Scroll to:
Study of the role of etiological factors on the likelihood of organic personality disorder
https://doi.org/10.21886/2219-8075-2022-13-3-59-66
Abstract
Objective: to study the influence of etiological factors on the possibility of the formation of organic personality disorder. Materials and methods: 80 patients with organic personality disorder were examined. The control group was represented by 82 healthy volunteers. Research methods: anamnestic, clinical, and statistical. Results: it was established that heredity aggravated by mental illness, alcoholization and drug addiction of relatives of different kinship lines, perinatal pathology factors associated with the child, diseases suffered in childhood (infectious diseases, etc.), which resulted in severe outcomes in the early stages of treatment in the form of hospitalizations or other complications in the form of pneumonia, bronchitis, etc., convulsive conditions, traumatic brain injuries received in childhood, reveal a reliably significant probability for the occurrence of organic personality disorder. The effect factor of operative interventions performed under general anesthesia in childhood did not show a statistically significant effect. Conclusions: heredity, perinatal pathology, some diseases suffered in childhood, convulsive states and various types of traumatic brain injury significantly increase the likelihood of organic personality disorder.
Keywords
For citations:
Khudina J.S., Zaika V.G. Study of the role of etiological factors on the likelihood of organic personality disorder. Medical Herald of the South of Russia. 2022;13(3):59-66. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-3-59-66
Introduction
Along with the observed general decrease in mental disorders in Russia, there is an increase in the proportion of organic non-psychotic disorders, especially in young and old people [1–3]. The study of the causes of such a change in the structure of morbidity is performed in different directions; there are studies of the role of the predominance of neurosis-like symptoms, pathology of attractions, various affective disorders, often with a dysphoric component, as well as mild and moderate cognitive impairments in the clinical picture [4]. A combination of the mental disorders described above with psychopathic personality changes is often revealed, which greatly complicates diagnostic assessments and the contribution of individual components. Organic personality disorder (OPD), according to modern concepts (ICD-11), is regarded as a mild neurocognitive disorder (6D71) [5] accompanied by identified objective cognitive decline, which is a consequence of the underlying nervous system disorder (trauma, infection, intoxication, etc.). However, studies on the role of various etiological factors and their evident impact on the development of this pathology are few and scattered [6–8]. All of the above dictates the need to study the influence of various etiological factors on this pathology development.
This research was aimed at studying the impact of some etiological factors on the probability of OPD development.
Materials and methods
The examination of 162 people divided into two groups was performed. The main group (I) included 80 people (36 men, 44 women, the mean age was 31 ± 1.1 years) who applied to the psychiatric bureau-branches of the Federal State Institution "Main Bureau of Medical and Social Expertise for the Rostov Region" of the Ministry of Labor and Social Protection of the Russian Federation. The respondents were included in the main research group (I) according to the following criteria: 1) the diagnosis of "Personality disorder of organic etiology" (F07.0x, according to the ICD-10 diagnostic criteria) established and documented by a psychiatric hospital; 2) age from 18 to 44 years; 3) written informed consent to the research. Individuals with chronic personality changes induced by mental disorders were not included in the research.
The control group (II) included 82 healthy volunteers (34 men, 48 women, the mean age was 24±0.6 years). Inclusion criteria were the absence of signs of a mental disorder and a history of seeking psychiatric treatment, the age indicated above, and the presence of voluntary consent to the research.
The research methods included the following ones: anamnestic, clinical, and statistical.
The results were processed using the Microsoft Office Excel 2017 program, and the χ2 criterion was calculated using an electronic Internet calculator. The distribution was taken as different from normal. When analyzing the frequencies of characteristic values in groups, the χ2 test was used for four-field tables (2×2). In cases where the expected event was less than 10, the authors used the Yates chi-squared (χ2) test to compare the two groups. Differences were considered statistically significant at p <0.05.
Results
During the research, the following factors were considered:
- psychopathologically aggravated heredity, which included the presence of confirmed mental disorders in relatives, alcoholism and drug addiction, as well as specific personality traits of close relatives noted by respondents (excessive irritability, cruelty, strange behavior);
- perinatal pathology of the child (birth trauma, asphyxia, premature birth, hydrocephaly);
- severe childhood diseases of various etiologies resulting in hospitalizations in stationary healthcare facilities;
- convulsive conditions that have arisen against the background of intoxication of various etiologies (including febrile convulsions);
- traumatic brain injury received in childhood;
- surgeries in childhood performed under general anesthesia, or other intoxications that could cause brain hypoxia.
For the ease of further discussion of the results, a table reflecting the proportion (in %) of clinical and anamnestic characteristics in the main and control groups should be considered (Table 1).
Table 1
Clinical and anamnestic characteristics of the respondents
|
|
Main group (n=80) |
Control group (n=82) |
Statistical significance (p) 1,2 |
||||||
|
Male |
Female |
Total1 |
Male |
Female |
Total2 |
|
|||
|
Age, years |
29±1.7 |
33±1.3 |
31±1.1 |
25±1.1 |
24±0.1 |
24±0.6 |
|
||
|
Sex |
36 (45%) |
44 (55%) |
80 (100%) |
34 (41.5%) |
48 (58.5) |
82 (100%) |
|
||
|
Heredity |
24 (66.7%) |
26 (59.1%) |
50 (62.5%) |
2 (5.9%) |
8 (16.7%) |
10 (12.2%) |
p < 0.001 |
||
|
Childhood illnesses |
19 (52.8%) |
11 (25.0%) |
30 (37.5%) |
0 (0%) |
7 (14.6%) |
7 (8.5%) |
p < 0.001 |
||
|
Perinatal pathology |
15 (41.7%) |
14 (31.8%) |
29 (36.3%) |
2 (5.9%) |
9 (18.8%) |
11 (13.4%) |
p < 0.001 |
||
|
Traumatic brain injury |
13 (36.1%) |
11 (25.0%) |
24 (30.0%) |
5 (14.7%) |
6 (12.5%) |
11 (13.4%) |
p = 0.011 |
||
|
Convulsive conditions |
9 (25.0%) |
13 (29.5%) |
22 (27.5%) |
3 (8.8%) |
4 (8.3%) |
7 (8.5%) |
p = 0.002 |
||
|
Surgical interventions under general anesthesia |
4 (11.1%) |
3 (6.8%) |
7 (8.7%) |
2 (5.9%) |
2 (4.2%) |
4 (4.9%) |
p = 0.505 |
||
Burdened heredity turned out to be the most significant factor among the respondents of Group I and reached 62.5% of the total volume of the group. When compared within this group, there was a predominance of positive answers in the subgroup of women (26 women out of 44, which accounted for 59.1% of the gender sample). The number of positive answers in the subgroup of men turned out to be 24 out of 36 men, which amounted to 66.7% of the gender sample. When comparing within gender samples, it was revealed that the number of positive responses in women prevailed over the number of responses in men. However, statistical assessment (in %) demonstrated that the proportion of male respondents had an advantage of almost 8% (Table 1). Among the characteristics of this factor listed by the respondents, alcoholism was noted among the closest relatives (more often on the father’s side – grandfather, father, cousin; less often – on the mother's side; alcoholism of both parents occurred in episodic cases), as well as various mental disorders manifested by psychotic states, personality changes and intellectual defects, and specific personality traits, including irascibility, anger (Figure 1).
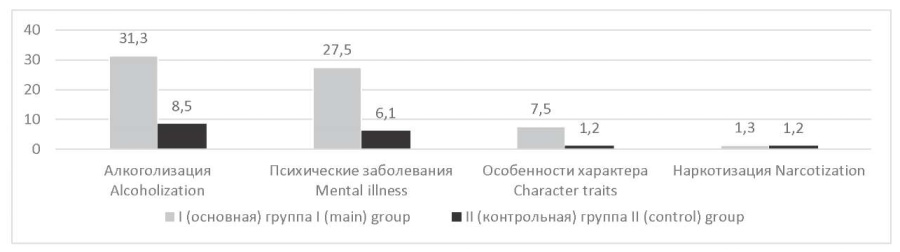
Figure 1. The role of the factor “Burdened heredity” in groups (in %).
In Group II, the factor "burdened heredity" was 12.2%, which was 5 times less than in Group I. When compared within this group, there was a predominance of positive answers in the subgroup of women (8 women out of 48, which amounted to 16.7%), while the number of positive answers among the subgroup of men was equal to 2 out of 34 men, which amounted to 5.9%. However, the statistical difference in this group between the proportion of women and men was almost 11% (Table 1). The factor was represented by the same characteristics as in the main group (Figure 1).
A detailed comparison of the "Burdened heredity" factor between groups allowed determining two predominant characteristics (alcoholism and mental disorders). The parameter "narcotization" in both groups was almost the same. The parameter "character traits" prevailed in Group I and needs to be further studied and more thoroughly analyzed (Figure 1).
Severe childhood illnesses in Group I were the second largest factor in the sample and were detected in more than a third of the respondents, which amounted to 37.5%. When compared within this group, there was a predominance of positive answers in the subgroup of men (19 men out of 36, which amounted to 52.8%), while the number of women was 11 out of 44 (25.0%). However, a statistical assessment (in %) demonstrated that the proportion of male respondents almost doubled (Table 1). As past diseases in Group I, in the vast majority of cases, infections of various etiologies were revealed. Frequent acute respiratory viral infections (ARVI) prevailed, which in almost all cases ended in hospitalizations due to complications such as pneumonia, bronchitis, etc. Infectious diseases such as mumps, rotavirus infection, whooping cough, salmonellosis, infection of unknown etiology, and meningitis turned out to be less significant. Further, the respondents indicated anemia and diseases of the gastrointestinal tract (dysbacteriosis, biliary dyskinesia). Toxic goiter, rickets, and lymphoblastic leukemia were indicated sporadically (Figure 2).
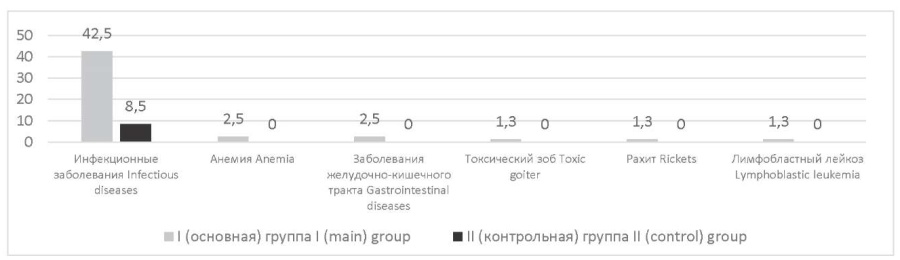
Figure 2. The role of the factor “Past diseases in childhood” in groups (in %).
In Group II, this factor was equal to 8.5%, which was almost 4.5 times less than in the main group. In addition, this factor was determined only in a subgroup of women (Table 1). Infectious diseases (ARVI, infectious mononucleosis) also prevailed as past diseases in Group II (Figure 2).
Perinatal pathology was in the third place in terms of significance in Group I and accounted for 36.3% of the total group. When compared within this group, there was a predominance of positive answers from a subgroup of men: 15 men out of 36 (41.7%); the number of women was 14 out of 44 (31.8%). However, a statistical assessment (in %) revealed that the proportion of male respondents in the general group had an advantage of almost 10% (Table 1). Among the characteristics of the factor listed by the respondents, asphyxia (due to tight entanglement by the umbilical cord and other reasons, including the use of resuscitation), the consequences of intrauterine infection (for example, in the form of sepsis or respiratory-affective-provoked seizures), as well as hydrocephaly were defined (Figure 3).
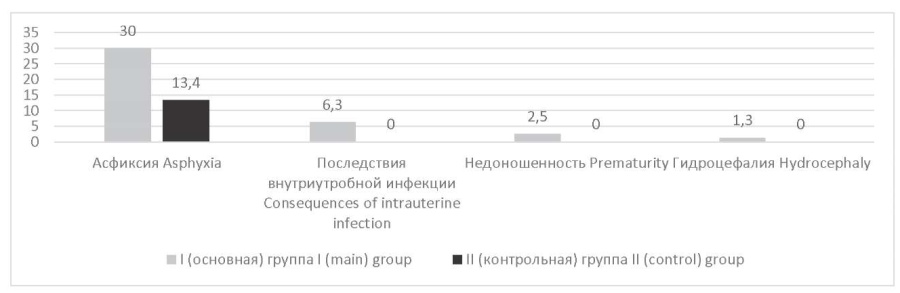
Figure 3. The role of the factor “Perinatal pathology” in groups (in %).
In the control group, this factor was one of the leading ones and amounted to 13.4%, and the subgroup of women prevailed over the subgroup of men: 9 women out of 48 (18.8%) and 2 men out of 34 (5.9%). However, the statistical difference in this group between the proportion of women and men was about 13% (Table 1). According to medical records, only asphyxia was recorded in this group (Figure 3).
Traumatic brain injuries received in childhood among the respondents of Group I amounted to 30.0%, becoming the fourth most important factor out of six studied in this research. When compared within this group, a subgroup of men prevailed: 13 men out of 36 (36.1%) and 11 women out of 44 (25.0%), while the statistical difference between the proportion of men and women was a little more than 11% (Table 1). Injuries received by the respondents of Group I could be divided into domestic (as a result of falls, fights, etc.) and injuries received in road accidents. One of the respondents noted several "sports" injuries (classes in the boxing section). In Group II, the factor "traumatic brain injury" was one of the leading factors and reached 13.4%. Within this group, a subgroup of women prevailed: 6 women out of 48 (12.5%) and 5 men out of 34 (14.7%). A statistical assessment (in %) revealed that the difference between the proportions of men and women turned out to be insignificant (Table 1). The characteristics of traumatic brain injuries in the main and control groups were the same.
Convulsive conditions were considered separately. For the main group, this figure was 27.5%. When compared within this group, a subgroup of women prevailed: 13 women out of 44 (29.5%) and 9 men out of 34 (25.0%), while the statistical difference between the proportion of men and women was about 5% (Table 1). Convulsive conditions in the main group were represented by major seizures and absences; febrile components of seizures predominated at the age of up to 3 years. In the control group, the “convulsive states” factor turned out to be 3 times less than in the main group and amounted to 8.5%. In this group, the number of women slightly prevailed: 4 women out of 48 (8.3%) and 3 men out of 34 (8.8%). A statistical assessment (in %) showed that the difference between the proportions of men and women turned out to be insignificant (Table 1). The characteristics of convulsive states practically did not differ in the main and control groups.
Surgical interventions in childhood in the respondents of the main group happened to be the smallest factor in terms of the frequency of detection and were confirmed in 8.7%. When compared within the main group, a subgroup of men prevailed: 4 men out of 36 (11.1%) and 3 women out of 44 (6.8%), while the statistical difference between the proportion of men and women was about 5% (Table 1). The "Surgical interventions" factor was represented by appendectomy, cleft lip and cleft palate surgeries, scleroplasty operations, correction of flat-valgus feet, skin graft surgeries due to body burns, and adenotomy. In Group II, this factor was equal to 4.9% (this was almost 2 times less than in the main group). When compared within this group, a subgroup of men and a subgroup of women gave the same number of answers (2 respondents of each gender), while the statistical difference between the proportion of men and women was a little more than 1% (Table 1).
Discussion
The performed statistical analysis revealed a high degree of reliability of some of the factors described above, which generally confirmed the opinion about the impact of these factors on the probability of OPD development. The heredity factor was a key risk factor for the probability of developing the studied pathology in comparison with all the others, which was consistent with other studies [9–11].
In the second place in terms of significance in this research was the factor of childhood diseases often followed by complications and hospitalizations. Many studies consider this fact as insufficiently developed and taking into account mainly early brain lesions [12].
The influence of perinatal pathology was in the third place in terms of significance in this research. However, according to the studied literature, active research is performed in the framework of the interpretation of mental and neurological disorders in the early stages of a child's life for the possibility of early prevention of diseases [13–16].
Convulsive seizures were next in terms of statistical significance. Despite the fact that these conditions are often encountered in the practice of pediatricians, neurologists, and epileptologists [17–19], in psychiatry, the influence of convulsive conditions on OPD occurrence is more often described in fundamental reference books than in modern articles [20].
During the analysis of samples, traumatic brain injuries received in childhood were also characterized by reliable statistical values. It should be noted that in the literature of the last few decades, the factor of influence of traumatic brain injury is the most frequently studied [21][22].
The results regarding surgeries performed under general anesthesia were as follows: in this research, in the control group, there was an increase of 3.0% of respondents who underwent this factor, in contrast to the main group. Despite the few available data on the impact of general anesthesia on the psyche [23], significant evidence of its impact on the probability of OPD development was not revealed during this research [24].
Therefore, psychopathologically aggravated heredity, childhood diseases of various etiologies followed by hospitalization in stationary healthcare facilities or other severe outcomes and complications, perinatal pathology, convulsive conditions that arose both autochthonously and against the background of intoxications of various etiologies, open and closed traumatic brain injuries received in childhood are negatively affecting the prognosis and can increase the risk of OPD development after 18 years of age (p < 0.001 or p < 0.05). This research has shown that the clinically unfavorable outcome of the factor "surgery in childhood performed under general anesthesia" did not demonstrate a statistically significant impact on the probability of OPD development.
Conclusion
It has been established that psychopathologically aggravated heredity, perinatal pathology, and a number of diseases, primarily childhood infectious diseases, convulsive conditions, and various types of traumatic brain injuries, significantly increase the probability of OPD development. This research did not reveal a statistically significant impact of general anesthesia during surgical interventions in childhood on the development of this pathology. It can be assumed that the data on a more significant role of anesthesia in children, available in the literature, were obtained when studying the influence of this factor with repeated exposure to anesthesia or without taking into account the possibility of a combined contribution of several etiological factors. The research results indicate the importance of studying the role of etiological factors when assessing the probability of OPD development.
References
1. Demcheva NK, Kekelidze ZI, Kazakovcev BA, et al. [Dynamics of the general and primary incidence of mental disorders in the population of the Russian Federation aged 60 and older in 2000-2016]. Rossiiskii psikhiatricheskii zhurnal [Russian Journal of Psychiatry]. 2017;(4):4-12. (In Russ.) eLIBRARY ID: 29823428
2. Yazdovskaya A.V., Demcheva N.K., Kazakovtsev B.A. Dynamics of incidence concerning mental disorders of non-psychotic character in the Russian Federation and federal districts in 1991-2017. Vestnik nevrologii, psihiatrii i nejrohirurgii. 2019;(3):16-26. (In Russ.) eLIBRARY ID: 37209046
3. Shishkina OA, Kachaeva MA, Kharitonova NK, Skibina NV, Nazarova LN. [Organic personality disorders in women (clinical, forensic psychiatric, biological and social aspects)]. Rossiiskii psikhiatricheskii zhurnal [Russian Journal of Psychiatry]. 2020;(3):74-86. (In Russ.) DOI: 10.24411/1560-957X-2020-10309
4. Vandysh-Bubko V.V. Organicheskoe psihicheskoe rasstrojstvo: sudebno-psihiatricheskij diagnoz. Nauchno-prakticheskaja konferencija s mezhdunarodnym uchastiem «Sudebnaja psihiatrija: sovremennye problemy teorii i praktiki (diagnostika, jekspertiza, profilaktika); Sentjabr 18-20, 2018; Moskva. (In Russ.) eLIBRARY ID: 36473622
5. MKB-11. Glava 06. Psihicheskie i povedencheskie rasstrojstva i narushenija nejropsihicheskogo razvitija. Statisticheskaja klassifikacija. M.: «KDU», «Universitetskaja kniga»; 2021. (In Russ.)
6. Shmakova OP, Mazaeva NA. Social adaptation of patients with organic mental disorders in childhood: the results of the long-term study. Zhurnal Nevrologii i Psikhiatrii imeni S.S. Korsakova. 2018;118(1):4‑12. (In Russ.). DOI: 10.17116/jnevro2018118114-12
7. Usyukina M.V., Kornilova S.V., Lavruschik M.V. Clinical-psychopathological features of organic personality disorder in connection with epilepsy. V.M. Bekhterev Rewiew of Psychiatry and Medical Psychology. 2018;(1):49-55. (In Russ.) eLIBRARY ID: 32850649
8. Hoehe MR, Morris-Rosendahl DJ. The role of genetics and genomics in clinical psychiatry. Dialogues Clin Neurosci. 2018;(3):169-177. DOI: 10.31887/DCNS.2018.20.3/mhoehe
9. Galstjan A.G. The role of heredity and environment in shaping human health. Jelektronnyj zhurnal «Sovremennye problemy nauki i obrazovanija». 2016;(4):232. (In Russ.). eLIBRARY ID: 26533023
10. Turabaeva A.M. Heredity and its impact on health. Mezhdunarodnaja nauchno-prakticheskaja konferencija studentov i aspirantov «Potencial Rossijskoj jekonomiki i innovacionnye produkty ego realizacii». 2019; 104-107. (In Russ.) eLIBRARY ID: 41000505
11. Evstropov V. M., Starchenko S. V., Klimov A. S. Faktory, vlijajushhie na zdorov'e cheloveka. Molodoj issledovatel' Dona. 2019;3(18). (In Russ.) Available at: https://cyberleninka.ru/article/n/faktory-vliyayuschie-na-zdorovie-cheloveka. Accessed February 06, 2022.
12. Sycheva M.A., Sergeeva I.G., Tulupov A.A. Organicheskie porazhenija golovnogo mozga. Novosibirsk : RIC NGU, 2015. (In Russ.)
13. Faa G, Manchia M, Pintus R, Gerosa C, Marcialis MA, Fanos V. Fetal programming of neuropsychiatric disorders. Birth Defects Res C Embryo Today. 2016; 108(3):207-223. DOI: 10.1002/bdrc.21139.
14. O'Donnell KJ, Meaney MJ. Fetal Origins of Mental Health: The Developmental Origins of Health and Disease Hypothesis. Am J Psychiatry. 2017;174 (4):319-328. DOI: 10.1176/appi.ajp.2016.16020138.
15. Kosenko V.G., Kolomiec Je.A., Shpakov A.Je., Kolomiec D.N., Zaharova-Makogon Ja.A. Nosological groups of mental disorders in (pre)conscripts and their association with medico-social and clinical characteristics of persons with childhood history of the CNS problems. Social'naja i klinicheskaja psihiatrija. 2017;27(2):45-49. (In Russ.). eLIBRARY ID: 30026898
16. Amiri M, Lamballais S, Geenjaar E, Blanken LME, El Marroun H, et al. Environment-Wide Association Study (En WAS) of Prenatal and Perinatal Factors Associated With Autistic Traits: A Population-Based Study. Autism Res. 2020;13(9):1582-1600. DOI: 10.1002/aur.2372.
17. Olimov A.R., Sharipov A.M., Hakimov D.P. Relevance evaluation of risk factors of complications development of febrile convulsions in children. Universum: medicina i farmakologija. 2017:4(38):29-36. (In Russ.). eLIBRARY ID: 28928267
18. Leung AKC, Hon KL, Leung TNH. Febrile seizures: an overview. Drugs in Context 2018; 7: 212536. DOI: 10.7573/dic.212536
19. Belousova E.D. Febrile seizures: what pediatricians should know. Rossiyskiy Vestnik Perinatologii i Pediatrii (Russian Bulletin of Perinatology and Pediatrics). 2018;63(6):108-114. (In Russ.) DOI: 10.21508/1027-4065-2018-63-5-108-114
20. Malinina E.V., Zabozlaeva I.V., Sablina T.N., Kochkina A.A. Jepilepsija v tablicah i shemah. Cheljabinsk: Izd-vo: StandART, 2014. (In Russ.)
21. Kosenko V.G., Kolomiec Je.A., Shpakov A.Je., Kolomiec D.N. Clinical and social factors of mental health of persons of pre-conscription and conscription age with central nervous system lesions in early childhood. Kubanskij nauchnyj medicinskij vestnik. 2017;1(162):74-77. (In Russ.) eLIBRARY ID: 29141499
22. Semple B.D., Zamani A., Rayner G., Shultz S.R., Jones N.C. Affective, neurocognitive and psychosocial disorders associated with traumatic brain injury and post-traumatic epilehsy. Neurobiol Dis. 2019;123:27-41 DOI: 10.1016/j.nbd.2018.07.018
23. Ing С., Zaccariello M.J., Kirsch A.C., Li G., Warner D.O. GAS, PANDA, and MASK: Comment. Anesthesiology. 2020;132:1587–1588. DOI: 10.1097/ALN.0000000000003284
24. Khudina J.S., Zaika V.G. The effect of addiction on the level of labour adaptation in persons with organic personality disorder. ŠESTI HRVATSKO–RUSKI PSIHIJATRIJSKI KONGRES s međunarodnim sudjelovanjem. 2021. Available at: https://hidp.hr/wp-content/uploads/2021/09/KNJIGA-SAZETAKA-2021-za-web-1.pdf. Accessed February 06, 2022.
About the Authors
J. S. KhudinaRussian Federation
Julia S. Khudina - assistant of the Department of psychiatry, Rostov State Medical University.
Rostov-on-Don.
SPIN-код 3480-2540
Competing Interests:
None
V. G. Zaika
Russian Federation
Vladimir G. Zaika - Dr. Sci. (Med.), Professor, head of Department of psychiatry, Rostov State Medical University.
Rostov-on-Don.
SPIN-код: 5668-4714
Competing Interests:
None
Review
For citations:
Khudina J.S., Zaika V.G. Study of the role of etiological factors on the likelihood of organic personality disorder. Medical Herald of the South of Russia. 2022;13(3):59-66. (In Russ.) https://doi.org/10.21886/2219-8075-2022-13-3-59-66







































