Scroll to:
Surgical aspects of treatment of hiatal hernia
https://doi.org/10.21886/2219-8075-2024-15-4-104-112
Abstract
Objective: enhancement the outcome of treatment of patients with complicated forms of hiatal hernia (HH) on the base on a devised personal complex approach.
Materials and methods: the review was carried out of 204 patients with complicated forms of HH at the age of 17 to 77 years (men — 44%, women — 56.4%). All 204 patients suffered from gastroesophageal reflux disease (GERD). In 53 (26%) cases synthetic mesh implants were used during surgical management. In 38 patients (18.6%) with hiatal hernia and metaplasia of the esophageal mucosa (ESM) exposed to complex treatment, which includes antireflux surgical management and argon plasma coagulation (APC).
Results: early postsurgical complications we met more oſten in the group of patients the ones we used mesh. Late postsurgical complications in the group of patients where mesh implants were used according to the indications were met less oſten. when assessing the quality of life according to the questionnaires GERD-HRqL and GSRS, the subjective symptoms of GERD decrease dramatically aſter surgical treatment (in 3 months), continue to decline up to 12 months, aſter which they acquire a constant character. In patients with hiatal hernia, which has become complicated by ESM metaplasia, aſter completing the courses of argonoplasmic coagulation, in all cases, complete regression of the metaplastic epithelium was registered by us.
Conclusions: surgical management of complicated forms of HH using video laparoscopic technique based on the developed algorithm is highly effective, which is confirmed by the low quantity of postsurgical complications and a major improvement of the quality of life of patients.
For citations:
Cherkasov D.M., Cherkasov M.F., Tat’yanchenko V.K., Starcev Y.M., Melikova S.G., Galashokyan K.M., Skuratov A.V., Endorenko K.V. Surgical aspects of treatment of hiatal hernia. Medical Herald of the South of Russia. 2024;15(4):104-112. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-4-104-112
Introduction
Hiatal hernia is one of the most common diseases in the world, almost always complicated by gastroesophageal reflux [1]. Less frequent but more serious complications include esophageal metaplasia, erosions, ulcers, stenosis, strangulation, and bleeding. According to many studies, metaplastic changes in the esophageal mucosa increase the risk of developing malignant tumors [2].
Surgical intervention has long been integrated into the complex treatment of patients with complicated hernias, but most surgeons still need to improve their understanding of the mechanisms of hernia development and the anatomical features of the body [1][3].
There is still no clear answer to the question of how to perform diaphragmatic defect plastic surgery in the case of esophageal hernia. Also, no general opinion exists on whether or not to use synthetic implants, and if so, which ones and in what cases [3–5].
When diagnosing in patients such a complication of hiatal hernia as metaplasia of the esophageal mucosa, a comprehensive approach is used, which includes not only anti-reflux surgery but also pre- and postoperative conservative therapy, as well as endoscopic intervention in various ways on the pathologically altered esophageal mucosa [6].
The study was aimed at improving the treatment results of patients with complicated hiatal hernia based on the developed individual comprehensive approach and anatomical studies.
Materials and methods
Anatomical study. Age and constitutional features of the biomechanical properties of fascial structures, as well as the blood supply to the diaphragm, were studied on 40 preparations from the corpses of people aged 19 to 75 years who died from causes not related to diseases of the digestive organs and cardiovascular system.
It has been found that starting from the second period of mature age, the elastic tissue of the fascial structures of the diaphragmatic crus degenerates, which is accompanied by cicatricial changes in the collagen bundles in these anatomical formations. In old age, the fascial structures of the diaphragmatic crus lose their strength and elasticity.
Starting from the second period of mature age, especially in brachymorphic people, the number of fat fibers surrounding the esophageal hiatus decreases significantly. This is one of the predisposing factors for the development of diaphragmatic hernia. In the process of anatomical studies from the second period of mature age, a pronounced decrease in the blood circulation of muscle tissues in the diaphragm area was also detected. Analysis of the diameter of the vessels supplying these muscle tissues showed a significant decrease in the diameter of the main vessels and their branches; in addition, the number of branches of orders III–IV decreased, and they developed tortuosity, which led to a decrease in vascularization in the diaphragm tissues. A study of the capacity of the arterial bed revealed its decrease by 1.5–2 times in the elderly age period.
Clinical study. The Rostov State Medical University Clinic analyzed the complex therapy of 204 patients with various forms of complications of hiatal hernia. It should be noted that the majority of patients (52.4%) were in the middle age group, the total age ranged from 17 to 77 years. Based on the anatomical studies, all 204 patients were divided by body type.
According to the classification of Petrovsky and Kanshin (1962), hiatal hernias are divided into axial and paraesophageal. This study included more patients with axial hernias (156 patients (76.5%)). In order to assess the hiatal defect in the treatment of this category of patients, Granderath’s formula was used, which allowed calculating the area of the hiatal defect, which was one of the most important data that allowed deciding on the choice of plastic surgery of the diaphragmatic crura in the preoperative period.
This study showed that 100% of patients suffered from gastroesophageal reflux disease; in addition, during the examination, other complications associated with the hiatal hernia were identified in patients.
The distribution of patients by body type and esophageal hiatus area, as well as the list of hiatal hernia complications, are presented in Table 1.
Таблица / Table 1
Основные характеристики пациентов
Basic patient characteristics
|
Характеристики пациентов Patient characteristics |
Количество пациентов (абс, %) Number of patients (abs., %) |
|
I. По типу телосложения / By body type: |
|
|
Брахиморфный тип / Brachymorphic type |
62 (30,4) |
|
Мезоморфный тип / Mesomorphic type |
108 (52,9) |
|
Долихоморфный тип / Dolichomorphic type |
34 (16,7) |
|
II. По площади дефекта пищеводного отверстия диафрагмы / By the area of the defect of the esophageal opening of the diaphragm: |
|
|
1. Аксиальные грыжи / Axial hernias |
|
|
Малая / Small |
54 (26,5) |
|
Большая / Large |
88 (43,1) |
|
Гигантская / Giant |
14 (6,9) |
|
2. Параэзофагеальные грыжи / Paraesophageal hernias |
|
|
Большая / Large |
32 (15,7) |
|
Гигантская / Giant |
16 (7,8) |
|
III. По осложнениям ГПОД / By complications of hiatal hernias: |
|
|
ГЭРБ / GERD |
204 (100) |
|
Эрозивно-язвенные изменения СОП / Erosive and ulcerative changes in the mucous membrane of the esophagus |
29 (14,2) |
|
Метаплазия желудочного типа / Gastric type metaplasia |
11 (5,4) |
|
Метаплазия кишечного типа / Intestinal type metaplasia |
27 (13,2) |
|
Пептическая стриктура пищевода / Peptic stricture of the esophagus |
7 (3,4) |
|
Ущемленная параэзофагеальная грыжа / Strangulated paraesophageal hernia |
1 (0,5) |
All patients with complicated forms of hiatal hernias received complex treatment, including surgical intervention, performed strictly according to indications and including diaphragmatic defect plastic surgery and application of an anti-reflux cuff. The distribution of patients, according to indications for surgical intervention, was as follows:
- inefficient courses of drug therapy (84 people);
- metaplasia of the esophageal mucosa (38 people, including of intestinal type – 27 patients, of gastric type – 11 patients);
- paraesophageal hernia (45 people);
- erosive and ulcerative changes in the esophageal mucosa (29 people);
- esophageal peptic stricture (7 people);
- strangulated paraesophageal hernia (1 person).
Concomitant surgical pathology was detected in 31 patients; this category of patients underwent simultaneous surgical interventions. In the surgical practice, as well as in this study, mesh implants were used quite selectively, according to the specifically developed algorithm, taking into account not only the size of the defect of the esophageal hiatus but also the patient's age and body type. In this regard, out of 204 patients, mesh implants were installed in 53 patients at the stage of plastic surgery of the esophageal hiatus, which amounted to 26% of the total number of patients who underwent complex treatment. Thus, in 29 patients, the reason for installing a mesh implant was giant paraesophageal (13 patients) and axial (16 patients) hiatal hernias. According to the developed algorithm of diaphragmatic defect plastic surgery, mesh implants were installed in 24 patients with large hernias (according to Granderath’s formula) and in the second period of mature age, having a brachymorphic body type.
When performing diaphragmatic crural plastic surgery by cruroraphy, an algorithm developed by the authors of the study was used, in which the size of the hernial defect, body type, and age of patients were evaluated. On this basis, with small sizes of the esophageal hiatus defect, regardless of the body type, the plastic surgery of the diaphragmatic defect was performed exclusively with the use of local tissues. With giant sizes of the hernial defect, cruroraphy was strengthened with an implant; in patients with large hiatal hernias, the plastic surgery of the diaphragmatic crura was performed depending on the body type. Thus, with a dolichomorphic body type, diaphragmocruroraphy was performed with a V-loc thread, and for the purpose of strengthening, single sutures were applied; for this, a VICRYL thread was used. In patients with a brachymorphic body type, diaphragmocruroraphy was strengthened with a mesh implant located in the posterior mediastinum. As for patients with a mesomorphic body type, in this group of patients, depending on the morphofunctional state of the diaphragmatic crura, both of the above-described methods were applicable.
The alloplasty method was as follows: under visual control, a rectangular mesh implant was installed in the posterior mediastinum above the diaphragm so that the long side of the implant was at least 2 cm from the posterior wall of the esophagus, and the surface of the implant covered the esophageal hiatus and the diaphragmatic crura. The endoprosthesis was fixed to the diaphragm at the corners, after which the implant was completely covered by suturing the diaphragm crura so that the outermost suture on the crura was placed above the implant (Patent for Invention of the Russian Federation No. 2611912/01.03.2017 "Method for Surgical Treatment of Hiatal Hernias").
During the examination of 38 patients with hiatal hernias, such a complication of the underlying disease as metaplasia of the esophageal mucosa caused by severe gastroesophageal reflux was detected. In this group of patients, in addition to metaplasia, severe forms of esophagitis were also identified, according to the Los Angeles classification, which required drug therapy at the pre- and postoperative stages of complex treatment. During the examination at the preoperative stage in this group of patients, a mandatory study was a biopsy of the esophageal mucosa, followed by a morphological study. Thus, low-grade dysplasia was detected in nine patients in the group of patients with metaplasia of the esophageal mucosa, which amounted to 23.7%. In all 38 patients, after a morphological study of the biopsy of the esophageal mucosa, high-grade dysplasia was not detected. All patients with metaplasia of the esophageal mucosa, in addition to conservative therapy in the postoperative period, underwent argon plasma coagulation sessions after 30–45 days.
The developed method of argon plasma coagulation (Patent for invention of the Russian Federation No. 2625592/17.07.2017 "Method of endosurgical treatment of Barrett's esophagus") is based on the identification and measurement of the maximum length of the circular segment of metaplasia (MLCSM), which allows the use of this method without fear of complications characteristic of this manipulation.
Argon plasma coagulation (APC) procedure:
- for MDCSM ≤ 1.5 cm, first, APC was performed on two adjacent esophageal walls, then 30 days later – on the two remaining walls;
- for the condition 1.5 cm < MDCSM ≤ 3.0 cm, first, APC was performed on two esophageal walls located one through the other, then 30 days later – on the two remaining walls;
- for MDCSM ˃ 3 cm, first, APC was performed on one esophageal wall, then 30 days later – on the opposite esophageal wall, then 30 days later – on the third esophageal wall, then 30 days later – on the remaining esophageal wall.
The number of APC sessions directly depends on the size of the area affected by metaplasia of the esophageal mucosa. In order to reduce the risk of possible esophageal stricture formation, the surface area subjected to APC should not exceed 4 cm².
Data collection was performed using Microsoft Excel 2013 spreadsheets (Microsoft, USA). Data were processed and analyzed using SPSS Statistic (IBM Statistics, USA) and Stattech v. 3.1.8 (developer: Stattech LLC, Russia) programs.
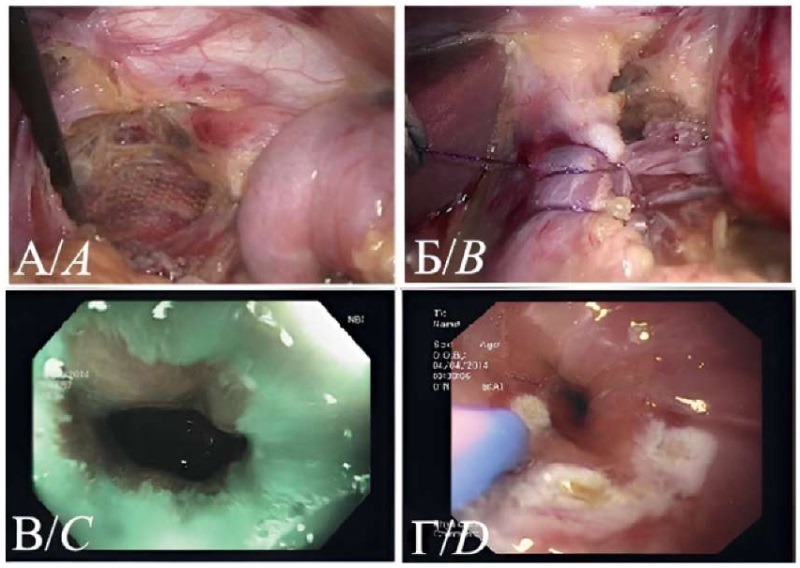
Рисунок 1. Этапы комплексного лечения пациента с грыжей пищеводного отверстия диафрагмы осложненной метаплазией кишечного типа. А — интраоперационное фото, установка синтетического имплантата в заднее средостение. Б — интраоперационное фото, ушивание диафрагмальных ножек. В — эндоскопическое исследование в режиме NBI. Участки измененной слизистой оболочки пищевода. Г — эндоскопическое исследование. Выполнение аргон-плазменной коагуляции.
Figure 1. Stages of complex treatment of a patient with a hiatal hernia complicated by Barrett's esophagus. A — intraoperative photo, installation of a mesh implant in the posterior mediastinum. B — intraoperative photo, suturing of the diaphragmatic crura. C — endoscopic examination in NBI mode. Areas of metaplasia of the esophageal mucosa. D — endoscopic examination. Performing argon plasma coagulation.
Results
A thorough analysis of complications after the implemented complex treatment of hiatal hernia in patients was conducted in the Rostov State Medical University Clinic. In the study, 53 patients out of the total number of patients underwent plastic surgery of esophageal hiatus using a synthetic implant installed in the posterior mediastinum and covered with diaphragmatic crus to avoid mechanical contact of the implant with the hollow organs of the abdominal cavity.
After studying the treatment results of patients who underwent esophageal mucosa plastic surgery using local tissues, 32 patients (21.2%) were found to have postoperative complications, some of patients were diagnosed with more than one complication, which is presented in detail in Table 2.
Таблица / Table 2
Ранние послеоперационные осложнения у пациентов при пластике ПОД местными тканями
Early postoperative complications after plastic using local tissues
|
Осложнения / Complications |
Мужчин / Males (n = 68) |
Женщин / Females (n = 83) |
Всего / Total (n = 151) |
|
Синдром gas-bloat / Gas-bloat syndrome |
8 |
11 |
19 |
|
Дисфагия / Dysphagia |
4 |
4 |
8 |
|
Икота / Hiccups |
1 |
1 |
2 |
|
Диспептические расстройства / Dyspeptic disorders |
5 |
9 |
14 |
|
Всего / Total |
18 |
25 |
43 |
For almost all patients in this group (147 patients out of 151) there were follow-up data. When analyzing postoperative complications, it was found that most complications were treated within a month after surgery. Only three patients had dyspeptic disorders, and one had dysphagia.
As for patients who underwent plastic surgery of esophageal hiatus using a mesh implant, all 53 patients in this category were analyzed. Early postoperative complications were identified in 17 patients. The nature of these complications is presented in Table 3.
Таблица / Table 3
Ранние послеоперационные осложнения у пациентов при пластике ПОД с сетчатым имплантатом
Early postoperative complications after plastic using a mesh implant
|
Осложнения / Complications |
Мужчин / Males (n = 22) |
Женщин / Females (n = 31) |
Всего / Total (n = 53) |
|
Синдром gas-bloat / Gas-bloat syndrome |
3 |
5 |
8 |
|
Дисфагия / Dysphagia |
1 |
2 |
3 |
|
Икота / Hiccups |
– |
1 |
1 |
|
Диспептические расстройства / Dyspeptic disorders |
2 |
3 |
5 |
|
Всего / Total |
6 |
11 |
17 |
A month after the surgery, a small number of complaints were recorded: two patients complained of dyspeptic disorders, two patients – of belching, and one patient – of dysphagia manifestations.
According to the Clavien-Dindo classification, all early postoperative complications identified corresponded to grade I. It should be noted that these complications were more often observed in patients with synthetic implants, but all these complications had a temporary effect and were managed with medications without resorting to repeated surgical interventions.
At a follow-up of up to 5 years, the results in 142 of the 151 patients who did not have mesh implants, which was 94%, and in all 53 patients who had mesh implants were analyzed.
In patients with plastic surgery of diaphragmatic crus with the use of local tissues, the following late complications were identified: migration of the fundoplication cuff (n-3), telescope phenomenon (n-2), cuff hyperfunction (n-2), and gastroesophageal reflux (n-8).
The diagnosed migration and slippage of the gastric cuff did not manifest any clinical symptoms or patient complaints, and therefore there was no need for additional treatment. Other complications identified did not require repeated surgical manipulations and were stopped with the use of drug therapy.
Among 53 patients who were followed up for 5 years and who used a mesh implant as a reinforcing material, such a complication as gastroesophageal reflux was diagnosed only in 2 (3.8%) patients. These patients were prescribed conservative therapy, which gave a positive effect. The conducted studies and their analysis clearly demonstrated that complications in the late postoperative period in patients who used mesh material during esophageal hiatus plastic surgery were detected significantly less frequently than in the group of patients who underwent plastic surgery with the use of local tissues.
The quality of life of patients was assessed by means of generally accepted questionnaires (Fig. 2).

Рисунок 2. Применяемые для оценки качества жизни опросники
Figure 2. Questionnaires used to assess quality of life
The questionnaires allowed establishing that three months after the surgical treatment, the manifestations of reflux decreased quite clearly, the tendency to decrease these manifestations continued for up to a year and then became continuous.
The conducted analysis of the GERD-HRQL questionnaire data in patients with cruroraphy reinforced with the synthetic material revealed high rates in this group of patients before surgery and three months after it compared to the group of patients whose plastic surgery was performed without the use of mesh material (Fig. 3). More pronounced complaints were associated with the fact that initially patients who underwent plastic surgery of esophageal hiatus reinforced with a synthetic implant had larger hernial orifices and experienced more pronounced clinical manifestations.
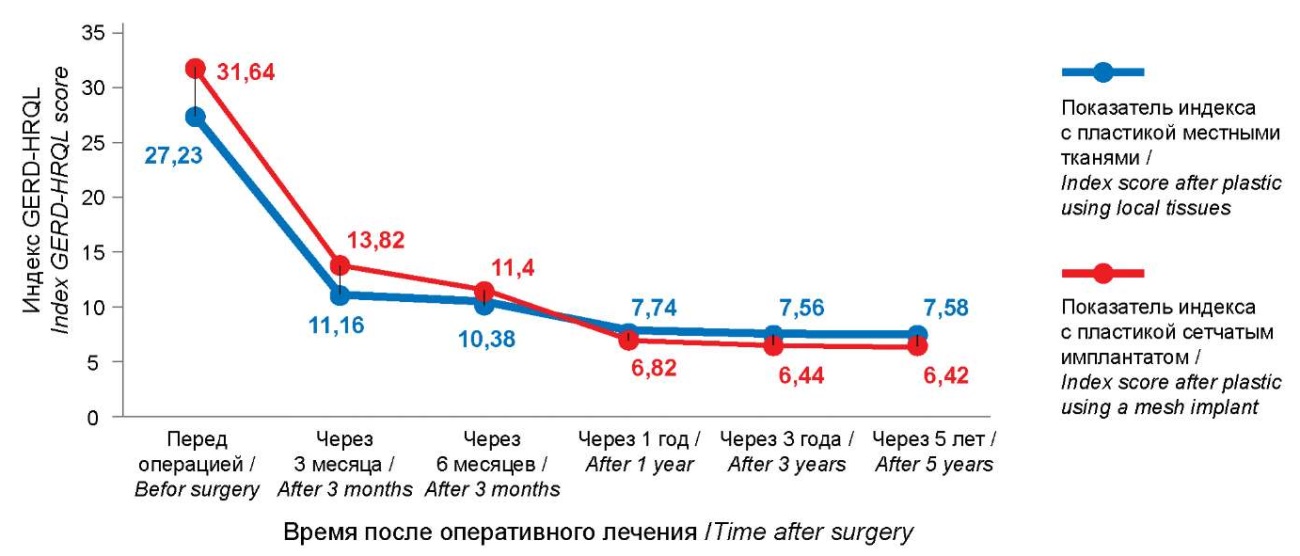
Рисунок 3. Показатели индекса GERD-HRQL
Figure 3. GERD-HRQL index scores
During the analysis of the GSRS questionnaire data in both observation groups, the indices of such scales as "abdominal pain", "reflux syndrome", and the total measurement scale had a significant tendency to decrease by the third month after surgery. By the sixth month, a decrease in these indices had also been observed, and from the 12th month, the values could be compared with the corresponding data of healthy people. When analyzing the "Reflux syndrome" scale, the greatest decrease in indices had already been identified by the third month. It should be noted that in patients whose hernial orifice plastic surgery was supplemented with a mesh implant, a slower decrease in indices was detected. When studying the "Dyspeptic syndrome" scale, normalization of these indices had already been established by the third month; in patients with plastic surgery using only local tissues, the data studied did not differ from the preoperative ones. The indicators of this scale were slightly increased in patients who underwent plastic surgery using synthetic materials, this was due to dyspeptic disorders in the early period after surgery; however, it was noted that by the sixth month of the postoperative period, these indicators had decreased, and by the 12th month after surgery, they had returned to normal indicators characteristic of a healthy person.
According to the SF-36 survey index, the severity of pain had significantly decreased by the third month, and by the sixth month, it no longer differed from normal values. The severity of pain in the postoperative period in patients whose plastic surgery was performed using a synthetic implant was significantly higher than in patients who underwent plastic surgery with the use of local tissues. The remaining SF-36 index scales used in patients of both groups had gradually increased by the third and sixth months of the postoperative period, and by the 12th month they had become the same as in healthy people.
During the entire observation period, not a single relapse of the disease was observed in either group.
In patients with hiatal hernia, in whom metaplasia of the esophageal mucosa was detected during examination, performing anti-reflux surgery led to a significant reduction in inflammatory manifestations on the esophageal mucosa, which in turn allowed performing coagulation under favorable conditions.
No complications were observed during APC.
Patients diagnosed with metaplasia of the esophageal mucosa underwent 2 to 5 sessions of APC.
Complete regression of esophageal mucosal metaplasia by replacing it with stratified squamous epithelium was morphologically confirmed during a control study of biopsy material after completion of all treatment courses. This study did not reveal a relapse of esophageal mucosa metaplasia within five years after the complex treatment.
Discussion
Over the past decades, laparoscopic removal of hiatal hernia has gradually replaced the "open" surgery, becoming the standard approach to treating this pathology [7]. As for the efficiency of using mesh implants for plastic surgery of the esophageal hiatus, it still remains controversial. According to Guan et al., one of the important elements for preventing the anatomical recurrence of hernia is the proper closure of the esophageal hiatus and its reinforcement with mesh [7]. In another study, the authors, although noting the advantages of alloplasty in terms of improving the quality of life and reducing the risk of hernia recurrence, at the same time describe the need for further research to determine clear indications for the use of mesh implants [8].
The conducted literature review has shown that there are practically no works devoted to anatomical studies in the area of the esophageal hiatus to justify the use of synthetic materials. According to the results of anatomical studies, it has been established that in patients from the second mature period, taking into account the decrease in blood supply to the fascial and muscle tissues, which results in ischemia of the esophageal hiatus (especially in patients with a brachymorphic body type), the use of exclusively their own tissues to close the esophageal hiatus defect is insufficient and anatomically and physiologically poorly justified.
The use of synthetic materials in the abdominal cavity is known to be accompanied by trauma to organs and the risk of developing specific complications, such as erosion and pressure ulcers of the esophagus and stomach by the implant (up to perforation); therefore, the installation of a mesh implant in the posterior mediastinum above the diaphragmatic crura and their subsequent suturing prevent contact of the implant with the hollow organs of the abdominal cavity and allow for reliable strengthening of the cruroraphy [1].
In the study performed, complications in the late postoperative period in patients after performing esophageal hiatus plastic surgery using a mesh implant were observed less frequently than in the group of patients with plastic surgery with the use of local tissues, which might be associated with the peculiarities of patient selection in the groups and the selected topographic and anatomical prerequisites for the installation of mesh implants, based on data from anatomical studies.
The data on the quality of life of patients in the postoperative period, obtained through the use of questionnaires, indicated an improvement in the quality of life of patients in both groups. Comparative analysis of these data with data obtained by other authors demonstrates similar results [9].
Restoration of normal morphofunctional relationships of the tissues of the esophagogastric junction during anti-reflux surgery leads to a decrease in the frequency of reflux, which in turn leads to a decrease in inflammatory changes in the esophageal mucosa. Endoscopic eradication of metaplasia foci after surgical intervention to eliminate hiatal hernia is performed under more favorable conditions, which improves the long-term treatment results and is confirmed in the practice of other clinicians [10].
Conclusion
The developed algorithm of surgical treatment allows selecting a method of plastic surgery of esophageal hiatus differentially, based on data on the size of the esophageal hiatus defect, body types, the condition and characteristics of the fascial and muscular structures of the esophageal hiatus zone, as well as the age of the patient.
A new surgical method of strengthening cruroraphy using a mesh implant, which has been developed, allows avoiding possible contact of the mesh with the hollow organs of the abdominal cavity, which in turn significantly reduces the risks of postoperative complications typical for this category of patients.
The developed differentiated method of APC of metaplastic areas of the esophageal mucosa, depending on the size of the MDCSM, provides the opportunity to significantly reduce the number of complications, both intra- and postoperative. This method is well tolerated by patients, and it can be performed in outpatient settings.
The implementation of minimally invasive videoendoscopic surgical interventions based on the algorithm of the developed differentiated approach to plastic surgery of esophageal hiatus with various options has proven its high efficiency and has allowed significantly improving the quality of life and reducing the number of complications in the postoperative period in patients suffering from complicated forms of hiatal hernias.
References
1. Sovpel I, Ishchenko R, Sedakov I, Sovpel O, Mykhaylichenko V, Parshin D. Modern aspects of diagnosis and surgical treatment of hiatal hernias: literature review. Archiv Euro-Medica. 2022;12(1):55-60. https://orcid.org/10.35630/2199-885x/2022/12/1.13
2. Mikhaleva L.M., Voytkovskaya K.S., Fedorov E.D., Birukov A.E., Gracheva N.A., et al. Clinical and morphological analysis of dysplasia in Barrett's esophagus and columnar-lined esophagus. Almanac of Clinical Medicine. 2020;48(2):94-101. (In Russ.) https://orcid.org/10.18786/2072-0505-2020-48-011
3. Petric j, Bright T, Liu DS, wee Yun M, watson DI. Sutured Versus Mesh-augmented Hiatus Hernia Repair: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Ann Surg. 2022;275(1):e45-e51. https://orcid.org/10.1097/SLA.0000000000004902
4. Campos V, Palacio DS, Glina F, Tustumi F, Bernardo wM, Sousa AV. Laparoscopic treatment of giant hiatal hernia with or without mesh reinforcement: A systematic review and meta-analysis. Int J Surg. 2020;77:97-104. https://orcid.org/10.1016/j.ijsu.2020.02.036
5. Rausa E, Manfredi R, Kelly ME, Bianco F, Aiolfi A, et al. Prosthetic Reinforcement in Hiatal Hernia Repair, Does Mesh Material Matter? A Systematic Review and Network Meta-Analysis. J Laparoendosc Adv Surg Tech A. 2021;31(10):1118-1123. https://orcid.org/10.1089/lap.2020.0752
6. Stawinski PM, Dziadkowiec KN, Kuo LA, Echavarria j, Saligram S. Barrett's Esophagus: An Updated Review. Diagnostics (Basel). 2023;13(2):321. https://orcid.org/10.3390/diagnostics13020321
7. Guan L, Nie Y, Yuan x, Chen j, Yang H. Laparoscopic repair of giant hiatal hernia for elderly patients. Ann Transl Med. 2021;9(8):704. https://orcid.org/10.21037/atm-21-1495
8. Laxague F, Sadava EE, Herbella F, Schlottmann F. when should we use mesh in laparoscopic hiatal hernia repair? A systematic review. Dis Esophagus. 2021;34(6):doaa125. https://orcid.org/10.1093/dote/doaa125
9. Chan DL, Tran S, Kanakaratne S, Bruce HM, Thilakanathan C, et al. Long-term outcomes and satisfaction of laparoscopic non-absorbable mesh-reinforced hiatal hernia repair. Surgery Open Digestive Advance. 2022;6:100042. https://orcid.org/10.1016/j.soda.2022.100042
10. Mittal SK, Baboli KM, Bremner RM. Reflux Control Aſter Barrett’s Esophagus Ablation. Foregut. 2021;1(1):78-85. https://orcid.org/10.1177/2634516121997233
About the Authors
D. M. CherkasovRussian Federation
Denis M. Cherkasov, Dr. Sci. (Med.), Professor of the Department of surgical diseases No. 2
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest.
M. F. Cherkasov
Russian Federation
Mihail F. Cherkasov, Dr. Sci. (Med.), Professor, head of the Department of surgery No. 4
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest.
V. K. Tat’yanchenko
Russian Federation
Vladimir K. Tat’yanchenko, Dr. Sci. (Med.), Professor, head of the Department Operative Surgery, Clinical Anatomy and Pathological Anatomy FPK and PPS
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest.
Y. M. Starcev
Russian Federation
Yurij M. Starcev, Cand. Sci. (Med.), associate Professor of the Department of surgery No. 4
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest.
S. G. Melikova
Russian Federation
Sabina G. Melikova, surgeon
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest.
K. M. Galashokyan
Russian Federation
Karapet M. Galashokyan, Cand. Sci. (Med.), assistant of the Department of surgery No. 4
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest.
A. V. Skuratov
Russian Federation
Andrey V. Skuratov, Cand. Sci. (Med.), assistant of the Department of gastroenterology and endoscopy
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest.
K. V. Endorenko
Russian Federation
Konstantin V. Endorenko, assistant of the Department of Normal Anatomy
Rostov-on-Don
Competing Interests:
Authors declares no conflict of interest.
Review
For citations:
Cherkasov D.M., Cherkasov M.F., Tat’yanchenko V.K., Starcev Y.M., Melikova S.G., Galashokyan K.M., Skuratov A.V., Endorenko K.V. Surgical aspects of treatment of hiatal hernia. Medical Herald of the South of Russia. 2024;15(4):104-112. (In Russ.) https://doi.org/10.21886/2219-8075-2024-15-4-104-112






































