Scroll to:
Comparison of the main parameters of 24-hour blood pressure monitoring in patients with hypertension and atherosclerotic lesions of the arteries of the lower extremities
https://doi.org/10.21886/2219-8075-2021-12-4-54-61
Abstract
Objective: To study the features of the parameters of 24-hour blood pressure monitoring (24h-BPM) in patients with hypertension and atherosclerosis of the arteries of the lower extremities (AALE).
Materials and Methods: A total of 120 patients with hypertension were divided into 3 groups: Group I consisted of 46 patients with hypertension and clinically manifested AALE; Group II included 39 patients with hypertension and asymptomatic AALE; Group III included 35 patients with hypertension without AALE. Laboratory and instrumental studies were performed, including 24h-BPM and ultrasound triplex scanning (USTS) of the arteries of the lower extremities. Statistical analysis was performed using Microsoft Office Excel 16 (2015, Microsoft, USA), Statistica 10.0 (StatSoft, USA), IBM SPSS Statistica 26.0 (IBM, USA).
Results: Higher values of systolic blood pressure (SBP) were revealed in Group I patients compared with Group III (P <0.05). Increased variability of daily average and daytime SBP were found in Group I patients (16 [13; 17] and 15.5 [12; 18] mm Hg), which significantly differed from those in Group III (P = 0.005). The patients of Group II showed higher values of diastolic blood pressure (DBP) compared with Group I (P <0.017). Higher values of pulse blood pressure (PBP) were found in Group I compared with Groups II and III (P = 0.001). In Group I, the normal type of 24-hour index of SBP was 2 times less common (P <0.017).
Conclusions: The clinical manifestation of AALE is associated with higher SBP and PBP values, SBP variability and lower DBP values, which indicates a higher risk of cardiovascular complications.
For citations:
Sementsova N.A., Chesnikova A.I., Terentyev V.P. Comparison of the main parameters of 24-hour blood pressure monitoring in patients with hypertension and atherosclerotic lesions of the arteries of the lower extremities. Medical Herald of the South of Russia. 2021;12(4):54-61. (In Russ.) https://doi.org/10.21886/2219-8075-2021-12-4-54-61
Introduction
Atherosclerosis is one of the most acute and important problems in modern healthcare because of its high medical and social significance [1]. Cardiovascular pathology associated with atherosclerosis remains the main cause of lethality in the majority of economically developed countries [2]. Russian Federation is a country with one of the highest rates of morbidity, disabilities, temporary loss of employability, and lethality associated with atherosclerosis [3]. Among men aged 35-75 years old, there are 1,447 cases of death from cardiovascular diseases per 100,000 people, which is 2-4 times higher than in the majority of other countries [4]. As a rule, atherosclerosis is the main reason for the development of ischemic heart disease and cerebrovascular disease, which primarily leads to the lesion of various arterial pools [5][6].
Arterial hypertension (AH) also significantly contributes to the development of cardiovascular pathology. According to the results of a large epidemiologic study ESSE-RF, the prevalence of AH increased to 44%, and by the year 2025, the number of people with essential hypertension will increase by 1.5 billion [7]. Increased AH is a risk factor for the development of myocardial infarction, stroke, ischemic heart disease, and chronic heart failure [8][9]. An upscale study “Multiple Risk Factor Intervention Trial” showed an association between AH and atherosclerotic lesions of various vascular pools [10].
One of the most acute problems of practical healthcare is a combination of AH and peripheral atherosclerosis. The identification of peculiarities of AH development in patients with associated atherosclerosis of the arteries of the lower extremities (AALE) is important for the optimization of therapy and reduction of the risks for cardiovascular complications.
The study aimed to study the features of the parameters of 24-hour blood pressure monitoring (24h-BPM) in patients with hypertension and atherosclerosis of the arteries of the lower extremities (AALE).
Materials and Methods
The study included 120 patients with AH. The mean age of patients was 62.1±3.12 years old. Al patients were comparable by the degree and duration of AH (р >0.05). The study did not include patients with acute coronary syndrome, acute cerebrovascular event, or transitory ischemic attack within the past six months, secondary (symptomatic) AH, decompensation of chronic heart failure, permanent atrial fibrillation, hemodynamically relevant structural heart defects, severe hepatic, and renal pathology. The study was conducted at the Rostov Regional Clinical Hospital.
Depending on the presence and degree of expression of AALE, all patients were divided into three main groups. The first group included 46 patients with AH and clinically manifested AALE, the mean age of patients was 61.7±5.5 years old. The second group included 39 patients with AH and symptomless AALE, the mean age was 63.8±8.1 years old. The third group included 35 patients with AH without AALE, the mean age was 60.8±8 years old.
Patients from all groups received antihypertensive therapy that included ACE inhibitors, Angiotensin II receptor antagonist (AIIRA), calcium channel blocking agents (CCB), beta-adrenergic blocking agents, and diuretics. In the majority of cases, the rate of prescription of various classes of drugs in the groups did not differ significantly. Despite the prescribed antihypertensive therapy, the target AH was not achieved in patients from all groups.
In the group of patients with AH and AALE, male patients prevailed (р <0.001). Among patients with AH and clinically manifested AALE, the number of smokers was statistically significant (61%) in comparison with patients with AH and symptomless AALE (31%, р=0.006) and patients with AH and without AALE (26%, р=0.002).
Clinical and anamnestic characteristics of patients from different groups are presented in Table 1.
Таблица / Table 1
Клинико-анамнестическая характеристика пациентов
Clinical and anamnestic characteristics of the patients
|
Группы Groups
Показатели Index |
I группа Group I (n=46) |
II группа Group II (n=39) |
III группа Group III (n=35)
|
р1 |
р2 |
р3 |
pmg |
|
|
Возраст, лет Age, years |
61,7 ±5,5 |
63,8 ± 8,1 |
60,8 ± 8 |
<0,014 |
0,04 |
0,27 |
0,03 |
|
|
Пол, (%) м/ж Sex, (%) m/f |
98/2 |
82/18 |
37/63 |
0,014 |
<0,001 |
<0,001 |
<0,001 |
|
|
Курение, (%) Smoking, (%) |
61 |
31 |
26 |
0,006 |
0,6 |
0,002 |
0,002 |
|
|
АГ, достигнутая степень, (%) Hypertension degree, (%)
|
1 |
22 |
31 |
34 |
0,3 |
0,7 |
0,2 |
0,3 |
|
2 |
39 |
36 |
34 |
0,76 |
0,88 |
0,65 |
0,67 |
|
|
3 |
39 |
33 |
32 |
0,58 |
0,86 |
0,47 |
0,55 |
|
|
Стаж АГ, лет Duration of hypertension, years
|
8,8±6,1 |
9,7±5,5 |
8,3±4,8 |
0,48 |
0,67 |
0,24 |
0,34 |
|
|
Стадия ГБ, (%) Stage of EH, (%) |
II |
- |
10 |
37 |
0,027 |
0,007 |
<0,001 |
<0,001 |
|
III |
100 |
90 |
63 |
|||||
|
ХИНК, стадия, (%) CILE, (%)
|
I |
- |
100 |
- |
- |
- |
- |
- |
|
II |
50 |
- |
- |
|||||
|
III |
13 |
- |
- |
|||||
|
IV |
10 |
- |
- |
|||||
ГБ — гипертоническая болезнь, ХИНК — хроническая ишемия нижних конечностей.
Note: differences are statistically significant at p <0,05, pmg — intergroup comparison, p1 — differences between Groups I and II, p2 – differences between Groups II and III, p3 – differences between Groups I and III, the post hoc analysis was performed with Bonferroni correction.
essential hypertension, CILE – chronic ischemia of lower extremities
All patients underwent laboratory and instrumental methods examination that included CBC, CUT, biochemical blood assay, ECG, and echocardioscopy.
A 24-hour blood pressure monitoring (24h-BPM) was performed with a portable device “BP Lab” (Nizhniy Novgorod, Russia). By the results of 24h-BPM, the authors analyzed the mean 24-hour systolic blood pressure (24-hour SBP); mean 24-hour diastolic blood pressure (24-hour DBP); mean 24-hour pulse blood pressure (24-hour PBP); daytime and nighttime SBP, DBP, and PBP; mean 24-hour, mean daytime, and mean nighttime parameters of SBP, DBP, and PBP variability; and the daily index.
The expression of atherosclerosis was evaluated by the results of triplex ultrasonography of the lower extremity arteries.
Statistical analysis was made using the software Microsoft Office Excel 16 (2015, Microsoft, USA), Statistica 10.0 (StatSoft, USA), and IBM SPSS Statistica 26.0 (IBM, USA). A comparative analysis for the evaluation of statistically significant differences of the quantitative data was made using parametric (Student’s t-test, ANOVA) and non-parametric (Mann-Whitney test, Kruskal-Wallis) tests. The difference was not statistically significant at р>0.05. The intergroup comparison was made using a Bonferroni-corrected post hoc analysis. The differences were statistically significant at р <0.017 when three groups were compared.
Results
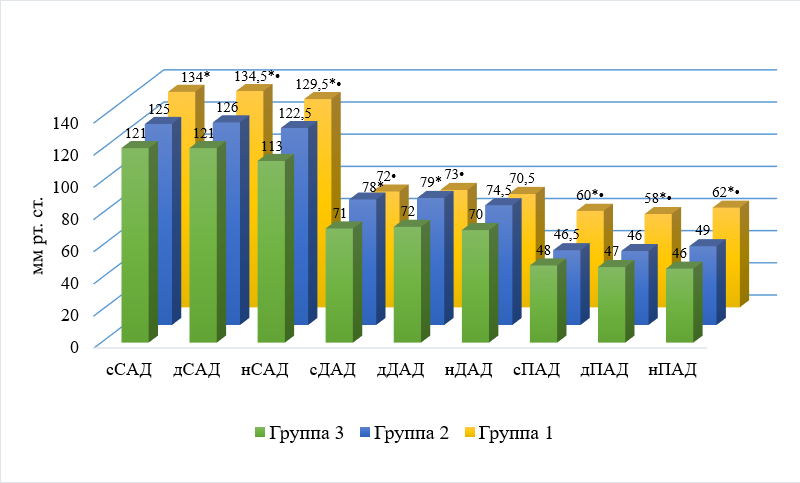
Comparative characteristic of the parameters of SBP, DBP, and PBP is presented in Fig. 1.
|
Russian |
English |
|
мм рт. ст. |
mmHg |
|
сСАД |
24-hour SBP |
|
дСАД |
daytime SBP |
|
нСАД |
nighttime SBP |
|
сДАД |
24-hour DBP |
|
дДАД |
daytime DBP |
|
нДАД |
nighttime DBP |
|
сПАД |
24-hour PBP |
|
дПАД |
daytime PBP |
|
нПАД |
nighttime PBP |
|
Группа 3 |
Group III |
|
Группа 2 |
Group II |
|
Группа 1 |
Group I |
Рисунок 1. Сравнительная характеристика показателей САД, ДАД и ПАД (мм рт. ст.)
Figure 1. Comparative characteristics of SBP, DBP and PBP (mmHg.)
Примечание: * — р<0,017 в сравнении с III группой, • — р <0,017 в сравнении со II группой. Апостериорный анализ проведен с поправкой на Бонферрони.
Note: * — P<0.017 comparison with Group III, • — P <0.017 comparison with Group II. The post hoc analysis was performed with Bonferroni correction.
The analysis of the obtained data showed a statistically significant (р=0.001) difference in 24-hour SBP (mmHg) in patients from Group I and III (134 [ 123;144] mmHg and 121 [ 113;127] mmHg, respectively). The difference was not statistically significant between patients from Groups I and III but there was an evident tendency to higher parameters in the group of patients with a classic manifested atherosclerotic lesion of lower extremity arteries (р=0.06). The analysis of the parameters of 24-hour DBP (mmHg) revealed significantly higher values in patients from Group II (78 [ 74;85] mmHg) than Group I (72 [ 68;79]) mmHg) and Group III (71 [ 67;78] mmHg).
It should be noted that the highest daytime and nighttime SBP values (mmHg) were registered in patients from Group I (134.5 [ 126;145] mmHg and 129.5 [ 120;147] mmHg, respectively) and the lowest values – in patients from Group III (121 [ 113;129] mmHg and 113 [ 109;129] mmHg, respectively). The obtained data indicate that the presence of the expressed atherosclerotic lesion of the lower extremity arteries aggravates the course of AH.
In patients from three groups, according to the average BP values proposed by the experts of the European Society of Hypertension, daytime DBP (mmHg) was classified as “normal” [11]. Along with that, nighttime DBP (mmHg) values exceeded the normal values in patients from Group II (74.5 [ 65.5;81] mmHg). The highest daytime DBP values were registered in patients from Group II (79 [ 73;86.5] mmHg) and the lowest – in patients from Group III (72 [ 67;79] mmHg).
The analysis of daytime and nighttime PBP values (mmHg) showed increased values (≥53 mmHg) in patients with AH and clinically manifested AALE (58 [ 52;70] mmHg and 62 [ 54;69] mmHg, respectively). The differences were statistically significant in comparison with patients from Groups II and III (р=0.001). The highest daytime PBP values (mmHg) were revealed in patients from Group I with AH and manifested AALE (60 [ 53;70] mmHg), they were significantly higher than in patients from Group II (46.5 [ 39;52.5] mmHg, р=0.001) and Group III (48 [ 38;57] mmHg, р=0.001).
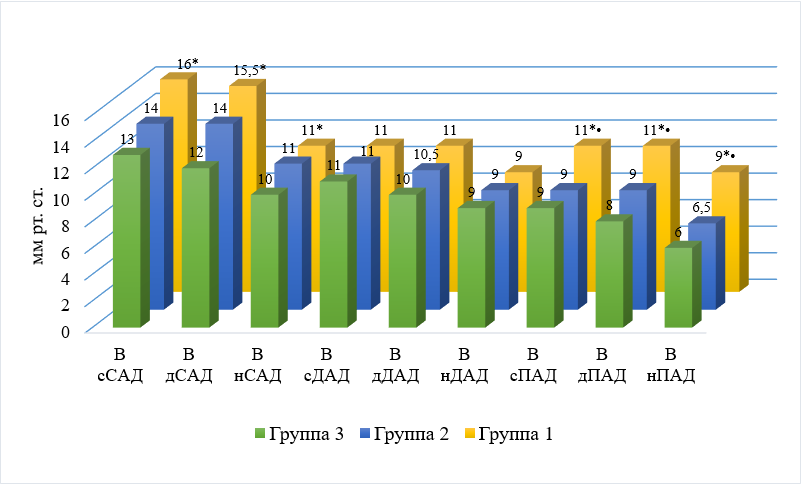
Comparative characteristics of the variability of SBP, DBP, and PBP are presented in Fig. 2.
|
Russian |
English |
|
мм рт. ст. |
mmHg |
|
В |
Variability |
|
сСАД |
24-hour SBP |
|
дСАД |
daytime SBP |
|
нСАД |
nighttime SBP |
|
сДАД |
24-hour DBP |
|
дДАД |
daytime DBP |
|
нДАД |
nighttime DBP |
|
сПАД |
24-hour PBP |
|
дПАД |
daytime PBP |
|
нПАД |
nighttime PBP |
|
Группа 3 |
Group III |
|
Группа 2 |
Group II |
|
Группа 1 |
Group I |
Рисунок 2. Сравнительная характеристика показателей вариабельности САД, ДАД и ПАД (мм рт. ст.)
Figure 2. Comparative characteristics of variability of SBP, DBP and PBP (mmHg.)
Примечание: * — р <0,017 в сравнении с III группой, • — р<0,017 в сравнении со 2-й группой. Апостериорный анализ проведен с поправкой на Бонферрони.
Note: * — P <0.017 comparison with Group III, • — P<0.017 comparison with Group II. The post hoc analysis was performed with Bonferroni correction.
The analysis of variabilities of 24-hour SBP and daytime SBP (mmHg) revealed increased values in comparison with the norm (>15 mmHg) in patients from Group III (13 [ 11;16] mmHg and 12 [ 10;15] mmHg, p=0.005). The variability of nighttime SBP, 24-hour DBP, daytime DBP, and nighttime DBP (mmHg) was within the norm in patients from three groups. The highest values of the variability of 24-hour PBP, daytime PBP, and nighttime PBP (mmHg) were registered in patients with AH and clinically manifested AALE (11 [9;15] mmHg, 11 [ 9;15] mmHg, and 9 [ 7;12] mmHg). They significantly exceeded the values registered in Group II (9 [ 7;10] mmHg, 9 [ 6;10] mmHg, and 6.5 [ 6;8.5] mmHg, р <0.017) and Group III (9 [ 7;11] mmHg, 8 [ 7;11] mmHg, and 6 [ 5;7] mmHg, р <0.017).
The distribution of patients according to the 24-hour index of SBP and DBP in each group is presented in Table 2.
Таблица / Table 2
Распределение пациентов с учетом СИ САД и ДАД в исследуемых группах
Distribution of patients according to 24-hour index of SBP and DBP in the 0study groups
|
Суточный индекс, абс. (%) 24-hour index, absolute number (%)
|
I группа Group I |
II группа Group II |
III группа Group III |
Уровень значимости Significance level |
||||
|
р1 |
р2 |
р3 |
рmg |
|||||
|
Dipper 10<СИ<20 10< 24-hour index <20 |
САД SBP |
15,2% |
38,5% |
42,8% |
0,045 |
0,7 |
0,016 |
0,013 |
|
ДАД DBP |
26,1% |
46,2% |
34,3% |
0,054 |
0,3 |
0,42 |
0,15 |
|
|
Non-dipper 0<СИ<10 0< 24-hour index <10 |
САД SBP |
41,3% |
35,9% |
28,6% |
0,6 |
0,23 |
0,23 |
0,4 |
|
ДАД DBP |
50% |
17,9% |
40% |
0,003 |
0,036 |
0,37 |
0,009 |
|
|
Over-dipper СИ> 20 24-hour index > 20 |
САД SBP |
2,2% |
2,5% |
2,9% |
0,9 |
0,8 |
0,9 |
0,9 |
|
ДАД DBP |
4,3% |
5,1% |
5,7% |
0,86 |
0,9 |
0,7 |
0,96 |
|
|
Night-peaker СИ <0 24-hour index <0 |
САД SBP |
41,3% |
23,1% |
25,7% |
0,075 |
0,79 |
0,14 |
0,1 |
|
ДАД DBP |
19,6% |
30,8% |
20% |
0,13 |
0,19 |
0,96 |
0,41 |
|
Note: differences are statistically significant at P <0.05; pmg — intergroup comparison, p1 — differences between Groups I and II, p2 — differences between Groups II and III, p3 — differences between Groups I and III; the post hoc analysis was performed with Bonferroni correction.
The analysis of the 24-hour index of SBP (%) showed that there were significantly fewer patients with a normal type of a 24-hour BP profile (“dipper” type) among patients with AH and clinically manifested AALE (15.2%) than in patients from Group II (38.5%, р=0.045) and Group III (42.8%, р=0.016).
The study of the 24-hour index of DAD (%) demonstrated the highest occurrence rate of a pathological 24-hour profile (“non-dipper” type) in patients from Group I in comparison with patients from Group III (50% and 17.9%, respectively, р=0.003).
The majority of researchers consider peripheral atherosclerosis to be a significant factor in the development of elevated BP in patients with AH [12]. According to the Trans-Atlantic Inter-Society Consensus scientists, AH increases the risk of the development of peripheral atherosclerosis in men by 2.5 times, and in women – by 3.9 times [13].
Atherosclerotic lesion of any vessels stimulates the progression of AH, while AH potentiates the development of atherosclerosis and accelerates its outcome [14].
An increase in BP is associated with chronic tension of an arterial wall with early dystrophic alterations, which can aggravate the progression of the atherosclerotic process from the destabilization of a plaque to the development of generalized atherothrombosis.
In the present study, the analysis of 24-hour BPM showed that the highest SBP values were registered in patients with AH and manifested AALE, which could be caused by the impairment of damping and transport functions of the arteries because of significant atherosclerotic lesion of vascular walls.
Higher values of 24-hour DBP and daytime DBP in patients with AH and symptomless peripheral atherosclerosis in comparison with these parameters in patients with AH and symptomless AALE could be associated with a more expressed increase in the peripheral vascular resistance. At the same time, according to the published data, in patients with the manifested atherosclerotic process, DBP tends to decrease because of impairments in the amortizing function of elastic vessels and a shift of the reflected pulse wave from the diastolic to early systolic phase [15], which was also demonstrated in the present study. Patients with AH and clinically manifested AALE had lower values of DBP in comparison with patients with a symptomless course of peripheral atherosclerosis.
High PBP, revealed in patients with AH and clinically manifested AALE, can indicate a significant increase in the stiffness of a vascular wall associated with manifested atherosclerosis, which is known to be the main mechanism of PBP increase and a predictor of high cardiovascular risk.
Higher values of the variability of SBP in patients from Group I also indicated a higher risk of cardiovascular complications in patients with AH and manifested AALE.
The analysis of a 24-hour index demonstrated that in patients with AH and clinically manifested AALE, a normal type of a 24-hour SBP profile “dipper” was registered rarer. Elevated nighttime SBP and an insufficient decrease in DBP were observed more frequently. Along with this, patients with symptomless AALE tended to have increased nighttime DBP (“night-peaker”).
Conclusion
AH and AALE are associated pathologies that aggravate each other’s development. Clinical manifestations of atherosclerotic alterations in the lower extremity vessels are reflected by higher values of a 24-hour, daytime, and nighttime SBP and PBP, variability of SBP, and lower values of 24-hour and daytime DBP. The revealed alterations indicate a higher risk for cardiovascular complications in patients with AH and associated clinically manifested AALE.
References
1. Akhmedov V.A., Shevchenko A. S., Isaeva A. S. Current view on the atherosclerosis emergence and progression factors. RMJ. Medical Review. 2019; 3(1-2):57–62. (In Russ.). eLIBRARY ID: 38165738
2. Sergienko S.V., Ansheles A.A., Kukharchuk V.V. Atherosclerosis and dyslipidemia: modern aspects of pathogenesis, diagnosis and treatment. M.: Patiss; 2017 (in Russ.). eLIBRARY ID: 27631153
3. Ezhov M. V., Sergienko I. V., Aronov D. M., Arabidze G. G., Akhmedzhanov N. M. et al. Diagnostics and correction of lipid metabolism disorders for prevention and treatment of atherosclerosis. Revision VI. Atherosclerosis and dyslipidemia. 2017; 3(28):5-22. (In Russ.). eLIBRARY ID: 29667695
4. Yao X, Yan C, Zhang L, Li Y, Wan Q. LncRNA ENST00113 promotes proliferation, survival, and migration by activating PI3K/Akt/mTOR signaling pathway in atherosclerosis. Medicine (Baltimore). 2018; 97(16):e0473. DOI: 10.1097/MD.0000000000010473.
5. Roever L, Resende ES, Diniz ALD, Penha-Silva N, O’Connell JL, et al. Epicardial adipose tissue and carotid artery disease: Protocol for systematic review and meta-analysis. Medicine (Baltimore). 2018; 97(17):e0273. DOI: 10.1097/MD.0000000000010273.
6. Kim M, Kim M, Yoo HJ, Lee E, Chae JS, et al. A promoter variant of the APOA5 gene increases atherogenic LDL levels and arterial stiffness in hypertriglyceridemic patients. PLoS One. 2017; 12(12):e0186693. DOI: 10.1371/journal.pone.0186693.
7. Boytsov S.A., Balanova Yu.A., Shalnova S.A., Deev A. D., Artamonova G. V., et al. Arterial hypertension among individuals of 25–64 years old: prevalence, awareness, treatment and control. by the data from eccd. Cardiovascular Therapy and Prevention. 2014; 13(4):4-14. (In Russ.). DOI: 10.15829/1728-8800-2014-4-4-14.
8. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018; 36(10):1953-2041. DOI: 10.1097/HJH.0000000000001940.
9. Chazova I. E., Zhernakova Y. V. Diagnosis and treatment of arterial hypertension [Guidelines]. Systemic hypertension. 2019; 16(1):6-31. (In Russ.). DOI: 10.26442/2075082X.2019.1.190179.
10. Mortality after 16 years for participants randomized to the Multiple Risk Factor Intervention Trial. Circulation. 1996; 94(5):946-51. DOI: 10.1161/01.cir.94.5.946. Erratum in: Circulation. 1997; 95(3):760. PMID: 8790030.
11. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018; 39(33):3021-3104. DOI: 10.1093/eurheartj/ehy339. Erratum in: Eur Heart J. 2019; 40(5):475. PMID: 30165516.
12. Evsikov E.M., Vechorko V.I., Teplova N.V., Zhapueva M.H., Artamonova N.G. Factors and mechanisms of arterial hypertension development in patients with atherosclerosis of lower limb arteries. Cardiovascular Therapy and Prevention. 2019; 18(1):150-155. (In Russ.) DOI: 10.15829/1728-8800-2019-1-150-155
13. TASC Steering Committee, Jaff MR, White CJ, Hiatt WR, Fowkes GR, et al. An Update on Methods for Revascularization and Expansion of the TASC Lesion Classification to Include Below-the-Knee Arteries: A Supplement to the Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Endovasc Ther. 2015; 22(5):663-77. DOI: 10.1177/1526602815592206.
14. Tkachenko E.I., Petrash V.V., Oreshko L. S., Ilina L.V., Litaeva M.P. The risk factors of atherosclerosis development in ontogenesis. Modern problems of science and education. 2016;(6):192. (In Russ.). eLIBRARY ID: 27694999.
15. Vasyuk Yu.A., Ivanova S.V., Shkolnik E.L., Kotovskaya Yu.V., Milyagin V.A., et al. Consensus of Russian experts on the evaluation of arterial stiffness in clinical practice. Cardiovascular Therapy and Prevention. 2016; 15(2):4-19. (In Russ.) DOI: 10.15829/1728-8800-2016-2-4-19
About the Authors
N. A. SementsovaRussian Federation
Nadezda A. Sementsova, PhD student of Department of internal medicine №1
Rostov-on-Don
A. I. Chesnikova
Russian Federation
Anna I. Chesnikova, Dr. Sci. (Med.), Professor, professor of Department of internal medicine №1
Rostov-on-Don
V. P. Terentyev
Russian Federation
Vladimir P. Terentyev, Dr. Sci. (Med.), Professor, head of the department of internal medicine №1
Rostov-on-Don
Review
For citations:
Sementsova N.A., Chesnikova A.I., Terentyev V.P. Comparison of the main parameters of 24-hour blood pressure monitoring in patients with hypertension and atherosclerotic lesions of the arteries of the lower extremities. Medical Herald of the South of Russia. 2021;12(4):54-61. (In Russ.) https://doi.org/10.21886/2219-8075-2021-12-4-54-61







































