Scroll to:
A case of timely diagnosis and successful surgical correction of the left pulmonary artery sling in a newborn
https://doi.org/10.21886/2219-8075-2021-12-1-82-88
Abstract
The article describes a clinical observation of a newborn patient with a rare congenital cardiovascular disorder of the left pulmonary artery sling. There are few publications in the world’s literature on the clinical observations of the above pathology, which causes the key difficulty in diagnostics. Moreover, this case features a favorable outcome thanks to a timely diagnosis and a successful surgical correction that followed.
Keywords
For citations:
Pukhtinskaya M.G., Estrin V.V., Lebedenko A.A., Porutchikovа Yu.A., Simonovа A.V., Aleksanyants T.N. A case of timely diagnosis and successful surgical correction of the left pulmonary artery sling in a newborn. Medical Herald of the South of Russia. 2021;12(1):82-88. https://doi.org/10.21886/2219-8075-2021-12-1-82-88
Despite rare occurrence in clinical practice (1:14,000 newborns), the left pulmonary artery sling is one of the “classic” causes of respiratory insufficiency in children associated with a congenital cardiovascular pathology [1].
Anatomically, a sling is an anomaly in which the left pulmonary artery originates from the right pulmonary artery and goes between the trachea and esophagus. The form “vascular loop” compresses and deforms the rings of the trachea and sometimes the bronchus [1][2]. Often, a comorbid congenital pathology of the heart and the tracheobronchial tree is diagnosed. Thus, the main symptoms of the disease are such clinical signs of respiratory insufficiency as cyanosis, expiratory or combined dyspnea, and tachyarrhythmia. Sometimes, the disease develops symptomless. The first description of the results of the autopsy of a patient with this anomaly was made by Glaevecke and Doehle (1897) [3]. It is believed that the term “left pulmonary artery sling” has been used in clinical practice since 1958 [4].
The treatment for this congenital pathology is only surgical [5]. Without surgical correction, the disease prognosis is unfavorable [6][7][8]. The first surgical correction of the left pulmonary artery sling was performed by Willis J. Potts in 1953.
The article describes a rare clinical case of a newborn with the left pulmonary artery sling, diagnostics, and a successful surgical correction.
Female child Ch. was born on October 10, 2020 at a delivery department of the Central Municipal Hospital by a 30-year-old mother with a burdened obstetric-gynecologic anamnesis (uterine scar, candida colpitis), mixed type vegetative-vascular dystonia, first-degree obesity, and chronic nicotine addiction. The mother had 4 pregnancies (2 artificial abortions in the anamnesis) with prelabor rupture of membranes; 2 abdominal deliveries (uterine scar, large fetus) at 38 weeks and 2 days. The fetus weight was 4000 g, 7-7 score by the Apgar scale, in a condition of moderate severity associated with neurologic symptoms (decreased reaction during examination, weak crying, muscular hypotonia, hyporeflexia).
The worsening of the condition was observed within the first day after the birth. Clinical symptoms of respiratory insufficiency appeared (grunting breathing with the involvement of additional muscles, intercostal retraction, nasal flaring, mixed dyspnea to 60 per minute, a decrease in saturation to 90–91%, weakening of breathing in the lungs). Respiratory therapy started that included a facial oxygen mask О2 5 L/min. The condition of the newborn continued worsening (score 4 by the Downes scale): dyspnea more than 70/minute, the appearance of bilateral crepitate rales, which required transfer to continuous positive airway pressure via nasal cannulas (positive end-expiratory pressure +5 mm H2O; О2 – 50%).
The indicated therapy did not stabilize the condition of the child. On October 11, 2020, the child was examined by a resuscitator, got intubated, and transferred to the Department of Intensive Care at the Scientific and Research Institute of Obstetrics and Pediatrics for artificial pulmonary ventilation (APV). The child was transported in a warmed transport incubator by a critical care transport ambulance. The diagnosis at admission was perinatal hypoxia, respiratory distress syndrome, congenital pneumonia?
The condition of the child at admission was severe. The severity was associated with respiratory insufficiency and neurologic symptoms. Heart rate HR = 156 bpm, t = 36.6оС, StO2 = 92%, blood pressure BP = 60/34 mmHg. Clinically: decreased reaction to examination. Spontaneous breathing activity was decreased. Bregmatic fontanel (2.5 × 2.0 cm) was not tensed, the sagittal suture was open. Muscular hypertonia and dystonia were observed. Reflexes of oral and spinal automatism were weak. Meningeal symptoms were not revealed. The pupillary diameter was normal, D = S; reaction to light was active and consensual. Horizontal spontaneous nystagmus was observed. The skin was pale pink; perioral acrocyanosis was reduced after oxygen therapy. Pastosity of the face and eyes was registered. Visible mucosae were wet and pink. Heart tones were muffed and rhythmic. The pulse strength and volume were satisfactory. Hemodynamics was stable. The child was on APV, adapted with the apparatus. By auscultation, breathing was detected in all the lobes. Breathing was weak in the posterior-inferior sections. The rales were not heard. The abdomen was soft, not swallowed, painless at palpation. The liver was +2.0 cm from the edge of the costal arch. The spleen was not palpated. Urination was unassisted, urine was light yellow. The stool was unassisted, meconium, without pathologic matter. At admission, the child was preliminarily diagnosed with cerebral ischemia (Р91.0) and respiratory distress syndrome of the newborn (Р28.5). Taking into account the mother’s anamnesis, the congenital infection could not be excluded.
At admission, the results of laboratory and instrumental studies showed:
- Complete blood count (CBC): leucocytes – 10.5×109/L; hemoglobin – 162 g/L; erythrocytes – 4.52×1012/L; hematocrit – 47.0%; platelet – 219×109/L;
- capillary blood pH: parameters were balanced, lactatemia 2.7;
- common urine analysis – without pathology;
- blood biochemistry: hypoglycemia – 1.4 mmol/L, hypoproteinemia – 41.4 g/L, hypoalbuminemia – 28.7 g/L, bilirubinemia – 57.3 µmol/L due to indirect filtration;
- coagulogram – normal;
- chest and abdominal X-ray – moderate, bilateral increased pulmonary vascularity (Figure 1), intestinal hyper pneumatization;
- neurosonogram – signs of external hydrocephalus, ischemia, intraventricular hemorrhage (IVH) stage 1–2.
- Ultrasonography of the heart – patent foramen ovale 2.2 mm, left-to-right shunting, the systolic function of the left ventricle was preserved;
Doppler sonography of brain vessels – vascular plexus of enhanced echo-density, the structure was inconsistent, contours were uneven, vein of Galen – 4.71 cm/s; - ultrasonography of internal organs – enlarged liver, changes in the parenchyma, neurologist’s examination – cerebral ischemia, IVH 1–2.

Figure 1. Chest X-ray at admission.
Рисунок 1. Рентгенография лёгких при поступлении.
At the department of resuscitation, the child underwent combined multicomponent intensive therapy. Respiratory therapy – sequentially, stage by stage: high-frequency ventilation (HFV); HFV with iNO 5 ppm; APV with standard parameters, high-flow nasal cannulas (HFNC); spontaneous breathing through an oxygen mask.
Antibiotic therapy (initial with further change) – by the decision of a multidisciplinary team meeting, for health reasons, considering the sensitivity of the isolated microflora, clinical symptoms, and written consent of patients.
Hemostatic therapy: vicasol, dicynone. Infusiontransfusion therapy: correction of hypocoagulation – native quarantine fresh-frozen plasma B(III)Rh+; correction of anemia – washed erythrocytes B(III)Rh+; correction of hypoproteinemia, hypoalbuminemia – albumin 10%; parenteral nutrition – glucose solution 20%, 10% with components, aminoven 10%, smooth lipid 20%. Adaptation with an APV apparatus – sodium oxybate i.v./by drop infusion. Phototherapy. Inhalation therapy: ipratropium, pulmicort. Enteral tube nutrition every 3 hours with Pre-Nan infant formula.
Despite the therapy, the patient’s condition remained severe. The severity of the condition was provided by respiratory insufficiency, symptoms of bacterial infection (pale, icteric skin, expressed vascular pattern on the anterior abdominal wall) associated with diminished breathing (primary, on the right side), bilateral crepitate rales, trachea produced significant amount of liquid, mucopurulent sputum, enlargement of the liver and spleen. CBC showed anemia, neutrophil leukocytosis to 26×109/L with a shift to stab, monocytosis. A common urine test showed protein and leukocyturia. Biochemistry of the blood showed hypoprotein-hypoalbuminemia, bilirubinemia primarily due to indirect fraction, an increase in the activity of aspartate transaminase; hypocoagulation. The acid-base balance of capillary blood in the dynamics revealed hypoxemia, persistent hypercapnia, lactatemia. Procalcitonin in the blood in the dynamics varied from 0.5 to >10 µg/L; С-reactive protein was not revealed. Bacteriologically: endotracheal tube, pharynx mucosa, nose – growth of Acinetobacter baumannii 1×106 CFU/ml (polyresistance to all antibiotics); Staphylococcus haemolyticus 1×106 CFU/ml; blood – growth of Staphylococcus epidermidis.
On October 17, 2020, considering severe condition, X-ray imaging of the lungs in dynamics was made. Atelectasis of the segment of the right upper lobe was diagnosed. The bronchovascular pattern was enhanced along both pulmonary fields (Figure 2).

Figure 2. X-ray of the lungs in dynamics; atelectasis of the right upper lobe.
Рисунок 2. Рентгенография легких в динамике; ателектаз правой верхней доли.
Therapeutic-diagnostic bronchoscopy was performed, which revealed dystopia of the trachea, catarrhal-mucous endobronchitis, expressed symmetrical slit-like narrowing of the right main bronchus to 1–2 mm. X-ray control: positive dynamics – lack of visualization of atelectasis in the right upper lobe, left-right asymmetric pattern of the visceral organs (the mediastinum was off-centered to the left and closed the left lung). Subsegmental atelectasis of the upper lobe of the left lung cannot be excluded.
On October 29, 2020, the condition of the patient was severe and stable. Supportive APV by continuous mandatory ventilation at a respiratory rate of 20/min; О2 -30%. HR = 142 bpm, t = 36.6о С, StO2 = 96%, BP = 73/44 mm Hg. Clinically, weak breathing remained, bilateral dry rales, a significant amount of liquid sputum expressed from the trachea. Considering the transportability of the patient, computed tomography (CT) of the chest was performed at the Regional Clinical Hospital for Children. Fibroatelectasis of the right upper lode was diagnosed. Fibrous alterations in S10 of the lower lobe of the left lung with inflammatory alterations (Figure 3) were revealed. Obstruction of the right main bronchus 1.0 cm lower than the bifurcation was observed (Figures 4, 5). At the same time, emphysematous dilation of the lower lobe of the right lung with a moderate off-center shift of mediastinal organs to the left was observed. Examination of the pediatric surgeon: congenital anomaly of the right lung. Therapeutic bronchoscopy was recommended. Surgical treatment at the time of examination was not required.

Figure 3. CT scan; fibroatelectasis of the right upper lobe; inflammatory changes in the left lung; narrowing of the left bronchus.
Рисунок 3. Компьютерная томография; фиброателектаз правой верхней доли; воспалительные изменения в левом лёгком; сужение левого бронха.

Figure 4. CT scan; narrowing of the trachea and main bronchus on the right.
Рисунок 4. Компьютерная томография; сужение трахеи и главного бронха справа.
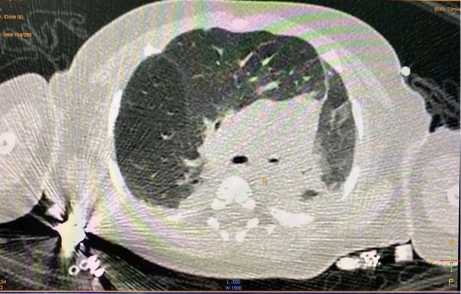
Figure 5. CT scan; narrowing of the right bronchus.
Рисунок 5. Компьютерная томография; сужение правого бронха.
On November 3, 2020, telemedical consulting of the patient was performed by cardiologists and surgeons from the State Pediatric Medical University (Saint Petersburg). The ultrasonography of the heart and vessels was recommended to exclude the vascular ring formed by aberrant veins and arteries. CT of mediastinal vessels in the vascular mode was recommended to exclude the exterior compression of the trachea and bronchus.
Positive dynamics were noted during the therapy: the patient was extubated and switched to spontaneous breathing via HFNC, later via a facial oxygen mask. Clinically: the skin was pink, mixed dyspnea 57/min, breathing with accessory muscles of respiration, moderate intercostal retraction. Lung auscultation: the breathing is heard with single rales on the left. On the right, in the projection of the upper lobe, the breathing was weak. In the projection of the middle lower lobe, every 2–3 respiratory movements, hissing breathing with a specific click was heard.
On December 3, 2020, at the cardio surgical department of the Rostov Regional Clinical Hospital, spiral CT with angiography of the chest was performed. Conclusion: a sharp narrowing of the distal section of the trachea to 2 mm (in the area of the bifurcation), narrowing of the right main bronchus to 1 mm (3.5 mm long). The left main bronchus was narrowed to 1.5 mm.
The lung artery (10.7 mm in diameter) coursed from the right ventricle. The stem was at the level of the bifurcation (12.5 mm). The right pulmonary artery was 9.7 mm. The left pulmonary artery was up to 5 mm, coursed from the right pulmonary artery, and looped over the right main bronchus and trachea constricting them.
On December 16, 2020, considering the diagnosed cardiovascular anomaly, the child was examined by a telemedical line and transported to the Saint Petersburg State Pediatric Medical University of the Ministry of Healthcare of the Russian Federation to the Intensive Care Unit for children with cardiosurgical pathology for further surgical treatment.
The primary clinical diagnosis: IDC-10: Q25.7: Congenital heart defect: Other congenital malformations of the pulmonary artery (left pulmonary artery sling), bronchi congenital defect. The complication of the primary disease: fibroatelectasis of the upper lobe of the right lung.
Comorbid diseases: early residual-organic lesion of the central nervous system, atrophic hydrocephalus syndrome, IVH stage 2, at the stage of organization, neonatal sepsis caused by other staphylococci, bilateral pneumonia, period of remission.
Discussion
On December 24, 2020, at the Saint Petersburg State Pediatric Medical University, the patients with a clinical diagnosis Q25.7 Congenital heart defect: left pulmonary artery sling; open arterial duct, compression of the right main bronchial ostium underwent successful surgery: reimplantation of the left pulmonary artery into the stem of the pulmonary artery in the condition of artificial circulation.
On January 15, 2021, the patient was discharged from the hospital in a satisfactory stable condition for a followup by a local pediatrician (Figure 6).
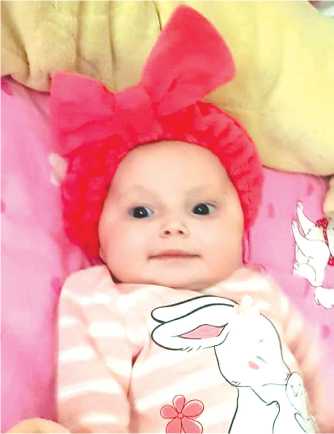
Figure 6. Patient Ch. after radical correction of the left pulmonary artery sling (photo is published with the written permission of the patient’s mother).
Рисунок 6. Пациентка Ч. после радикальной коррекции слинга левой легочной артерии (фотография публикуется с письменного разрешения матери).
The presented clinical case confirmed complicated diagnostics of the left pulmonary sling, especially, in the neonatal period. APV, severe bacterial complications, complicated or often impossible use of highly informative methods of diagnostics in the specialized conditions considering the “non-transportability” of patients, a requirement for consultations with various medical specialists, lack of “medical vigilance” and clinical experience because of the rare occurrence of the pathology determine the actual condition of the problem.
A thorough analysis of the development of the disease allowed the authors to make the following conclusions. In this case, the main signs within the symptom complex that suggested the left pulmonary artery sling included persistent weakening of breathing on the right (affected side), a significant volume of liquid mucous sputum during the observation, persistent hypercapnia, a necessity in long-term APV, atelectasis of the upper lobe of the right lung, and narrowing of the right main bronchus.
The only effective method of treatment for this congenital cardiovascular defect is the surgical correction of the pulmonary loop, which is performed “open”- hearted with artificial blood circulation. This involves the transportation and hospitalization of the patient to a cardio surgical specialized inpatient center [1][2][3][4][5][6][7][8]. It is evident that in these conditions, the success of this surgery with a favorable outcome is multifactor and ambiguous.
In this case, a favorable outcome of the correction of the left pulmonary artery sling in the patient was provided by the timely highly informative diagnostics that included fibrobronchoscopy, CT with angiography, cooperation of various specialists, telemedical counseling, careful transportation, high professionalism, and personal involvement.
Conclusion
The presented clinical case has confirmed that currently, a favorable outcome of the treatment for the left pulmonary artery sling in a newborn is possible when combined highly technological diagnostic, intensive care, and surgical help are provided. CT with vessels contrasting is the method of choice if the pulmonary artery sling is suspected.
Although this pathology is rare, neonatologists and resuscitators should have clinical vigilance for the possibility of this cardiovascular pathology. A clinical protocol for the management of a neonate with the left pulmonary artery sling should be developed and implemented.
References
1. Bazylev V.V., Chernogrivov A.E., Chernogrivov I.E. Aberrant origin of the left pulmonary artery, congenital tracheal stenosis and ring-sling complex (part I). Byulleten’ Nauchnogo Tsentra Serdechno Sosudistoy Khirurgii imeni A.N. Bakuleva RAMN (Bulletin of Bakoulev Scientific Center for Cardiovascular Surgery RAMS). 2018;19(1):14–27. (In Russ.). DOI: 10.24022/1810-0694-2018-19-1-14-27
2. Bockeria L.A., Svobodov A.A., Nikiforov V.S., Adkin D.V., Yurpol’skaya L.Yu. The case of successful correction of abnormal left pulmonary artery(sling) with an interventricular septal defect in achild aged 6 months. Detskie Bolezni Serdtsa i Sosudov (Children’s Heart and Vascular Diseases). 2010;3:68–69. (In Russ.). eLIBRARY ID: 15269318
3. Kim A.I., Akatov D.S., Makarenko V.N., Mumladze K.V., Nikiforov V.S. The case of successful correction of an abnormal departure of the leftpulmonary artery from the right pulmonary arterywith stenosis of the trachea. Detskie Bolezni Serdtsa i Sosudov (Children’s Heart and Vascular Diseases). 2012;4:68–9. (In Russ.). eLIBRARY ID: 18981625
4. Shatalov K.V., Razumovskiy A.Yu., Arnautova I.V., Turdieva N.S. Surgical correction of the left pulmonary artery sling in combination with trachealstenosis in young children. Detskie Bolezni Serdtsa i Sosudov (Children’s Heart and Vascular Diseases). 2015;2:34–8. (In Russ.). eLIBRARY ID: 25008655
5. Razumovskiy A.Yu., Afukov I.I., Kulaev A.D., Alkhasov A.B., Mitulov Z.B., Kulikova N.B., Stepanenko N.S. Sliding tracheoplasty in childrenunder conditions of extracorporeal membrane oxygenation (The first experience in Russia) (withcomments). Khirurgiya. Zhurnal imeni N.I. Pirogova (N.I. Pirogov Journal Surgery). 2015; 8: 4–13. (In Russ.). DOI: 10.17116/hirurgia201584-13
6. Giudici V, Kanani M, Muthialu N, Carr M, Calder AD, et al. Duplicated left pulmonary artery: an unknown disease? Three case reports and review of the literature. Cardiol Young. 2016;26(2):340-6. DOI: 10.1017/S1047951115000281
7. Butler CR, Speggiorin S, Rijnberg FM, Roebuck DJ, Muthialu N, et al. Outcomes of slide tracheoplasty in 101 children: a 17-year single-center experience. J Thorac Cardiovasc Surg. 2014;147(6):1783-9. DOI: 10.1016/j.jtcvs.2014.02.069
8. Speggiorin S, Torre M, Roebuck DJ, McLaren CA, Elliott MJ. A new morphologic classification of congenital tracheobronchial stenosis. Ann Thorac Surg. 2012;93(3):958-61. DOI: 10.1016/j.athoracsur.2011.12.019.
About the Authors
M. G. PukhtinskayaRussian Federation
Marina G. Pukhtinskaya, Dr. Sci. (Med.), Leading Researcher of Department of Anesthesiology and Resuscitation
Rostov-on-Don
V. V. Estrin
Russian Federation
Vladimir V. Estrin, Dr. Sci. (Med.), Professor, Head of Department of Anesthesiology and Resuscitation
Rostov-on-Don
A. A. Lebedenko
Russian Federation
Alexander A. Lebedenko, Dr. Sci. (Med.), Professor, Director (Vice-Rector)
Rostov-on-Don
Yu. A. Porutchikovа
Russian Federation
Yulia A. Porutchikova, Chief Medical Officer
Rostov-on-Don
A. V. Simonovа
Russian Federation
Anna V. Simonova, Cand. Sci. (Med.), Manager of Intensive Care unit SRIOP
Rostov-on-Don
T. N. Aleksanyants
Russian Federation
Tatyana N. Aleksanyants, anesthesiolog-resuscitator the highest category of Intensive Care unit SRIOP
Rostov-on-Don
Review
For citations:
Pukhtinskaya M.G., Estrin V.V., Lebedenko A.A., Porutchikovа Yu.A., Simonovа A.V., Aleksanyants T.N. A case of timely diagnosis and successful surgical correction of the left pulmonary artery sling in a newborn. Medical Herald of the South of Russia. 2021;12(1):82-88. https://doi.org/10.21886/2219-8075-2021-12-1-82-88







































