Scroll to:
Dysfunction of the symphysis as one of the actual problems of modern obstetrics
https://doi.org/10.21886/2219-8075-2021-12-3-44-49
Abstract
Objective: To analyze the factors of the course and outcome of pregnancy in women with pubic joint dysfunction (DLS).
Materials and Methods: Th e authors performed a retrospective analysis of the course of pregnancy and the outcome of childbirth in women with pubic joint dysfunction (DLS) observed in 2016 – 2019. As a result, data on the clinical course of pregnancy and childbirth in 75 women with DLS were obtained. All women underwent routine clinical and biochemical examinations, ultrasound diagnostics (US), dopplerometry (DPM), and cardiotocography (CTG). Th e analysis of all the above parameters was carried out according to the data of birth histories for 2016-2018. Statistical processing of the obtained results was carried out using the programs Statistica 10 and Microsoft Excel 2013.
Results: Clinical manifestations, as well as changes in ultrasound data, became the main factor in deciding on the method of delivery. All patients with second-degree DLS delivered by elective Caesarean section at 39 – 40 weeks of gestation. Women with the fi rst degree of DLS had a vaginal birth. Ultrasound examination in the postpartum period did not reveal an increase in the diastasis of the pubic joint in any woman. All the postpartum women had no complications during the postpartum period.
Conclusion: DLS is a serious complication, which can lead to serious consequences in some cases in the postpartum period. It may require surgical treatment and subsequent long-term rehabilitation. For early diagnostics of DLS, it may be advisable to conduct a mandatory ultrasonic examination of the pubic joint, which is the “gold standard” for the diagnosis of this pathology, to all patients during screening ultrasonic examination.
Keywords
For citations:
Borscheva A.A., Pertseva G.M., Alekseeva N.A. Dysfunction of the symphysis as one of the actual problems of modern obstetrics. Medical Herald of the South of Russia. 2021;12(3):44-49. (In Russ.) https://doi.org/10.21886/2219-8075-2021-12-3-44-49
Introduction
Pregnancy and delivery are possible due to serious changes in a woman’s organism that occur under the effect of several hormones. From week 12, the placenta starts producing relaxin in gradually increasing concentration [1][2]. It is known that relaxin contributes to the degradation of collagen in the symphysis, and thus, symphysis diastasis, and softening of the cartilage and supporting ligaments [3][4]. Such changes in the symphysis are observed through the course of pregnancy. In women with physiological pregnancy, symphysis diastasis is insignificant and reaches 2–3 mm by the end of the 3rd trimester of pregnancy. It has an adaptive character for an increase in the pelvis diameter to facilitate vaginal delivery [4][5]. However, excessive relaxation of the symphysis leads to its instability, discomfort, and pain [6]. This condition is called symphysis pubic dysfunction (SPD). Physiologically normal pregnancy contributes to the center-of-gravity shift in a pregnant woman backward because of an increase in the lumbar lordosis, which increases the load on the pubic symphysis [5][6]. The etiology of SPD is still understudied. According to the published data, the risk factors for the development of SPD include age 25 to 40 years old, smoking, heavy physical activities during pregnancy, malposture, a significant increase in the body mass or body mass deficiency, multifetal pregnancy, rickets in the anamnesis, repeated dislocations, a pelvic asymmetry that aggravates during pregnancy, and urinary tract inflammation (UTI) [5][6][7]. Several authors pay special attention to UTI as the main factor leading to SPD because of renal losses of calcium and magnesium, which disturbs mineral metabolism in a female organism and contributes to the demineralization of bone tissue [6]. Usually, the clinical picture of SPD appears after weeks 27–30 of gestation and manifests itself as painful sensations in the area of the pubic symphysis, which enhances during movements or physical activity and decreases during rest [8][9]. A typical sign for SPD in pregnant women is “goose gait” [8][9]. Manifestations of pelvic pain in the 1st and 2nd trimesters are rare [9]. The gold standard in the diagnostic of SPD is an ultrasonic investigation (USI) in dynamics for the monitoring of the process progression and evaluation of the pain syndrome by a 10-score scale and Trendelenburg’s test [6][8]. According to the USI data, there are three stages of pubic symphysis diastasis. The first degree corresponds to the diastasis of symphysis 5–8 mm, the second stage – 8–10 mm, and the third stage – >10 mm [6][8]. The final degree of pubic symphysis diastasis (>10 mm) is a rupture of pubic symphysis [6]. Besides, SPD is diagnosed by pelvis X-ray in the frontal projection. For a more detailed examination of the pubic symphysis and ligaments, magnetic resonance imaging or computed tomography (CT) is recommended [9][10]. However, during pregnancy, these tests require significant indications. According to the published data, the expression of the pain syndrome in patients with SPD does not always correspond to the degree of diastasis because of the subjective nature of pain perception [10][11]. It was specified that the correlation was observed in the case of third-degree SPD [10]. Women with each degree of symphysis diastasis have a certain clinical picture. During the first stage of diastasis, changes in the pubic symphysis can be revealed only with an ultrasound or X-ray study because pregnant women do not have complaints yet at this stage [10][11]. Clinical manifestations of pubic symphysis diastasis of the second degree include painful sensations in the sacral and pubic areas that intensify during walking [10][11]. Third-degree pubic diastasis is complicated by the rupture of the symphysis, which leads to intense pain in the sacral and pubic areas and the impossibility of active movements in the lower limbs [10][11]. As a rule, SPD is not a life-threatening complication in pregnancy but it can lead to hemorrhagic shock and anemia in patients with associated vaginal laceration, and uterus, or pelvic diagram rupture. These complications increase the risk of an unfavorable outcome of pregnancy for the mother and the fetus [12][13]. Thus, dynamic monitoring is required for the condition of the pubic symphysis in pregnant women from the SPD risk group. Besides, it is relevant for women with primarily diagnosed changes in the pubic symphysis, because by the end of pregnancy, the degree of diastasis is the main criterion for the choice of the method of delivery. The majority of pregnant women with SPD receive conservative therapy for this condition, which includes special bandage that contributes to a reduction of the space between the pubic bones, analgesic therapy for pain syndrome management, indication of calcium, magnesium, and vitamin D-containing drugs, and physiotherapy [10][11][14][15]. In pregnant women with third-degree symphysis diastasis, strict bed confinement is recommended because of a high risk of pubic symphysis rupture and associated complications [10][14][15]. Some authors reported that continuous wearing of a bandage decreased the symphysis diastasis by 2–4 mm, which enabled a vaginal delivery. Pregnant women with SPD that did not wear bandages delivered by Cesarean section (CS) [10][11]. When conservative therapy for SPD is ineffective, pregnant women with pubic diastasis > 3–5 mm and with such complications as sacroiliac joint rupture and urologic pathology are indicated surgical treatment. It includes surgical fixation of the pubic symphysis using osteosynthesis with plates and screws [10][12][14][16]. To exclude the risk of repeated bones dislocation and osteosynthesis failure, some authors recommend the removal of the damaged cartilage located between the symphysis [9][10]. There are cases of successful conservative treatment of symphysis diastasis 5-9.5 cm. However, it should be noted that such cases are single and bear a high risk of pain syndrome and residual diastasis in the future, which can provoke sclerosis in the symphysis and other functional disorders [13][16]. On the contrary, some authors strongly recommend early surgical treatment for pubic diastasis to prevent pelvic pains and functional disorders in pubic symphysis [17]. Surgical intervention is performed as a one-step surgery for urgent indications in the case of open injury of the p pubic symphysis complicated by the associated injury of the vagina, uterus, or vast hematomas in the pubic symphysis area [12][14]. A decision on the choice of the method of delivery for each pregnant woman with SPD is made based on the evaluation of the associated obstetrical and extragenital risk and a degree of pubic symphysis diastasis. Vaginal delivery is recommended in women with the first degree of pubic diastasis, unexpressed pain syndrome, and lack of obstetrical contraindications [8][10][11]. CS is indicated to women with the second degree of pubic diastasis [8][10][11]. CS is also indicated to women with the third degree of diastasis even when there is no obstetrical or extragenital pathology because of a high risk of pubic symphysis rupture [8][6][10][11].
The study aimed to analyze the factors of the course and outcome of pregnancy in women with SPD and review publications on this pathology.
Materials and Methods
The authors performed a retrospective analysis of a course of pregnancy and outcome in women with SPD in 2016–2019. The analysis included the materials obtained from the maternity unit in one of the hospitals of Rostov-on-Don. The materials contained the data on pregnancy development and outcome in 75 women with SPD. All women underwent routine clinical, biochemical, and instrumental examination (ultrasound diagnostics, dopplerometry, and cardiotocography). The examinations were performed according to the Decree of the Ministry of Health of the Russian Federation dated November 1st, 2012 No. 572n “Protocol of medical help to obstetrical and gynecologic patients (excluding assisted-reproductive technologies)”. Ultrasonic and dopplerometry studies of the pelvic organs were performed for the measurement of the mass and size of the fetus, evaluation of the placental site and structure, Amniotic Fluid Index, and other standard parameters (APLIO MX, Toshiba Medical Sistem, Japan, 2015) with transvaginal and abdominal sensors at 5 and 6.5 Hz (greyscale). Patients from the studied group underwent USI of the pubic symphysis and were consulted by a traumatologist. Indications for these examinations included uncomfortable sensations in the area of the symphysis during movements and palpation and changes in the gait. There was no special preparation for USI of the pubic symphysis. The study was performed in a supine position of a patient. CT was made with medical fetal monitors for the mother and fetus (G6B Plus, 2017). The analysis of all the mentioned parameters was performed by medical histories of deliveries for 2016–2019. The studied documentation contained a signed form of informed consent for the processing of personal data. Statistical processing of the obtained results was made using the software packages Statistica 10 and Microsoft Excel 2013. The authors calculated the occurrence rate of features (%). Statistical significance in the occurrence rate of features was evaluated using Pearson’s chi-square test. The differences between the groups were considered significant at p < 0.05.
Results
The analysis of the documentation revealed the following results. During the specified period, 15,072 women performed deliveries. There were 75 pregnant (0.50%) women with SPD. In 2016, there were 10 pregnant women with SPD out of 3,773. In 2017, there were 23 (0.62%) women with SPD out of 3,737. In 2017, the number of women with SPD increased in comparison with 2016 (an increase in the number of women with SPD in comparison with 2016 was statistically significant, p = 0.022). A significant increase in the number of patients with SPD was observed also in 2018 and 2019 in comparison with 2016. In 2018, there were 20 (0.55%) delivered women with SPD out of 3,999 (p = 0.049). In 2019, there were delivered 20 women with SPD (0.56%) out of 3,563 (p = 0.046). However, in 2017–2019, the number of patients with the specified pathology remained relatively stable. In 2016, all patients (100%) with SPD had abdominal delivery. In 2017, 19 (82.61%) patients underwent CS and four patients (17.3%) had vaginal delivery. In 2018, 17 (77.27%) women underwent CS and five (22.7%) women had a vaginal delivery. In 2019, five women (25.00%) had a vaginal delivery and 15 (75.00%) women underwent CS. The specified data are presented in Table 1.
Table 1
Number of deliveries and patients with SPD delivered in 2016–2019
|
Years |
Number of deliveries |
Number of women with SPD |
Number of abdominal deliveries |
Number of vaginal deliveries |
|
2016 |
3,773 |
10 (0.27%) |
10 (100%) |
0 (0.00%) |
|
2017 |
3,737 |
23 (0.62%) |
19 (82.61%) |
4 (17.39%) |
|
2018 |
3,999 |
22 (0.55%) |
17 (77.27%) |
5 (22.73%) |
|
2019 |
3,563 |
20 (0.56%) |
15 (75.00%) |
5 (25.00%) |
The women with SPD aged 22–35 years old. There were 57 (76.00%) primiparous women and 18 (24.00%) two parous women (Fig. 1).

Fig. 1. The number of primiparous and two parous women with SPD in 2016–2019.
Extravaginal pathology in primiparous and two parous women included vegetovascular dystonia, neurocirculatory dystonia, chronic pyelonephritis, and nephroptosis. In 2 two parous women, before and after pregnancy, multiple myomatous nodules were revealed (< 2–3 cm in diameter). The growth of these nodules was not observed during pregnancy. Six (8.00%) primiparous women had cervical incompetence that was corrected with a vaginal pessary. Twelve (16.00%) women had light gestational anemia. Fourteen two parous women (18.67%) had moderate hydramnios. The weight of neonates varied from 3,000 to 4,500 g. There were 31 large children (41.33%) (Fig. 2).
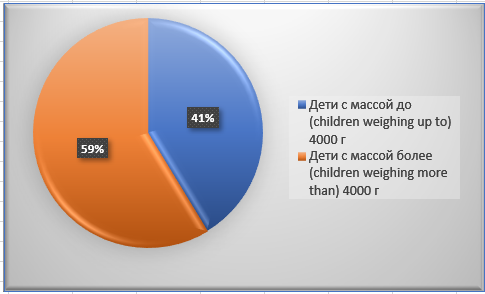
Fig. 2. The mass of children born in women with SPD in 2016– 2019.
Fourteen pregnant women (18.67%) out of 75 had first-degree SPD (diastasis 5–7 mm). These patients complained about insignificant discomfort in the pubic symphysis area during movements. In 61 (81.33%) patients, second-degree SPD was diagnosed (diastasis 11–17 mm). These pregnant women complained about discomfort and pain in the area of pubic symphysis during movements, changes in the body position, and during palpation. In the outpatient facilities (maternity welfare center), women underwent biochemical tests to evaluate the content of calcium and magnesium in the blood. There were no significant deviations from the norm. The rest women did not undergo these tests. The X-ray method is feasible in the diagnostics of SPD. However, in pregnant women, this method is used only for certain indications. The method of choice is USI. All pregnant women underwent USI of the pubic symphysis that showed also the conditions of ligaments and soft tissues. Women with first-degree SPD had diastasis without other changes. Patients with second-degree SPD had diastasis and other symptoms typical for the inflammatory process. Women with second-degree SPD received conservative therapy with Magne M6 and Calcemine. This therapy was performed from the time of SPD diagnostics to the end of pregnancy. All women with first and second-degree SPD were prescribed bandage wearing.
Clinical manifestations and changes in USI parameters were the main factors in the choice of the delivery method. All patients with second-degree SPD had planned abdominal delivery in the 39th-40th weeks of pregnancy. Women with first-degree SPD had a vaginal delivery. In the postpartum period, USI did not reveal any increase in pubic diastasis in any women. In all women, there were no complications in the postpartum period. They were discharged with children in a satisfactory condition. All patients with SPD were recommended additional examination for the identification of the cause and correction of this condition.
Discussion
The performed studies showed that SPD was not a frequent pathology during pregnancy. According to the obtained results, its prevalence rate in 2016–2019 varied from 0.27% to 0.62%. Women with SPD did not have severe extragenital or obstetrical pathology. SPD was diagnosed three times more often in primiparous women (76.0%) (p = 0.0022) than in two parous women (24.0%). When it comes to the degree of severity, second-degree SPD was revealed in 61 women (81.33%). First-degree SPD was diagnosed in 14 women (18.67%). This, the occurrence rate of second-degree SPD exceeded the occurrence rate of first-degree SPD by 4.36 times. There were no patients with a severe degree of SPD in the studied group. Since second-degree SPD is an indication for abdominal delivery, the share of women that delivered by CS was 81.33%. The timely and correct choice of the method of delivery allowed the doctors to exclude the progression of SPD. There were no complications associated with SPD in the studied women in the postpartum period.
Conclusion
The obtained data indicated an insignificant occurrence rate of SPD. On average, it was 0.50% of the total number of deliveries in 2016–2019. Still, this complication is quite serious and requires abdominal delivery in more than 80% of pregnant women with this pathology. In some cases, SPD leads to severe consequences and requires surgical correction and long-term rehabilitation. Considering this fact, it is feasible to perform USI screening of the pubic symphysis in all pregnant women. Since USI is a gold standard of SPD diagnostic, this would provide a 100% timely diagnostic at early stages of pregnancy (before the manifestation of clinical signs), timely conservative correction of this pathology (pharmacotherapy, bandage, etc.), and minimization or exclusion of severe SPD consequences. Timely diagnosis of SPD at the early stages of pregnancy and its conservative management would provide a decrease in the total rate of CS due to its decrease in the group of women with SPD.
References
1. Noskova O.V., Churilov A.V., Sviridova V.V., Litvinova E.V. Features of the course of symphysiopathy during pregnancy. Journal of Hygiene and Epidemiology. 2020;(1):64-66. (In Russ.). eLIBRARY ID: 42564613
2. Yamaguchi M, Morino S, Nishiguchi S, Fukutani N, Tashiro Y, et al. Compartion of pelvic alightment among never-pregnant women, pregnant women and postpartum women (pelvic alightment and pregnancy). Journal of Women's Health Care. 2016;5(1):1-5. DOI: 10.4172/2167-0420.1000294
3. Petrushin A.L., Pryaluchina A.V. Pubic symphysis diastasis in pregnancy and delivery (review). Traumatology and Orthopedics of Russia. 2018;24(3):145-156. (In Russ.). DOI: 10.21823/2311-2905-2018-24-3-145-156
4. Chawla JJ, Arora D, Sandhu N, Jain M, Kumari A. Pubic Symphysis Diastasis: A Case Series and Literature Review. Oman Med J. 2017;32(6):510-514. DOI: 10.5001/omj.2017.97
5. Gudushauri Ya.G., Lasarev A.F., Versin A.V. Surgical correction of the consequences of obstetric pubic symphysis ruptures. N.N. Priorov Journal of Traumatology and Orthopedics. 2014;(4):15-21. (In Russ.). eLIBRARY ID: 22951557
6. Logutova L. S., Chechneva M. A., Lysenko S. N., Cherkasova N. Yu. Ultrasound diagnostics of the state of the pubic joint in women. RMJ. 2015;23(1):42-45. (In Russ.). eLIBRARY ID: 23773001
7. Chernysheva T.V. Experience of ultrasound examination of the pubic joint in pregnant women. Ultrasound and functional diagnostics. 2015;S5:188-189. (In Russ.). eLIBRARY ID: 25655914
8. Klipfel I.V., Kalugina N.A., Emelyanova N.B. Th e possibilities of ultrasound in the diagnosis of pubic joint dysfunction. Bulletin of the Chelyabinsk Regional Clinical Hospital. 2016;1(31):64-67. (In Russ.). eLIBRARY ID: 28938765
9. Petrushin A.L., Pryalukhina A.V., Sukhanova A.I. Divergence of the pubic joint during pregnancy and childbirth. Diffi cult Patient. 2018;16(4):46-49.. (In Russ.). eLIBRARY ID: 35076887
10. Yavorskaya S.D., Plotnikov I.A., Bondarenko A.V., Olimova A.O., Plotnikova I.V. Treatment of obstetric symphysis pubic ruptures and pubic symphysis dysfunction. Obstetrics and Gynecology. 2018;(9):68-72. (In Russ.). DOI: 10.18565/aig.2018.9.68-72
11. Chawla JJ, Arora D, Sandhu N, Jain M, Kumari A. Pubic Symphysis Diastasis: A Case Series and Literature Review. Oman Med J. 2017;32(6):510-514. DOI: 10.5001/omj.2017.97
12. Buitendyk M, Brennan B, Vora P, Smith P, Winsor S. Acute Intrapartum Rupture of the Pubic Symphysis Requiring Resuscitation and Surgical Intervention: A Case Report. J Obstet Gynaecol Can. 2018;40(1):68-71. DOI: 10.1016/j.jogc.2017.05.028
13. Erickson D, Low J, Shumway J. Management of Postpartum Diastasis of the Pubic Symphysis. Orthopedics. 2016;39(2):e367-9. DOI: 10.3928/01477447-20160307-02
14. Palvia V, Kim S, Warholic H, Anasti J. Severe pubic symphysis diastasis managed conservatively: case report and review. Case Rep Clin Med. 2017;6:120-126. DOI: 10.4236/crcm.2017.64010
15. Agar N, Gremeau AS, Bonnin M, Vendittelli F. Local analgesic infi ltration and post-partum hyperalgetic symphysis pubis dysfunction. Gynecol Obstetric Case Rep. 2016;2(1):1-3
16. Tripathi SK, Kumar S, Agarwal NK, Khan A, Jain P, Nanda SN. Post-partum diastasis: a case report. Ann Int Med Dent Res. 2016;2(5):10-11.
17. Mulchandani NB, Jauregui JJ, Abraham R, Seger E, Illica E. Post-partum management of severe pubic diastasis. Clin Exp Obstet Gynecol. 2017;44(3):464-466. PMID: 29949295.
About the Authors
A. A. BorschevaRussian Federation
Alla A. Borscheva, Cand. Sci. (Med.), associate Professor, associate Professor of the Department of obstetrics and gynecology No. 1
Rostovon-on-Don
G. M. Pertseva
Russian Federation
Galina M. Pertseva, Cand. Sci. (Med.), assistant of the Department of obstetrics and gynecology No. 1
Rostovon-on-Don
N. A. Alekseeva
Russian Federation
Natalia A. Alekseeva, Cand. Sci. (Med.), Associate Professor, Associate Professor of the Department of Health Organization and Public Health No. 2
Rostovon-on-Don
Review
For citations:
Borscheva A.A., Pertseva G.M., Alekseeva N.A. Dysfunction of the symphysis as one of the actual problems of modern obstetrics. Medical Herald of the South of Russia. 2021;12(3):44-49. (In Russ.) https://doi.org/10.21886/2219-8075-2021-12-3-44-49





































