Scroll to:
Assessment of the prevalence of overweight and obesity among school-age children in Samara
https://doi.org/10.21886/2219-8075-2022-13-4-106-113
Abstract
Purpose: Assessment of the prevalence of overweight and obesity among school-age children in Samara. Material and methods. Medical checkup of 1503 schoolchildren aged from 7 to 14 years old was performed. The authors assessed anthropometric indicators, calculated body mass index, and standard deviation score. Diagnosis of overweight or obesity was based on the analysis of the indicators according to the criteria of the World Health Organization. Results. The prevalence of overweight among schoolchildren in Samara made up 20.9% and obesity was observed in 13.5%. The prevalence of obesity among boys was significantly higher than in girls (63.58% vs 39.48%, respectively). The peak debut of obesity occurs at an early school age. In the study group, obesity of 1st degree was most common (67.2% of obese children). A comparison of the obtained data with previous studies revealed that the prevalence of obesity increased dramatically over the past fifteen years (from 3.6% to 13.5%). The prevalence of overweight has also increased from 10.6% to 20.9%. Conclusion. Considering the increasing prevalence of overweight and obesity among school-age children, this problem should remain one of the priorities for the Samara region.
For citations:
Skvortsova O.V., Migacheva N.B., Mikhaylova E.G., Katkova L.I. Assessment of the prevalence of overweight and obesity among school-age children in Samara. Medical Herald of the South of Russia. 2022;13(4):106-113. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-4-106-113
Introduction
Obesity is one of the most challenging modern problems facing the entire medical community. Despite the active methods of control and prevention, the accumulated knowledge, as well as the results of numerous scientific studies, the prevalence of obesity over the world continues to increase, including among the child population. In 2015, 107.7 million children and 603.7 million adults were obese; and since 1980, the prevalence of obesity has doubled in more than 70 countries [1]. At present, the problem of overweight is detected in every fourth inhabitant of Earth and is becoming global. Moreover, in recent years, the attention of scientists has been attracted by the increase in the prevalence of higher classes of obesity and the early development of metabolic syndrome in patients [2]. In addition to the main well-known obesity complications (type 2 diabetes mellitus, hypertension, nonalcoholic fatty liver disease, etc.) leading to early disability and reducing life expectancy, excess weight affects all organs and systems, without exception, disrupting their functioning. The influence of obesity on immunity has recently been attracting more and more attention from scientists. Data have been obtained on changes in the functioning of the immune system in conditions of excess weight and the development of nonspecific inflammation, which, in turn, contributed to the earlier implementation of the main complications of obesity [3][4]. In addition, obesity has been shown to be a risk factor for mortality in viral infections such as COVID-19 [5]. Particular attention has been drawn to the role of obesity during pregnancy. Obesity contributes to multiple risks of developing complications both during pregnancy and childbirth itself (gestational diabetes mellitus, preeclampsia, premature birth, etc.), and leads to adverse consequences for the child in the future [6]. Therefore, in addition to a significant negative impact on the quality of life and social adaptation, especially important in childhood and adolescence, obesity is one of the possible reasons for the potential decline in population growth in the future.
In recent years, data on the prevalence of obesity in children and adolescents in different regions of the Russian Federation have had significant fluctuations in indicators and ranged widely from 2.3% to 14.5% [7][8]. In addition, at present, an insufficient number of large-scale, multicenter epidemiological studies of the epidemiology of obesity in children in the Russian Federation have been conducted. The most significant among them are the studies of the National Medical Research Center for Endocrinology (2006) and the Federal Research Center for Nutrition, Biotechnology, and Food Safety in 2014.
In 2006, examination data of 11,977 adolescents aged 12–17 years living in the Russian Federation were analyzed on the basis of the National Medical Research Center for Endocrinology [9]. It was demonstrated that the prevalence of obesity in Russia among children aged 12–17 was 2.5% in boys and 1.7% in girls, and the prevalence of overweight was 11.02% and 7.7%, respectively. In Samara, according to the same study, obesity was found in 3.6% of children, and overweight – in 10.6% of children. Among the cities that were part of the study, Samara ranked second after Moscow in terms of the prevalence of obesity among adolescents.
In 2014, the Federal Research Center for Nutrition, Biotechnology, and Food Safety conducted another multicenter study on the prevalence of overweight and obesity among children in the Russian Federation [10]. The study included 5,182 children (2,696 boys and 2,486 girls) aged 5, 10, and 15. According to the results of the study, the prevalence of overweight and obesity in the examined children averaged 19.9% and 5.6%, respectively, and was similar in different regions of the Russian Federation.
When considering the global increase in the prevalence of obesity over the world, varying dietary patterns and lifestyles, an important task of public health becomes the assessment of the dynamics of the prevalence of obesity and overweight among the child population.
In this regard, the research was aimed at studying the prevalence of overweight and obesity in dynamics on the example of the child population of one of the districts of the city of Samara, taking into account gender and the degree of obesity in the context of rapidly changing dietary and lifestyle stereotypes.
Materials and methods
A retrospective one-stage single-center study was conducted on the basis of the children's polyclinic department of the State Budgetary Institution of Health of the Samara Region “Samara City Hospital” No. 10 of the Kuibyshev District of Samara from February 2021 to May 2021.
During the annual preventive examination of schoolchildren, 1,503 children aged 7 to 14 years (750 boys and 753 girls; the average age was 10.8 years (± 2.3)) were examined. The research inclusion criteria were as follows: the age of the child from 7 to 14 years; living in the studied area; the absence of diseases directly affecting the growth and physical development of the child (genetic syndromes, severe concomitant somatic diseases in the stage of decompensation); the informed consent of parents to conduct a preventive examination of the child. The research exclusion criteria were as follows: children aged under 7 and over 14 years; the presence of severe concomitant somatic diseases; taking medications that affect appetite regulation (neuroleptics, antidepressants, oral administration of large doses of glucocorticosteroids, etc.).
All children underwent an assessment of anthropometric data: height (m) and weight (kg) were measured, sexual maturation was assessed (according to the Tanner sexual maturity rating scale). All the data obtained were also recorded in the registration form No. 030-PO/u-17 (to the order of the Ministry of Health of the Russian Federation of August 10, 2017 No. 154 n) for 2020–2021. Overweight and obesity were established by means of defining the body mass index (BMI) (kg/m²) with the calculation of the standard deviation score (SDS) using the AnthroPlus software [11].
The calculations were made according to the criteria of the WHO anthropometric standards based on the data of a representative cross-sectional study conducted among children in 1977 in the USA [12]. According to these criteria, excess body weight in children is determined according to percentile tables or standard deviations, which consider not only the height and weight but also the sex and age of the child [13][14]. In the WHO tables and graphs, as well as in the AnthroPlus software, standard deviations are indicated depending on the sex and age of children 5–19 years old. Based on the analysis of these data, according to WHO, the criteria for the diagnosis of overweight are as follows:
BMI-SDS from +1 to +2.
Diagnostic criteria for obesity are as follows:
- BMI-SDS from +2 to 2.5 – obesity class I.
- BMI-SDS from +2.6 to 3.0 – obesity class II.
- BMI-SDS from +3.1 to 3.9 – obesity class III.
- BMI-SDS more than/equal to 4 – obesity class IV.
The obtained data were statistically processed using Microsoft Excel v.16.0.12527.20278 and Statistica v.12.6. for Windows. The prevalence of overweight and obesity was calculated as the percentage of cases of deviation in weight from the total number of children.
Results
When distributing the examined schoolchildren by age, the largest number of children fell into the age group from 9 to 12 years (Figure 1). The overall prevalence of obesity among 1,503 research participants was 13.5%, 20.9% of children were overweight. Significant differences were revealed in the prevalence of obesity among the examined schoolchildren depending on age. The largest number of obese children was defined at the age of 7 years (32.5%), and the smallest number – at the age of 14 years (8.33%). In the interval between these age periods, a consistent decrease in the prevalence of obesity was established. Therefore, among 10-year-old children, 12.4% were obese, and among 13-year-olds – 9.1%. The prevalence of obesity and overweight in children of different age groups is presented in detail in Figure 2.
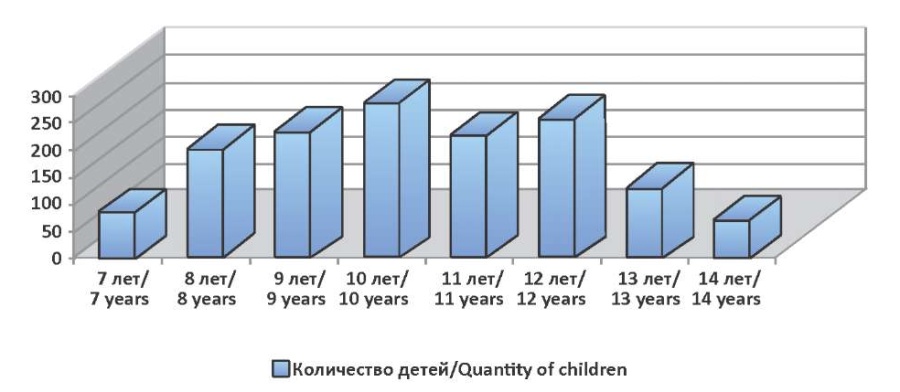
Figure 1. Distribution of children of the studied group by age

Figure 2. Prevalence of obesity and overweight in children of the studied group by age.
The analysis of the data obtained showed that the prevalence of obesity among 7-year-old children predominated over the prevalence of overweight equal to 19.7%, which revealed serious flaws in the regular medical checkup of preschool children. Such indicators are considered to be critical and were not observed in previous years.
When assessing obesity by classes, it was revealed that obesity class I dominated in children and accounted for 67.2% of the total number of obese children. Less common was obesity of class II and class III (23.8% and 9.2%, respectively). Obesity class IV was not revealed in children of the studied group (Figure 3).

Figure 3. Frequency of detection of various degrees of obesity in children of the studied group.
The results of studying the prevalence of obesity and overweight in the distribution of children by gender were also analyzed. Of the total number of patients with obesity, boys accounted for 63.58%, and girls – 39.48% (1.6 times less). Considering the physiological characteristics of the female body, an increase in the occurrence of obesity among girls in puberty could be expected. Therefore, the prevalence of obesity in boys revealed in this study required special consideration. It should be noted that a persistent predominance of obesity in the male population was traced in all age groups (Figure 4), and its sharp increase was revealed at the age of 13 years (83.3%). In girls, the prevalence of obesity remained relatively stable in all age periods with a slight decrease at the age of 12–14 years (29.62–33.3%), which might be associated with an active increase in height.

Figure 4. Prevalence of obesity in children of the studied group by age and gender.
The results of this research were compared with the results of studies in 2006 and 2014, which allowed assessing the dynamics of the prevalence of obesity and overweight in children and adolescents in the city of Samara (Figure 5). An obvious epidemiological trend was a significant increase in the prevalence of obesity among children and adolescents with stable indicators of the incidence of overweight. From 2006 to 2021, the number of obese children in Samara increased from 3.6% to 13.5%. The prevalence of overweight in children increased from 10.6% to 19.5% from 2006 to 2014, respectively. In 2021, this indicator remained practically unchanged compared to 2014 and amounted to 20.9%. The significance of the difference between the studied features and parameters was assessed using Pearson's chi-square test. Differences were considered statistically significant at p<0.05. According to the comparative analysis, there was a statistically significant increase in the prevalence of obesity both from 2006 to 2014 (p=<0.05) and from 2014 to 2021 (p=<0.05). The same results were obtained when statistically comparing the increase in the prevalence of overweight from 2006 to 2014 (p=<0.05) and from 2006 to 2021 (p=<0.05). Therefore, the prevalence of obesity among schoolchildren in Samara increased significantly (from 5.6% to 13.5%, p=<0.05), while there was practically no increase in the prevalence of overweight over the past 7 years (p= 0.189).

Figure 5. Dynamics of the prevalence of overweight and obesity in children from 2006 to 2021.
Discussion
According to the research results, the prevalence of obesity and overweight among school-age children in Samara is currently high (13.5% and 20.9%, respectively) and significantly (more than 2 times) higher than the corresponding figures obtained during the previous studies.
It should be noted that in the studies conducted in Samara in 2006 and 2014, the peak prevalence of obesity was in adolescence (11–13 years); and in 2021, its maximum prevalence was recorded in children of primary school age. Such a sharp increase in the obesity rate in this age group was revealed for the first time, which requires a serious analysis of the causes of the current situation and a review of existing organizational approaches to the prevention of childhood obesity.
While analyzing the reasons that could lead to such a sharp increase in the prevalence of obesity among children and adolescents, one should pay attention to a combination of various social, medical, and psychological factors.
First of all, this is the insufficient health literacy of the population, which has been repeatedly noted by a number of researchers [15][16]. The problem often lies in the lack of understanding by parents of the consequences and complications associated with overweight and obesity, as well as the low awareness of expectant mothers, starting from the pregnancy period, about the importance of developing proper eating habits and an active lifestyle, both in relation to themselves and in regarding their unborn children.
In addition, even from infancy, many children develop a selective appetite with a significant predominance of fast carbohydrates in the diet; in some cases, children get an excessive amount of products based on whole cow's milk, which is often encouraged by parents. Insufficient physical activity in school years, as well as an unbalanced diet with a predominance of carbohydrates, violate the ratio between the intake and the expenditure of calories and energy, which leads to the formation of obesity already in primary school.
At present, a popular trend is the widespread use of various computer gadgets by families, including children, which leads to a significant decrease in their spontaneous physical activity. Considering the increase in school workload, as well as the length of time children spend at school on the second shift, many of them lose interest in active sports and steadily get less opportunities to attend sports sections. It is important to note that children with obesity are assigned to the health group III and, accordingly, to the preparatory group for physical education, which also reduces their physical activity, since these children are engaged in physical activities without passing school standards and they are not allowed to compete. Most physical education teachers do not have sufficient knowledge and motivation to effectively deal with this category of children.
The amount of time families currently spend outdoors continues to decline. Parents, due to responsibility (they do not always let their children go for a walk without supervision) and the lack of free time, do not have time to spend it with their children. This is most often the case in preadolescents.
Many of the children do not receive rational school meals, especially in high school, but purchase them on their own and, as a rule, their choice is in favor of fast carbohydrates. However, those children who receive breakfast and lunch at school are also not limited to school meals. At home, in most cases, they get the first breakfast, and they get some “snacks” after a school lunch as there is such a habit, which, as a rule, does not correspond to the principles of rational nutrition. The combination of the above habits forms the wrong eating behavior in children.
The fact that the children of the studied group had no obesity class IV should also be noted. On the one hand, this may be the result of a rather rigorous approach to the calculation of the analyzed indicators, in particular, BMI-SDS. Despite the sufficient sample size in the research, the probability of detecting morbid obesity may increase with an increase in the number of children examined. On the other hand, the results obtained indicate that the majority of obese children have sufficient potential to prevent disease severity progression. Therefore, the search for efficient and rational strategies for the prevention and early detection of excess body weight can become an important direction of organizational work to suppress the identified trend in the increase in the prevalence of overweight and obesity in children and adolescents in Samara and disease severity progression.
While considering the research problem, it is necessary to pay attention to the existing shortcomings in the provision of medical care to overweight and obese children by the local pediatric service. Their reasons may be the excessive workload of the primary care pediatricians, the prevalence of appeals to them with other problems, and insufficient preventive work with parents. It is obvious that parents often turn to a pediatric endocrinologist late, not at the stage when the child is overweight, but at the stage of obesity or its complications. Early detection of the disease and preventive work are the prerogative of primary care pediatricians, who observe the physical development of the child from an early age.
Unfortunately, to date, due attention is not paid to psychological assistance to overweight children and their families. Only a few patients, usually with a high degree of obesity, regularly work with a psychologist. In some cases, this is due to the lack of positions of clinical psychologists in polyclinic institutions, and in some cases, the patient's family does not consider this necessary.
Conclusion
The research results reveal a high prevalence of obesity and overweight in school-age children in Samara (13.5% and 20.9%, respectively). Moreover, over the past 15 years, there has been an increase in the prevalence of overweight from 10.6% to 20.9% and obesity from 3.6% to 13.5% in children in Samara in the age group from 7 to 14 years. The peak of the obesity onset at the age of 7 years (32.5%) implies the shortcomings of the existing organizational approaches to the medical examination of schoolchildren and the prevention of obesity in children. As the research results indicate, a change in the paradigm of regular medical checkups of children in primary school, with the obligatory participation of a pediatric endocrinologist, as well as the involvement of a pediatrician working in educational institutions in preventive work, is necessary. In addition, there is a need for closer interaction among the local pediatric service and preschool and school educational institutions regarding issues of promoting a healthy lifestyle, proper nutrition, and physical activity.
Information about the contribution of the authors:
Skvortsova O.V: contribution to the concept and design of the study, obtaining and analyzing data, writing an article, agreeing to be responsible for all aspects of the work and to guarantee appropriate consideration and resolution of issues related to the accuracy and integrity of all parts of the work.
Migacheva N.B: a significant contribution to the concept and design of the study, a significant revision of the important scientific and intellectual content of the article, the final approval of the version for publication.
Mikhailova E.G: data analysis and interpretation, final approval of the version for publication.
Katkova L.I: Writing an article, final approval of the version for publication, review of publications on the topic of the article.
References
1. GBD 2015 Obesity Collaborators, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017;377(1):13-27. https://doi.org/10.1056/NEJMoa1614362
2. Chung YL, Rhie YJ. Severe Obesity in Children and Adolescents: Metabolic Effects, Assessment, and Treatment. J Obes Metab Syndr. 2021;30(4):326-335. https://doi.org/10.7570/jomes21063
3. Saltiel AR, Olefsky JM. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest. 2017;127(1):1-4. https://doi.org/10.1172/JCI92035
4. McLaughlin T, Ackerman SE, Shen L, Engleman E. Role of innate and adaptive immunity in obesity-associated metabolic disease. J Clin Invest. 2017;127(1):5-13. https://doi.org/10.1172/JCI88876
5. Sanchis-Gomar F, Lavie CJ, Mehra MR, Henry BM, Lippi G. Obesity and Outcomes in COVID-19: When an Epidemic and Pandemic Collide. Mayo Clin Proc. 2020;95(7):1445-1453. https://doi.org/10.1016/j.mayocp.2020.05.006
6. Catalano PM, Shankar K. Obesity and pregnancy: mechanisms of short term and long term adverse consequences for mother and child. BMJ. 2017;356:j1. https://doi.org/10.1136/bmj.j1
7. Okorokov P.L., Vasyukova O.V., Shiryaeva T.Yu. Resting metabolic rate and factors of its variability in adolescents with obesity. Vopr. det. dietol. (Pediatric Nutrition). 2019;17(3):5–9. (In Russ.). https://doi.org/10.20953/1727-5784-2019-3-5-9
8. Dakhkilgova Kh.T. Childhood obesity: the current state of the problem. Vopr. det. dietol. (Pediatric Nutrition). 2019;17(5):47–53. (In Russ.). https://doi.org/10.20953/1727-5784-2019-5-47-53.
9. Dedov I.I., Mel'nichenko G.A., Butrova S.A., Savel'eva L.V., Bodaveli O.V., et al. Ozhirenie u podrostkov v Rossii. Obesity and metabolism. 2006;3(4):30-34. (In Russ.) https://doi.org/10.14341/2071-8713-5141
10. Tutelyan V.A., Baturin A.K., Kon I.YA., Martinchik A.N., Uglitskih A.K., et al. Prevalence of overweight and obesity in child population of Russia: multicenter study. Pediatria n.a. G.N. Speransky. 2014;93(5).
11. Fediaeva V.K., Bogova E.A., Peterkova V.A., Rebrova O.Yu. Efficacy of interventions for prevention and correction of overweight and obesity in children 7–8 years old: a meta-analysis. Obesity and metabolism. 2020;17(2):115-124. (In Russ.) https://doi.org/10.14341/omet12120
12. Natale V, Rajagopalan A. Worldwide variation in human growth and the World Health Organization growth standards: a systematic review. BMJ Open. 2014;4(1):e003735. https://doi.org/10.1136/bmjopen-2013-003735
13. Peterkova V. A., Bezlepkina O.B., Vasyukova O. V., et al. Obesity in children: Clinical recommendations. Russian Association of Endocrinologists. Moscow: Ministry of Health of the Russian Federation, 2021.
14. Vasyukova O.V. Obesity in children and adolescents: diagnosis criteria. Obesity and metabolism. 2019;16(1):70-73. (In Russ.) https://doi.org/10.14341/omet10170
15. Vitebskaya A.V., Pisareva E.A., Popovich A.V. Lifestyle in children and adolescents with obesity: results of the survey of patients and their parents. Obesity and metabolism. 2016;13(2):33-40. (In Russ.) https://doi.org/10.14341/omet2016233-40
16. Vasyukova O.V., Okorokov P.L., Kasyanova Yu.V., Bezlepkina O.B. Energy exchange: how we can personalize obesity therapy. Problems of Endocrinology. 2021;67(5):4-10. https://doi.org/10.14341/probl12830
About the Authors
O. V. SkvortsovaRussian Federation
Olga V. Skvortsova - Pediatric endocrinologist, N.N. Ivanova Samara Regional Children's Clinical Hospital.
Samara
Competing Interests:
Authors declares no conflict of interest
N. B. Migacheva
Russian Federation
Natalia B. Migacheva - Dr. Sci. (Med.), Associate Professor, Head of the Department of Pediatrics, Institute of Professional Education, Samara State Medical University.
Samara
Competing Interests:
Authors declares no conflict of interest
E. G. Mikhaylova
Russian Federation
Evgeniya G. Mikhaylova - Cand. Sci. (Med.), Associate Professor of the Department of Pediatrics, Institute of Professional Education, Samara State Medical University, Director of the Department of Pediatric Endocrinology N.N. Ivanova Samara Regional Children's Clinical Hospital.
Samara
Competing Interests:
Authors declares no conflict of interest
L. I. Katkova
Russian Federation
Lyudmila I. Katkova - Dr. Sci. (Med.), Professor of Department of Pediatrics, Institute of Professional Education, Samara State Medical University.
Samara
Competing Interests:
Authors declares no conflict of interest
Review
For citations:
Skvortsova O.V., Migacheva N.B., Mikhaylova E.G., Katkova L.I. Assessment of the prevalence of overweight and obesity among school-age children in Samara. Medical Herald of the South of Russia. 2022;13(4):106-113. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-4-106-113







































