Scroll to:
Manifestation of electrocardiographic signs of the Brugadа syndrome in the setting of therapy with class Ic antiarrhythmic drug Ethacizine
https://doi.org/10.21886/2219-8075-2021-12-4-62-66
Abstract
The article presents a clinical case of a patient presenting with electrocardiographic signs of the Brugada syndrome in the setting of therapy with class Ic antiarrhythmic drug Ethacizine. The special feature of this case is a complete disappearance of ECG signs of the Brugada syndrome and the normalization of ECG after withdrawal of the drug. For a functional diagnostiсian, it is important to pay timely attention to the Brugada pattern on the ECG and consider such changes not only in connection with subepicardial ischemia and possible myocardial damage.
For citations:
Sazonova Yu.N. Manifestation of electrocardiographic signs of the Brugadа syndrome in the setting of therapy with class Ic antiarrhythmic drug Ethacizine. Medical Herald of the South of Russia. 2021;12(4):62-66. (In Russ.) https://doi.org/10.21886/2219-8075-2021-12-4-62-66
Introduction
Brugada syndrome (BS) is one of the diseases with a high risk of sudden cardiac death (SCD) at a young age1. The main diagnostic manifestation of BS is the formation of a typical ECG pattern in the right precordial deflections (V1-V3), sometimes, in combination with the right His bundle branch block (RBBB). The peculiarity of BS is in a typical ECG pattern that underlies the diagnosis. It frequently has a transitory character or is identified before the development of life-threatening arrhythmias. It is induced by pharmacological drugs or physical factors (hyperthermia). In the present study, the author described a clinical case of BS (1 type ECG) associated with antiarrhythmic therapy with Ethacizine (Ic class).
Syncopal patients with I type spontaneous ECG should be included in a group of potentially high risk and non-syncopal patients with I type spontaneous ECG – in a group of intermediate risk.
Clinical monitoring of the rate of spontaneous ST-segment elevation and alterations of its morphology is feasible in both patients with clinical manifestations and without them as well as in closest relatives. Especially, it is true for the cases when ST-segment elevation develops only as a result of provoking pharmaceutical tests or antiarrhythmic drug administration1.
Clinical case
Patient K., female, 61 years old, applied to a hospital on 31.10.2019 with complaints of the feeling of heart work interruptions, dyspnea, sharp pain in the chest not associated with loads, and increased BP (150/90 mmHg, operating blood pressure 120/80).
Anamnesis. The patient has had these complaints since 2019. She takes the prescribed indap 2.5 mg/day, vamloset 5/160 mg/day, livazo 2 mg/day, and Ethasizine 50 mg 1/2 tab/TID. Chronic diseases include type 2 diabetes mellitus. According to the patient’s words, she had a paroxysm of ventricular tachycardia in the anamnesis. Burdened hereditary background: myocardial infarction (MI) in mother and ischemic heart disease (IHD) in farther.
Physical examination. Height – 170 cm, weight – 73 kg, BMI – 27, BP – 120/80 mmHg, HR 85 bpm, RR 18/min. The patient’s condition is satisfactory. The respiration is vesicular in all sections, without rales. The hear tones are muffed. CVA tenderness test is negative on both sides. Bowel and bladder functions are normal. The ankles are pasty.
Examination. An echocardiogram revealed aortal wall thickening, atherogenic index (AI), an increase in the myocardial mass, I degree left ventricular diastolic dysfunction (LVDD). ECG at rest showed sinus rhythm, HR 79 bpm, signs of left ventricular hypertrophy (LVH), PQ = 180 ms, QRS = 92 ms, QT = 400 ms. There were no pathological alterations in the ST-segment. Frequent ventricular extrasystoles (LBBB) were registered. Holter monitoring showed sinus rhythm, HR 43-87 bpm, and frequent ventricular extrasystoles (VE) 1134.
Ischemic heart disease (IHD). Arrhythmic variant. Heart rhythm disorders (HRD) as frequent VE. Lown grade IVa. III degree essential hypertension, stage 2, risk 4. Chronic heart failure (CHF) 2а functional class II. ICD-10 code: 20.8.
The following therapy was recommended to the patient:
- Indap 2.5 mg in the morning.
- Ethacizine 50 mg (1 tab) TID.
- Vamlocet 5/160 mg/day.
- Livazo 2 mg in the evening.
- Cardiomagnyl 75 mg in the morning.
- Omacor 1 drop/day, 1 month.
During the repeated application to the hospital on 14.11.2020, the patient continued complaining of the feeling of heart work interruptions and increased BP (170/90 mmHg, operating blood pressure 120/80). The patient takes indap 2.5, vamlocet 5/160 mg, livazo 2 mg, and Ethacizine 50 mg (1 tab.) TID.
Physical examination. Height – 170 cm, weight – 73 kg, BMI – 27, BP – 130/80 mmHg, HR 85 bpm, RR 18/min. The patient’s condition is satisfactory. The respiration is vesicular in all sections, without rales. The hear tones are muffed. CVA tenderness test is negative on both sides. Bowel and bladder functions are normal. No edemas were observed.
Examination: echocardiogram (14.11.2020) revealed LHV, I type LVDD, and ejection fraction (EF) 62%.
ECG (14.11.2020): sinus rhythm, HR 80 bpm. The electrical heart axis (QRS axis) is horizontal. ECG: sings of Brugada symptoms. Differentiation with focal alterations, subepicardial ischemia of the anteroseptal left ventricular area. Single VE. AV-block 1 degree, PQ = 276 ms, QRS = 180 ms, QT = 420 ms, QTc = 485 ms. ECG in dynamics and trop-test are recommended. During ECG, the patient did not complain of chest pain.

Рисунок 1. ЭКГ Пациент К., 62 г. Синдром Бругада.
Figure 1. EСG Patient K, male, 62 yr. Brugada syndrome.
ECG alterations correspond to I type Brugada syndrome (Fig. 1).
Holter monitoring (16.11.2020): sinus rhythm, HR 52 bpm, max 99 bpm. VE 44, including early. Lown-Wolf-Ryan grade V. Atrioventricular (AV) conduction disorder (QRS 180 ms). Transient ST-segment elevation to 2.5 mm. Intraventricular conduction disturbance. Manifested Brugada syndrome? (Fig. 2).

Рисунок 2. Холтер-ЭКГ. Пациент К., 62 г. Признаки синдрома Бругада. Частая ранняя вентрикулярная экстрасистолия.
Figure 2. Holter-ECG Patient K., male, 62 yr. Signs of Brugada syndrome. Frequent early ventricular extrasystole.
Ventricular extrasystoles are registered with a wide QRS complex as CBBB (possible arrhythmia localization is the right ventricle). An elongation of PR interval to 252 ms is observed. AV blockade of I degree, elongation of QRS to 0.172 s, and an increase in the interval QTs to 454 ms are registered. In the right precordial deflections (leads V1-V2), there is a coved elevation of ST-segment with a negative final part of T wave (ECG pattern typical for type I of Brugada syndrome) (Fig. 5).
Trop-test (14.11.2020) is negative.
IHD, arrhythmic variant. Heart rhythm disorder as frequent VE. Lown grade V. III degree hypertonic disease that reached 2 stage, risk 4. CHF 2a, FC 2. Manifested Brugada syndrome? ICD code: I 49.8».
The following therapy was recommended to the patient:
- Indap 2.5 mg in the morning.
- Vamlocet 10/160 mg/day.
- Preductal OD 1 tab/day, 3 months.
- Cordaron 200 mg, 1 tab BID, 10 days; further 1 tab/day 5 days/week.
- Rosuvastatin 10 mg in the evening.
- Clopidogrel 75 mg in the morning.
Bravadin 5 mg during the heartbeat. Physiotens 0.4 mg sublingual during BP elevation.
Ethacizine was withdrawn from therapy because of the appearance of signs of Brugada symptoms on ECG. The patient was switched to Cordaron 200 mg BID for 10 days, and further, 200 mg OD for 5 days/week (Saturday and Sundays – break).
ECG don 18.11.2020 (after Ethacisine withdrawal and an indication of Cordaron): sinus rhythm, HR 75 bpm. QRS is horizontal. Intraventricular conduction impairment, PQ = 190 ms, QRS = 100 ms, QT = 480 ms. In comparison with ECG dd 11.2020, there are no ECG signs of Brugada symptoms. Rhythm impairments are not registered (Fig. 3).
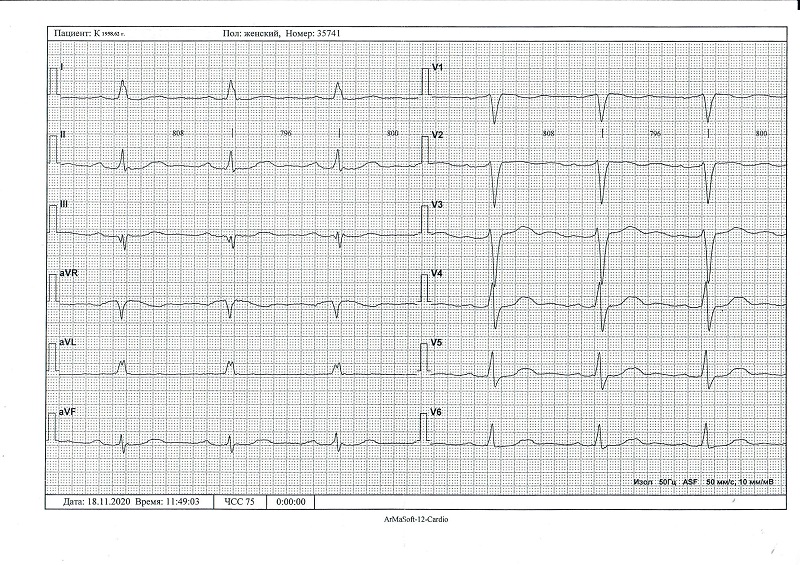
Рисунок 3. ЭКГ Пациент K.,62 г. После отмены этацизина.
Figure 3. ECG Patient K., male, 62 yr. After the Ethacizine withdrawal.
Holter monitoring (15.12.2020) after Ethacisine withdrawal: no ECG signs of Brugada syndrome (Fig. 4).
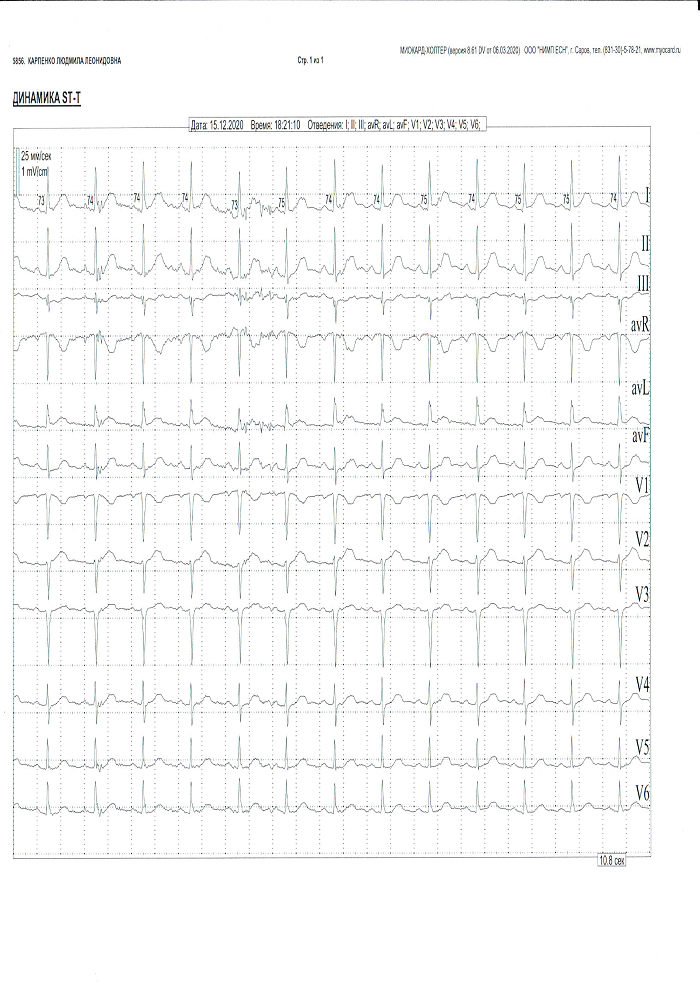
Рисунок 4. Пациент К.,62 г. Холтер-ЭКГ после отмены этацизина.
Figure 4. Patient K., male, 62 yr. Holter-ECG after Ethacizine withdrawal.
Discussion
BS is a heterogeneous genetic disease with a high risk of SCD [1]. The key element of BS pathogenesis is a genetically determined cardiomyocyte ion channel disorders associated with mutations in the gene SCN5A. The gene encodes the structure of α-subunits of cardiomyocyte sodium channels that provide rapid sodium currents in action potentials (I Na). The main diagnostic criteria of BS is a registration of a coved or “roof” ECG in two and more right precordial deflections (leads V1-V3) without the signs of ischemic alterations in discordant deflections. It has several types (Table 1, Fig. 5). Additional ECG signs include CBBB and periodical elongation of PR interval.
Taблица / Table 1
Диагностические критерии синдрома Бругада. Аномалии сегмента ST в отведениях V1–V3
Criteria for the diagnosis of Brugada Syndrome. ST segment anomalies in leads V1–V3
|
ЭКГ-изменения EСG Changes |
Тип 1 Type1 |
Тип2 Type2 |
Тип 3 Type3 |
Волна J J Wave |
>2 мм >2 mm |
>2 мм >2 mm |
>2 мм >2 mm |
|
Тип сегмента ST Type of ST segment |
Сводчатый Vaulted |
Седловидный Saddleback |
Седловидный Saddleback |
|
Конечная часть ST The final ST part |
Постоянно-отриц.(-) Constantly negative |
>1 мм >1 mm |
Подъём ST <1мм ST Elevation <1 mm |
|
Зубец T T Wave |
Отриц.(-) Negative ( -) |
+или +/- + or +/- |
+ + |
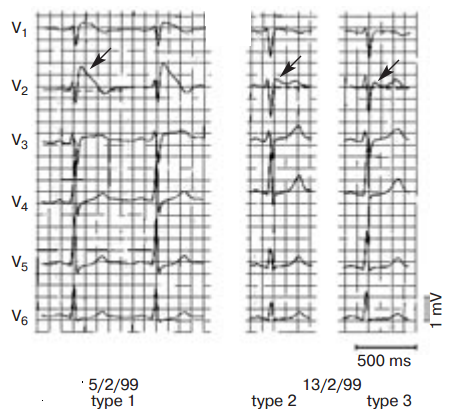
Рисунок 5. Типы синдрома Бругада.
Figure 5. Types of Brugada syndrome.
A typical ECG pattern of BS is inconsistent, which is different from the syndrome of long QT and other congenital arrhythmogenic channelopathies. Typical alterations in ECG are more expressed before ventricular fibrillation or right after it and can be induced by some pharmaceutical drugs. An official protocol of examination of patients with suspected BS, recommended by the working group of the European Society of Cardiology, includes tests with intravenous injection of I class antiarrhythmic drugs such as gilurytmal 1 mg/kg, procainamide 10 mg/kg, and flecainide 2 mg/kg (or 400 mg orally)1. Apart from drugs used for tests, there are some pharmacological drugs and chemical compounds that can cause Brugada-like alternations on ECG. A similar effect is described during the application of antiarrhythmic drugs of I class (sodium channel blockers: pilsicainide, propafenone, lidocaine), II class (β-adrenergic antagonist propranolol), IV class (calcium channel blockers verapamil, diltiazem), antianginal (nitrosorbide, isosorbide dinitrate, nicorandil), and psychotropic agents (tricyclic and tetracyclic antidepressants, serotonin reuptake inhibitors), antihistamine drugs (H1 antagonist dimenhydrinate), anesthetic agents (propofol, bupivacaine, methadone), as well as alcohol and cocaine intoxication.
Juntilla et al [2] observed 47 patients with induced BS patterns. In 16 patients, Brugada-like ECG type was induced by hyperthermia, and in 26 patients – by various drugs (antidepressant, antiarrhythmic, antihistamine, anesthetic, and other agents). In 24 (51%) out of 47 patients, there was malignant ventricular tachyarrhythmia; 18 patients (38%) had SCD or clinical death, 3 patients had syncope, and 3 patients had ventricular tachycardia. Nine patients received antiarrhythmic drugs (propafenone, flecainide, procainamide) for atrial fibrillation.
Type 1 Brugada-pattern on ECG associated with the administration of Ethacizine is not mentioned in the available published data. This is explained by the fact that this domestic drug of class IC is not used widely in foreign countries as Pilsicainide, which is primarily used in Japan [3]. Ethacizine is an effective and relatively safe drug of class IC, which is widely used as the first-line therapy in patients with idiopathic ventricular extrasystoles [3]. However, a similar case of the development of a clinical picture of BS in a 56-year-ol woman with ventricular extrasystoles associated with the administration of Ethacizine (also with a positive antiarrhythmic effect) was presented at the IX Congress of Russian Society of Holter Monitoring and Non-Invasive Electrophysiology (ROHMINE)2.
This shows that not all drugs that provoke manifestations of BS on ECG are well-known. However, there is another important question arises. How should drug-induced manifestations of BS be clinically interpreted? Drug-induced long QT is considered to be a secondary or acquired syndrome of long QT, which resolves after the withdrawal of the provoking factor. It is a reliable way to cope with life-threatening arrhythmias and does not indicate diagnosis “syndrome of long QT”. However, in patients with drug-induced BS, this approach is not used and the identification of a typical ECG pattern in not less than two right chest deflections after the introduction of therapeutic doses of procainamide, gilurytmal, or flecainide is sufficient for diagnosing BS [3].
At the same time, the appearance of BS pattern on ECG during the administration of other drugs (primarily class IC), that can also affect ECG, is not considered to be a valid method of diagnostic of latent BS. Molecular-genetic diagnostic is not a gold standard either in the diagnostic of BS (Table 2). Not all patients with typical clinical ECG pattern of BS have impaired sodium channels, which indicates the presence of molecular-genetic heterogeneity of this disease. In 25% of cases, the genetic background of the disease is not clear, in 15% of cases, patients lack typical family anamnesis, which can be a result of sporadic mutations [2]. Besides, molecular-genetic diagnostic is very expensive, which prevents its wide implementation.
Таблица / Table 2
Гены, ответственные за развитие синдрома Бругада
Genes associated with Brugada syndrome
|
Вариант LG-TS LQ-TS Variant |
Ген Gene |
ДНК-диагноститка в России DNA diagnostics in Russia |
|
ВrS 1 |
SCN5A |
Проводится (Conducted) |
|
ВrS 2 |
GPD1L |
Не проводистя ( not conducted) |
|
ВrS 3 |
CACNA2b |
Не проводистя ( not conducted) |
|
ВrS 4 |
CACNA2c |
Не проводистя ( not conducted) |
|
ВrS 5 |
SCN4B |
Проводится (Conducted) |
Besides, the author believes that all cases of drug-induced BS provide the necessity in the same approach as the results of pharmacological tests recommended by the working group of the European Society of Cardiology. After the verification of the diagnosis, it is feasible to stratify the risk based on the existing clinical, non-invasive, and invasive studies.
Conclusion
Oral administration of Ethacizine can provoke ECG alterations typical for BS.
During the application of Ethacizine as an antiarrhythmic agent, it is necessary to perform regular Holter monitoring and ECG at rest to exclude induced signs of BS and possible complications of this syndrome (ventricular rhythm disorders, ventricular tachycardia, high risk of SCD caused by polymorphic ventricular tachycardia or ventricular fibrillation).
ECG of Patient K. (Fig. 1) demonstrates I type Brugada pattern (Fig. 6).
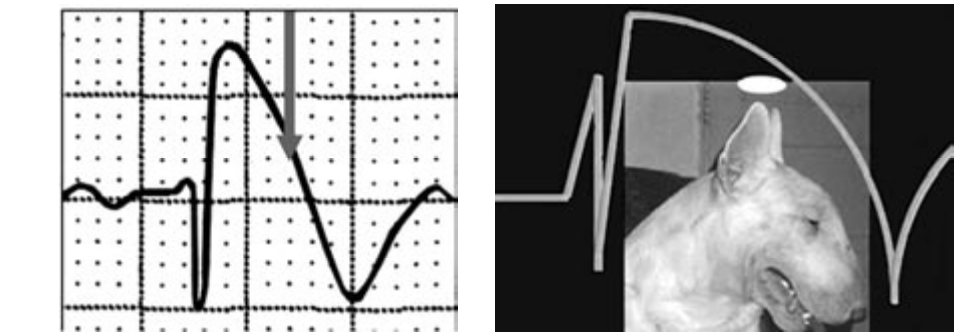
Рисунок 6. ЭКГ типа Бругада IA («тип бультерьера»).
Figure 6. Brugada IA type ECG (“bull terrier” type).
Verification of spontaneous I type Brugada pattern is associated with lower cumulative survival, doubled risk of arrhythmic events, and shorter time to the first arrhythmic event in comparison with drug-induced I type Brugada pattern on ECG. There are some difficulties in the verification of Brugada syndrome such as sporadic gene mutations and the high cost of the genetic assay.
The identification of I type Brugada pattern on ECG is an indication for examination and monitoring of the closest relatives of the patient even if they do not have cardiovascular diseases.
Patients with suspected Brugada syndrome that lack I type Brugada pattern on ECG are recommended provocation tests with class I antiarrhythmic drugs (AAD) (sodium channel blockers) for the differential diagnostic and verification of the diagnosis. In the Russian Federation, procainamide is available for this purpose (AAD Ia class, ATC code: C01BA02).
The application of Ethacizine as a drug for provocation tests in patients with suspected Brugada syndrome requires further studies.
1. Clinical recommendations for Brugada syndrome. Russian Association of Cardio-Vascular Surgeons. 2020. Available at https://racvs.ru/clinic/files/2020/brugada.pdf. Date of access: 09.09.2021
2. Tsygankova E.V., Donetskaya O.L., Goryukhina A.A. Changes in ECG associated with the administration of Ethacizine. Materials of IX Congress of Russian Society of Holter Monitoring and Non-Invasive Electrophysiology (ROHMINE) and II Congress “Clinical Electrocardiology”. 2008.
References
1. Ikeda T. Brugada syndrome: current clinical aspects and risk stratification. Ann Noninvasive Electrocardiol. 2002; 7(3):251- 62. DOI: 10.1111/j.1542-474x.2002.tb00172.x.
2. Junttila MJ, Gonzalez M, Lizotte E, Benito B, Vernooy K, et al. Induced Brugada-type electrocardiogram, a sign for imminent malignant arrhythmias. Circulation. 2008; 117(14):1890-3. DOI: 10.1161/CIRCULATIONAHA.107.746495.
3. Makarov L.M., Komolyatova V.N. Appearance of ECG signs of the Brugada syndrome during therapy with class 1C antiarrhythmic drug Ethacizine. Kardiologiia. 2011; 51(4):93-95. (In Russ.). eLIBRARY ID: 16606257
About the Author
Yu. N. SazonovaRussian Federation
Yuliуa N. Sazonova, functional diagnostician
Rostov-on-Don
Review
For citations:
Sazonova Yu.N. Manifestation of electrocardiographic signs of the Brugadа syndrome in the setting of therapy with class Ic antiarrhythmic drug Ethacizine. Medical Herald of the South of Russia. 2021;12(4):62-66. (In Russ.) https://doi.org/10.21886/2219-8075-2021-12-4-62-66







































