstetrician-Gynecologist. 2013;13(4):82‑85. (In Russ.).
10. Galustyan M.V., Kutsenko I.I., Borovikov I.O., Magay A.S. Opportunities for predicting cesarean scar insufficiency. Medical Herald of the South of Russia. 2021;12(1):54-61. https://doi.org/10.21886/2219-8075-2021-12-1-54-61
11. Mulic-Lutvica A, Axelsson O. Postpartum ultrasound in women with postpartum endometritis, after cesarean section and after manual evacuation of the placenta. Acta Obstet Gynecol Scand. 2007;86(2):210-7. https://doi.org/10.1080/00016340601124086
12. Moulton LJ, Lachiewicz M, Liu X, Goje O. Endomyometritis after cesarean delivery in the era of antibiotic prophylaxis: incidence and risk factors. J Matern Fetal Neonatal Med. 2018;31(9):1214-1219. doi: 10.1080/14767058.2017.1312330
13. Tirskaya Yu.I., Barinov S.V., Dolgikh T.I. Prediction of infectious risk and a way to prevent postpartum endometritis in puerperal women of infectious risk. Obstetrics & Gynecology. 2014;(5):37-42. (In Russ.) eLIBRARY ID: 21704286
14. Mohamed-Ahmed O, Hinshaw K, Knight M. Operative vaginal delivery and post-partum infection. Best Pract Res Clin Obstet Gynaecol. 2019;56:93-106. https://doi.org/10.1016/j.bpobgyn.2018.09.005
15. Batrakova T.V., Zazerskaya I.E., Vavilova T.V. Early prognosis of postpartum endometritis. Doctor.Ru. 2021;20(1):17–20. (In Russ.) https://doi.org/10.31550/1727-2378-2021-20-1-17-20
About the Authors
I. I. KutsenkoRussian Federation
Irina I. Kutsenko - Dr. Sci. (Med.), Prof., Head of the Department of Obstetrics, Gynecology and Perinatology of the Kuban State Medical University.
Krasnodar
Competing Interests:
Authors declares no conflict of interest
I. O. Borovikov
Russian Federation
Igor O. Borovikov - Dr. Sci. (Med.), As. Prof. of the Department of Obstetrics, Gynecology and Perinatology of the Kuban State Medical University.
Krasnodar
Competing Interests:
Authors declares no conflict of interest
M. V. Galustyan
Russian Federation
Marina V. Galustyan - graduate student of the Department of Obstetrics, Gynecology and Perinatology at the Kuban State Medical University.
Krasnodar
Competing Interests:
Authors declares no conflict of interest
A. S. Magay
Russian Federation
Anton S. Magay - graduate student of the Department of Obstetrics, Gynecology and Perinatology at the Kuban State Medical University.
Krasnodar
Competing Interests:
Authors declares no conflict of interest
O. I. Borovikova
Russian Federation
Olga I. Borovikova - graduate student of the Department of Obstetrics, Gynecology and Perinatology at the Kuban State Medical University.
Krasnodar
Competing Interests:
Authors declares no conflict of interest
Review
For citations:
Kutsenko I.I., Borovikov I.O., Galustyan M.V., Magay A.S., Borovikova O.I. Possibilities of predicting purulent-inflammatory complications after cesarean section. Medical Herald of the South of Russia. 2022;13(4):73-87. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-4-73-87







































