Scroll to:
Features of atherosclerotic lesions of the coronary arteries in patients with myocardial infarction and concomitant newly diagnosed hypothyroidism
https://doi.org/10.21886/2219-8075-2024-15-3-55-61
Abstract
Objective: to assess the incidence of newly diagnosed subclinical and manifest hypothyroidism in patients with ST-segment elevation myocardial infarction (STEMI) and to identify angiographic features of coronary artery lesions in this combined pathology.
Materials and methods: in all patients with STEMI, the level of thyroid-stimulating hormone (TSH) was determined, and thyroid function was assessed if the TSH level deviated from the norm. Stage I of the study included 441 patients, stage II included 133 patients with STEMI. Depending on the presence of newly diagnosed hypothyroidism, patients were divided into 3 groups: 1st — patients without hypothyroidism (n = 57), 2A group — with subclinical hypothyroidism (n = 42) and 2B group — with manifest hypothyroidism (n = 34). All patients underwent coronary angiography and percutaneous coronary intervention.
Results: newly diagnosed hypothyroidism occurred in 27.44% of patients with STEMI: subclinical — in 19.73%, manifest — in 7.7% of cases. Patients with concomitant overt hypothyroidism had significantly more severe atherosclerotic lesions of the coronary arteries compared to patients without hypothyroidism.
Conclusion: a high incidence of newly diagnosed hypothyroidism in patients with STEMI was established (27.44% of cases). Multivessel coronary lesions were recorded more often in patients with overt hypothyroidism than in patients with subclinical hypothyroidism and without hypothyroidism.
Keywords
For citations:
Gridneva Yu.Yu., Chesnikova A.I., Khripun A.V., Safronenko V.A., Pashchenko E.V. Features of atherosclerotic lesions of the coronary arteries in patients with myocardial infarction and concomitant newly diagnosed hypothyroidism. Medical Herald of the South of Russia. 2024;15(3):55-61. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-3-55-61
Introduction
Cardiovascular diseases (CVDs) have been the leading cause of death worldwide for decades [1–3]. Comorbidity is currently one of the most pressing issues in patients with CVDs in modern practice, and its role is widely discussed in the scientific literature [4–7]. The impact of primary subclinical and overt hypothyroidism on coronary artery disease (CAD) progression and the severity of myocardial infarction (MI) has been discussed for a long time.
According to a number of authors, thyroid dysfunction is detected in 10–15% of the adult population [6][7]. The prevalence of overt hypothyroidism in patients over 60 years of age reaches 12%, and that of subclinical hypothyroidism – 26% [7][8].
One of the pressing issues concerning this relationship is the impact of thyroid hormone imbalance on the coronary bed. Results of scientific research demonstrate conflicting data: some authors indicate the progression of coronary atherosclerosis in conditions of severe dyslipidemia; however, other authors have not revealed a statistically significant effect of hypothyroidism on coronary atherosclerosis severity [9].
It should be noted that modern researchers have not come to a consensus on the effect of subclinical hypothyroidism on the CAD course [10][11]. Despite the interest of the authors in the problem of the combination of CVDs and hypothyroidism, the incidence rate of newly diagnosed hypothyroidism and CAD in patients with MI in the presence of concomitant hypothyroidism remains insufficiently studied [9][12–14].
The study was aimed at assessing the incidence rate of newly diagnosed subclinical and overt hypothyroidism in patients with STEMI and identifying angiographic features of CAD in this combined pathology.
Material and methods
At the first stage of the study, the thyroid-stimulating hormone (TSH) level was determined in all patients consecutively admitted to the cardiology department No. 1 of the Regional Vascular Center of the Rostov Regional Clinical Hospital with STEMI from 2022 to 2023, and thyroid function was assessed in case of deviation of the TSH level from the normal range [15]. The following patient data were entered into specially developed questionnaires: gender, age, body mass index, risk factors, the presence of concomitant pathology, hereditary history, and the duration and characteristics of the CAD course before hospitalization. The study included a total of 441 patients with STEMI, whose average age was 61.73 ± 0.51 years.
The second stage of the study included 133 patients with STEMI aged 40 to 88 years [15].
Inclusion criteria were as follows: patients with acute STEMI without thyroid dysfunction and with newly diagnosed subclinical or overt hypothyroidism who signed written informed voluntary consent to participate in the study.
Exclusion criteria were as follows: amiodarone intake at the time of admission and in the anamnesis; coronavirus infection COVID-19 (positive test for SARS-CoV-2 antigens in nasopharyngeal and oropharyngeal swabs) during hospitalization and during inpatient treatment; thyroid surgery; hemodynamically significant heart defects; oncological diseases; vascular delirium; severe renal and hepatic dysfunction; acute cerebrovascular accident and transient ischemic attack within the last 6 months; mental illness that prevents signing voluntary consent and participating in the study.
Depending on the presence of newly diagnosed hypothyroidism, all patients were divided into three groups: group I (control group, n = 57) – patients with STEMI without hypothyroidism (mean age was 60.09 ± 1.2 years); group IIA (n = 42) – patients with STEMI and subclinical hypothyroidism (mean age was 60.95 ± 1.73 years), and group IIB (n = 34) – patients with STEMI and overt hypothyroidism (mean age was 64.59 ± 1.6 years) [15].
The diagnosis of STEMI was established based on electrocardiogram data (ST segment elevation more than 2 mm), as well as in the presence of a positive quantitative troponin test (more than 40 ng/L). In the study groups, the localization of infarction mainly along the anterior or inferior wall of the left ventricle was almost comparable; statistically significant differences between them were not observed (p>0.05). All patients underwent percutaneous coronary intervention and stenting of the infarct-related artery with drug-eluting stents, STEMI treatment was performed according to modern clinical guidelines [4][5].
In order to assess thyroid function, the concentration of TSH, levels of free triiodothyronine (FT3) and free thyroxine (FT4), and thyroid peroxidase antibodies were determined, and an ultrasound examination of the thyroid gland was performed.
Subclinical hypothyroidism was diagnosed in cases when patients had an increase in the TSH level of more than 4.0 μIU/mL without characteristic clinical manifestations and with FT3 and FT4 values within the normal range. Overt hypothyroidism was diagnosed with an increase in the TSH level of more than 4.0 μIU/mL and a decrease in the level of thyroid hormones (FT4) below the reference values. An important stage in the diagnosis of overt hypothyroidism was considered to be the identification of characteristic clinical symptoms: severe fatigue, drowsiness, dry skin, hair loss, swelling of the face, fingers, and toes, obstipation, memory loss, etc. [8][15]. However, in patients with newly diagnosed overt hypothyroidism in the acute MI period, characteristic clinical signs were not determined; therefore hypothyroidism was revealed based on laboratory test data.
Patients with newly diagnosed hypothyroidism were referred to an endocrinologist. Treatment of overt hypothyroidism was performed according to current clinical recommendations (sodium levothyroxine at an average dosage of 50 mcg/day) [8].
Data on the prevalence of coronary atherosclerosis and the severity of stenosis of the coronary arteries based on the results of coronary angiography (CAG) for each patient were reflected in specially developed questionnaires.
Statistical processing of the obtained results was performed using the STATISTICA 13.3 application program (manufacturer StatSoft Inc., USA). The sample was tested for compliance with the normal distribution using the Shapiro-Wilk criterion. Quantitative data corresponding to the normal distribution were presented as the mean and the standard deviation (M ± m). Quantitative data differing from the normal distribution were described by the median and interquartile range (Me [Q1–Q3]). Qualitative variables were presented as absolute (n) and relative (%) values. Comparison of groups by qualitative characteristics was performed using Yates' chi-squared test, and by quantitative characteristics – using the Mann-Whitney U test for two independent groups. The Kruskal-Wallis ANOVA test was used to compare three groups of patients. The critical level of reliability of the null statistical hypothesis was taken to be p<0.05.
The study was performed at the Regional Vascular Center of the Rostov Regional Clinical Hospital. The study complied with the standards of the Declaration of Helsinki and was approved by the independent ethics committee of the Rostov State Medical University of the Ministry of Health of the Russian Federation (protocol No. 16/21 dated October 21, 2021).
Results
Based on the data obtained, it should be noted that 305 of 441 patients (69.16%) had no thyroid dysfunction. The screening study results revealed that newly diagnosed hypothyroidism occurred in 27.44% (n = 121) of patients with STEMI, with its subclinical form occurring in 19.73% (n = 87) of cases and overt form occurring in 7.7% (n = 34) of cases. The data obtained indicated a high incidence rate of newly diagnosed hypothyroidism in patients with STEMI — in every 3rd–4th case. Hyperthyroidism was newly diagnosed in 10 patients, accounting for 2.27% of cases (subclinical hyperthyroidism was revealed in 9 patients, overt hyperthyroidism — in 1 patient).
In the study participants with STEMI without concomitant thyroid pathology, the average TSH level was 2.39 [ 1.62; 3.04] μIU/mL, while in all patients with newly diagnosed hypothyroidism, it was 5.81 [ 4.66; 9.0] μIU/mL (p<0.001). It should be mentioned that in patients with newly diagnosed hypothyroidism, the TSH level was above 10 μIU/mL in 21.9% of cases, which amounted to 6.1% (n = 27) of the total number of patients included in the screening. In patients with overt hypothyroidism, the FT3 level was 2.11 [ 1.93; 2.48] pg/mL, and FT4 — 0.79 [ 0.62; 0.85] ng/dL.
The second stage of the study was devoted to the examination of coronary artery damage during hospital treatment depending on the presence of concomitant hypothyroidism.
According to the CAG conducted in the groups, analysis of the CAD results allowed revealing that one-, two-, and three-vessel CAD in the control and subclinical and overt hypothyroidism groups did not differ statistically significantly (p>0.05). Herewith, in patients with overt hypothyroidism, multivessel CAD (more than three vessels) occurred statistically significantly more often than in the control group patients (p=0.005). It was found that the frequency of multivessel CAD in patients in the STEMI group without hypothyroidism and in patients with STEMI and subclinical hypothyroidism did not differ significantly (p>0.05).
In a comparative aspect, the CAD analysis according to CAG data in patients with STEMI in the study groups is presented in Figure 1.
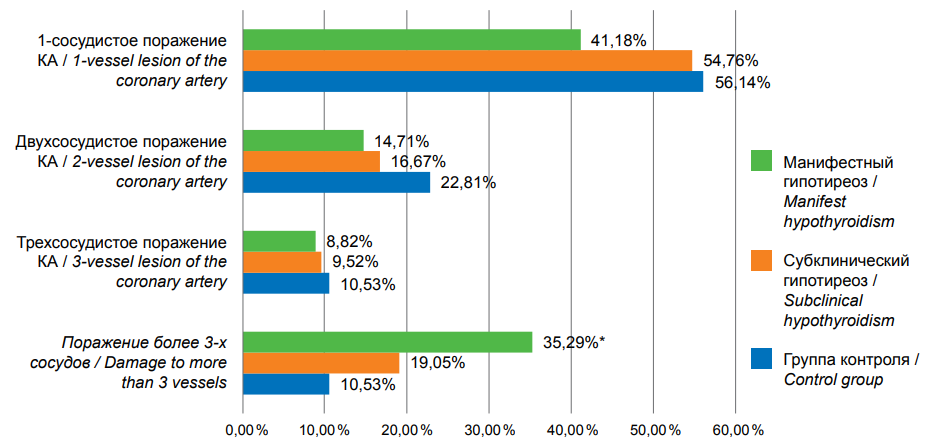
Рисунок 1. Анализ поражения коронарных артерий у больных с ИМпST в исследуемых группах.
Figure 1. Analysis of coronary artery lesions in patients with STEMI in the study groups.
Примечание: * — р=0,005, при сравнении группы пациентов с манифестным гипотиреозом с группой контроля.
Note: * — p=0.005 when comparing the group of patients with manifest hypothyroidism with the control group.
A detailed analysis of the CAG data in the study groups revealed that in patients with STEMI and subclinical hypothyroidism, a statistically significant higher incidence rate of anterior interventricular branch (AIB) lesion with 50–74% stenosis was recorded compared to the control group (p=0.036); a tendency toward lesion of the diagonal branch (DB) with 50–74% stenosis was also determined compared to the group of patients without concomitant thyroid pathology (p=0.078).
The most pronounced atherosclerotic changes in the coronary arteries were registered in patients with STEMI and overt hypothyroidism (group IIB) in comparison with both the control group and patients in the subclinical hypothyroidism group (group IIA). Thus, hemodynamically significant stenoses (50–74% and more than 75%) of the left coronary artery (LCA) trunk and circumflex branch (CB), as well as 50–74% stenosis of AIB, DB, and obtuse marginal branch (OMB) were statistically significantly more common in patients in group IIB in comparison with patients in the control group (p<0.05) (Figure 2).
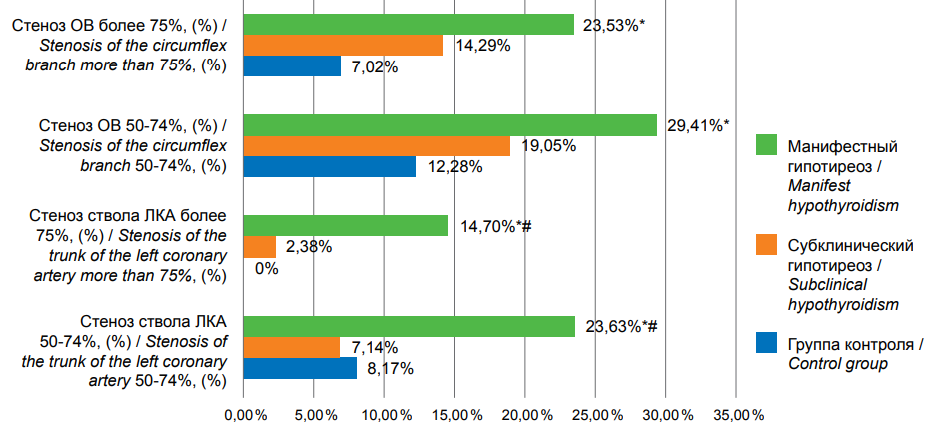
Рисунок 2. Анализ поражения ствола ЛКА и ОВ у больных с ИМпST в исследуемых группах.
Figure 2. Analysis of lesions of the left coronary artery trunk and OS in patients with STEMI in the study groups.
Примечание: * — р<0,05, при сравнении с группой контроля, # — р<0,05, при сравнении с группой с субклиническим гипотиреозом.
Note: * — p<0.05 when compared with the control group, # — p<0.05 when compared with the group with subclinical hypothyroidism.
In addition, patients in group IIB had significantly more frequent lesions of the LCA, right coronary artery, DB, and OMB with 50–74% stenosis compared to patients in group IIA (p<0.05).
The lesions of the coronary arteries in patients in these groups are shown more clearly in Figure 3.
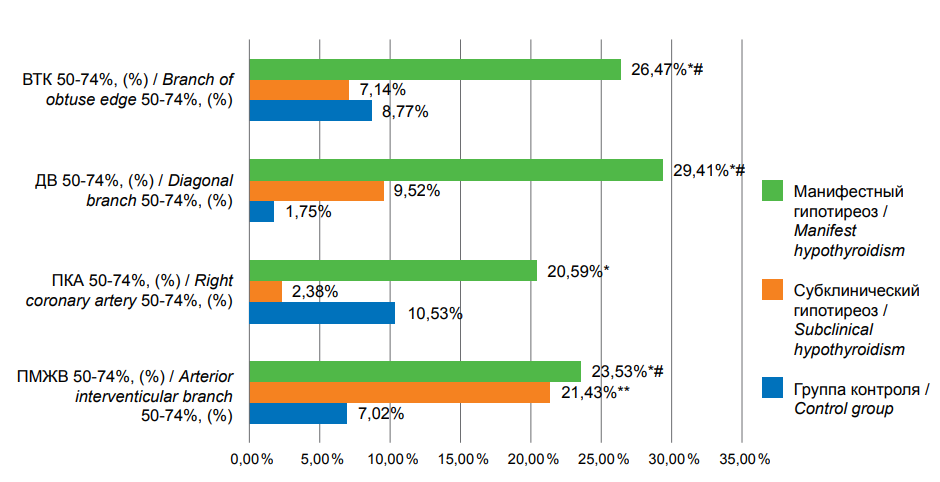
Рисунок 3. Анализ поражения коронарных артерий у больных с ИМпST в исследуемых группах.
Figure 3. Analysis of coronary artery lesions in patients with STEMI in the study groups.
Примечание: * — р<0,05, при сравнении с пациентами с субклиническим гипотиреозом, ** — р<0,05, при сравнении с пациентами без гипотиреоза, # — р<0,05, при сравнении с пациентами без гипотиреоза.
Note: * — p<0.05 when compared with patients with subclinical hypothyroidism, ** — p<0.05 when compared with patients without hypothyroidism, # — p<0.05 when compared with patients without hypothyroidism.
Therefore, patients with STEMI and concomitant newly diagnosed subclinical and overt hypothyroidism had statistically significantly more pronounced atherosclerotic lesions of the coronary arteries compared to patients without thyroid pathology. Multivessel CAD was significantly more common in patients with overt hypothyroidism than in patients with subclinical hypothyroidism and without hypothyroidism.
Discussion
According to the conducted screening study, newly diagnosed hypothyroidism was revealed in 27.44% of patients with STEMI, with the subclinical form of the disease occurring in 19.73% of cases and the overt form occurring in 7.7% of cases. There are no data in the modern literature on the frequency of newly diagnosed subclinical and overt hypothyroidism in patients with STEMI.
A number of studies have shown a higher risk of developing CAD and MI in patients with hypothyroidism. One of the largest meta-analyses, including 55 studies and a total of 1,898,314 patients, demonstrated that the presence of overt hypothyroidism was associated with an increased risk of myocardial ischemia (by 13%), MI (by 15%), arrhythmia, and overall mortality (by 25%) compared with euthyroidism [10–13].
According to research data from a number of authors, patients with CAD, including those with MI and concomitant hypothyroidism, have significantly higher values of atherogenic fractions of lipoproteins, serum triglycerides, and plasma homocysteine than patients with normal thyroid function [10][11][15]. The more pronounced degree and prevalence of atherosclerosis in the present study in patients with STEMI and overt hypothyroidism was apparently due to a number of factors. As is known, in addition to atherogenic dyslipidemia, the development and progression of atherosclerosis are affected by systemic inflammation. According to literature data, patients even with subclinical hypothyroidism had higher concentrations of C-reactive protein and homocysteine, a dependence of homocysteine concentration on the FT4 level, and more pronounced endothelial dysfunction [10][11][15], which could also contribute to the progression of coronary artery atherosclerosis in patients with STEMI and concomitant hypothyroidism [9][15].
The data obtained in the study, indicating a high prevalence of concomitant hypothyroidism in patients with STEMI admitted to the cardiology department (in every 3–4 cases), demonstrated that it was necessary to determine the TSH level in all patients with STEMI, which allowed timely detection of this concomitant pathology and optimization of patient management tactics. Achieving euthyroidism by means of replacement therapy will obviously reduce the risk of developing cardiovascular complications in MI [12–14], which is known to be significantly increased in concomitant hypothyroidism [15].
The importance of timely detection of overt hypothyroidism in patients with MI is also due to the need for more careful monitoring of possible side effects during the use of statins. It should be mentioned that the presence of hypothyroidism requires caution when prescribing statins due to the risk of myopathy/rhabdomyolysis, and the use of a high dose of rosuvastatin is completely contraindicated [12–13]. Studies by a number of authors have shown positive dynamics of hemodynamic parameters, as well as lipid profile parameters during the use of levothyroxine in patients with CAD and hypothyroidism [14–16].
Conclusion
In patients with STEMI, hypothyroidism was first detected in 27.44% of cases: subclinical hypothyroidism in 19.73% of cases and overt hypothyroidism in 7.7% of cases.
Patients with STEMI and concomitant newly diagnosed subclinical and (especially) overt hypothyroidism had statistically significantly more severe atherosclerotic CAD compared to patients without hypothyroidism. Multivessel CAD was significantly more common in patients with overt hypothyroidism than in patients with subclinical hypothyroidism and without hypothyroidism.
The results of the study indicate the need for early detection of concomitant hypothyroidism in patients with STEMI for the purpose of timely drug correction and improved prognosis.
References
1. Izkhakov E, Zahler D, Rozenfeld KL, Ravid D, Banai S, et al. Unknown subclinical hypothyroidism and in-hospital outcomes and short- and long-term all-cause mortality among ST segment elevation myocardial infarction patients undergoing percutaneous coronary intervention. J Clin Med. 2020; 9(12):3829. https://doi.org/10.3390/jcm9123829
2. Nowbar AN, Gitto M, Howard JP, Francis DP, Al-Lamee R. Mortality from ischemic heart disease. Circ Cardiovasc Qual Outcomes. 2019;12(6):e005375. https://doi.org/10.1161/circoutcomes.118.005375
3. Korzukhin A.Yu., Yuldoshev J.R., Troshina A.A., Khuramshina L.R., Guzarik V.N., et al. Type 2 myocardial infarction: diagnostic and therapeutic difficulties in modern cardiology. Complex Issues of Cardiovascular Diseases. 2023;12(3):84-97. (In Russ.) https://doi.org/10.17802/2306-1278-2023-12-3-84-97
4. Korobka V.L., Khripun A.V., Malevannyy M.V., Kulikovskikh Ya.V. The short-term and mid-term outcomes of percutaneous coronary intervention with implantation of bioresorbable vascular scaffolds for STEMI treatment. Endovaskulyarnaya khirurgiya = Russian Journal of Endovascular Surgery. 2015;2(1–2):58–68 (In Russ.). EDN: XGWEYF.
5. Razvi S, Leng O, Jabbar A, Bano A, Ingoe L, Addison C, et al. Sample Timing, Diagnosis of Subclinical Thyroid Dysfunction and Mortality in Acute Myocardial Infarction: ThyrAMI1 Study. J Clin Endocrinol Metab. 2020;105(4):dgz143. https://doi.org/10.1210/clinem/dgz143. PMID: 31769839.
6. Zghebi SS, Rutter MK, Sun LY, Ullah W, Rashid M, et al. Comorbidity clusters and in-hospital outcomes in patients admitted with acute myocardial infarction in the USA: A national population-based study. PLoS One. 2023;18(10):e0293314. https://doi.org/10.1371/journal.pone.0293314
7. Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000;160(4):526–534. https://doi.org/10.1001/archinte.160.4.526
8. Eagan D, Spencer-Bonilla G, Maraka S, Aggarwal M, Singh Ospina N. Management of Hypothyroidism in Patients with Acute Myocardial Infarction. Medicina (Kaunas). 2020;56(5):214. https://doi.org/10.3390/medicina56050214
9. Rahman M.A., Vijayaraghavan G., Ankudinov A.S., Kalyagin A.N. State of the coronary arteries and assessment of the role of hormone replacement therapy in patients with coronary heart disease against the background of primary manifest hypothyroidism. Kardiologiia. 2020;60(9):76-83. https://doi.org/10.18087/cardio.2020.9.n1029
10. Drapkina O.M., Gegenava B.B., Morgunova T.B., Fadeev V.V. Effect of hypothyroidism on the cardiovascular system. Endokrinologiya: novosti, mneniya, obuchenie = Endocrinology: News, Opinions, Training. 2016;2(15):21–30 (In Russ.). EDN: WHOUSX.
11. Khan R, Zarak MS, Munir U, Ahmed K, Ullah A. Thrombolysis in Myocardial Infarction (TIMI) risk score assessment for complications in acute anterior wall ST elevation myocardial infarction. Cureus. 2020; 12(6): e8646. https://doi.org/10.7759/cureus.8646
12. Corona G, Croce L, Sparano C, Petrone L, Sforza A, et al. Thyroid and heart, a clinically relevant relationship. J Endocrinol Invest. 2021;44(12):2535–2544. https://doi.org/10.1007/s40618-021-01590-9
13. Ning Y, Cheng YJ, Liu LJ, Sara JD, Cao ZY, et al. What is the association of hypothyroidism with risks of cardiovascular events and mortality? A meta-analysis of 55 cohort studies involving 1,898,314 participants. BMC Medicine. 2017; 15(1): 21. https://doi.org/10.1186/s12916-017-0777-9
14. Liu D, Jiang F, Shan Z, Wang B, Wang J, et al. A cross-sectional survey of relationship between serum TSH level and blood pressure. J Hum Hypertens. 2010;24(2):134-138. https://doi.org/10.1038/jhh.2009.44
15. Gridneva Yu.Yu., Chesnikova A.I., Safronenko V.A., Edlenko E.V., Zatloukal M.Yu. Incidence and clinical significance of newly diagnosed hypothyroidism in patients with ST-segment elevation myocardial infarction. Therapy. 2024;10(4):82–90. https://doi.org/10.18565/therapy.2024.4.82-90
16. Gluvic ZM, Zafirovic SS, Obradovic MM, Sudar-Milovanovic EM, Rizzo M, Isenovic ER. Hypothyroidism and risk of cardiovascular disease. Curr Pharm Des. 2022;28(25):2065–2072. https://doi.org/10.2174/1381612828666220620160516
About the Authors
Yu. Yu. GridnevaРоссия
Yulia Y. Gridneva, postgraduate student of the Department of Internal Medicine No. 1;
cardiologist of the Cardiology Department No. 1
Rostov-on-Don
A. I. Chesnikova
Россия
Anna I. Chesnikova, Cand. Sci. (Med.), Professor, Head of the Department of Internal Medicine No. 1
Rostov-on-Don
A. V. Khripun
Россия
Alexey V. Khripun, Cand. Sci. (Med.), Director of the Regional (head) Vascular Center;
Associate Professor of the Department of Internal Medicine No. 1
Rostov-on-Don
V. A. Safronenko
Россия
Victoria A. Safronenko, Cand. Sci. (Med.), Associate Professor, Department of Internal Medicine No. 1
Rostov-on-Don
E. V. Pashchenko
Россия
Ekaterina V. Pashchenko, Cand. Sci. (Med.), endocrinologist at the emergency department;
assistant at the Department of Internal Medicine No. 1
Rostov-on-Don
Review
For citations:
Gridneva Yu.Yu., Chesnikova A.I., Khripun A.V., Safronenko V.A., Pashchenko E.V. Features of atherosclerotic lesions of the coronary arteries in patients with myocardial infarction and concomitant newly diagnosed hypothyroidism. Medical Herald of the South of Russia. 2024;15(3):55-61. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-3-55-61
JATS XML







































