Scroll to:
Opportunities for predicting cesarean scar insufficiency
https://doi.org/10.21886/2219-8075-2021-12-1-54-61
Abstract
Objective. The study aimed to compare the diagnostic value of different methods of assessing the condition of the scar on the uterus after a cesarean section.
Materials and methods. A comparative analysis of the diagnostic value of assessing the validity of the scar on the uterus in the pre-graviridar period and during pregnancy ultrasound (ultrasound) investigation with dopplerometry (DM), magnetic resonance imaging (MRI), and microwave radiothermometry (RTM). The study included fertile patients after delivery by cesarean section (n = 56), at the planning stage, during pregnancy and after delivery, both through natural birth pathways and by re-cesarean section.
Results. A comparative analysis of the assessment of the scar in the uterus by the mentioned methods revealed the comparable diagnostic value of these methods during the planning phase of pregnancy and in gestation time 11–12 and 20 –21 weeks, while at the period of 37–38 weeks, the sensitivity of RTM was significantly (1.6 times) higher than ultrasound investigation.
Conclusions. Despite the high diagnostic effectiveness of all three methods of assessing the condition of the uterine scar after cesarean section, the method of microwave radiothermometry has advantages in the simplicity of the method, lack of need for expensive equipment, and specialized qualifications of the doctor.
Keywords
For citations:
Galustyan M.V., Kutsenko I.I., Borovikov I.O., Magay A.S. Opportunities for predicting cesarean scar insufficiency. Medical Herald of the South of Russia. 2021;12(1):54-61. https://doi.org/10.21886/2219-8075-2021-12-1-54-61
Introduction
In modern obstetrics, cesarean section is the most widespread assisted delivery surgery (in the Russian Federation, the rate is 15–16% on average, reaching 30-40% in 3rd-level obstetrics centers – perinatal centers) [1][2][3][4]. The number of extragenital pathologies and patients with burdened gynecologic-obstetrical anamnesis (especially, infertile patients after assisted reproductive treatment and age primipara, and patients with combined endocrine pathology) is increasing among the indications for cesarean section [4][5]. The above-mentioned factors contribute to an increase in the number of abdominal deliveries and contribute to the increase in women with a uterine scar, which is the main indication for the repeated cesarean section in nearly all countries [1][2][3][4]. At the same time, the number of complications during a repeated cesarean section increases by 3–4 times, which is more than 20% (5 times higher than after the first cesarean section [2][3][4]. A hysterectomy injury associated with operative delivery leads to a disturbance of intrauterine hemostasis and uterine drainage, which increases the rate of hemorrhagic and purulent-septic complications [5]. Besides, there are some unfavorable prognoses for complete recovery after abdominal delivery that include the increased risk of gynecological diseases (endometriosis, secondary infertility, syndrome of pelvic pains), subsequent obstetrical complications (ectopic pregnancy, premature delivery, fetal presentation, and placenta increta) [1][5][6][7].
The rationale for the present study is defined by the factors that can in the future provide possible vaginal delivery after assisted surgical delivery in the anamnesis, which requires the establishment of significant and reliable criteria for scar competence. Presently, obstetriciangynecologists have two opinions regarding conservative vaginal delivery in patients with a uterine scar. Some specialists believe that vaginal delivery in such patients contributes to a decrease in the rate of caesarian sections, and thus, the rate of associated complications [2]. Others highlight the impossibility to standardize the criteria of uterine scar competence, which will increase the rate of metrorrhexis along the scar [1][2]. Despite this diversity in opinions, presently, more and more clinical studies appear that focus on different methods of pregnancy and delivery management in women with a uterine scar that would provide successful vaginal delivery [4][5][6][7][8][9]. Even though there is a high rate of repeated abdominal deliveries at the majority of neonatal centers in Russia and the world, the so-called “careful approach” to the choice of the method of delivery in patients with a uterine scar, more and more institutions (primarily of the level III) practice vaginal delivery in such patients [10].
Primarily, the possibility of conservative delivery in women with a uterine scar after cesarean section is determined by the quality of the morphofunctional healing of the lower uterine segment, which requires the search for reliable methods of evaluation of uterine scar competence [11][12]. Presently, the most widespread method of the evaluation of the uterine scar is the ultrasonic investigation of the uterine scar in the pre-conceptional period and during pregnancy (evaluation of the thickness of the lower uterine segment, consistency of the myometrium in the scar area, acoustic density in the area of the former section). Besides, a complex examination of the uterine scar is becoming more popular before pregnancy (ultrasonography (US) with a contrasting agent, hysterography with contrasting agent, hysteroscopy, biopsy with further histological study, computed tomography (CT), and magnetic resonance imaging (MRI)) [11][12][13]. Even though the majority of these studies provide quite reliable information on the regeneration of the uterine scar, there are no precise criteria on the uterine scar competence evaluation and there is no objective algorithm for the determination of the possibility of vaginal delivery for such women.
Apart from clinical and anamnestic signs of the uterine scar incompetence, modern clinical recommendations include ultrasound investigation during pregnancy (indirect signs of the uterine scar incompetence include the thickness of the lower segment less than 2 and more than 5 mm, incompetence of the lower segment in the scar area (balloon-shaped, cone-shaped lower segment), the symptom of the “niche”, and increased acoustic density along the former section. Still, a decision on the uterine scar competence can be made intraoperatively only during cesarean section with its visual evaluation or after vaginal delivery (manual examination of the uterine cavity) [11][12][13].
The method of microwave radio thermometry (RTM), i.e. the measurement of the intensity of electromagnetic radiation of the human tissues in the range of super-high frequency for the evaluation of the uterine scar competence after a cesarean section is a new and promising method that has not been applied before in this area. A change in tissue temperature can be caused by inflammatory changes in the wounded tissues or their incompetence associated with the regeneration in this area. Besides, the absolute safety of RTM for patients and personnel should be noted. All the above-mentioned provides the rationale for the present study.
The study aimed to perform a comparison of the diagnostic value of different methods of evaluation of the uterine scar competence after abdominal delivery.
Materials and Methods
The studies were performed at the facilities of Kuban State Medical University of the Ministry of the Russian Federation at the Department of Obstetrics, Gynecology, and Perinatology (Head of the Department Prof. Kutsenko, PhD). A prospective, non-randomized study was performed at the perinatal center of Krasnodar Regional Clinical Hospital for Children (January 2018 – August 2019). The study included 56 fertile women who had abdominal delivery not later than 18 months before the study, were included in the study during the pre-conception period, and had a successful delivery. The examination was performed according to the Decree No. 572n dated November 12, 2012 of the Ministry of Healthcare of the Russian Federation. The study was approved by the local ethical committee Protocol No. 4 dated September 23, 2019.
Criteria of inclusion in the study:
- age 18 years old and older;
- one uterine scar after cesarean section in the lower uterine segment (the surgery was performed not later than 18 months before the study). The surgery was performed in the 37th week of pregnancy and later (single fetation). Uncomplicated post-operative period;
- lack of severe somatic pathology and malignant neoplasms;
- lack of other absolute and relative indications to abdominal delivery;
- signed form of informed consent for participation in the study.
Apart from a general clinical study (Decree No. 572n), the methods of instrumental diagnostics of the uterine scar competence after a cesarean section included transvaginal ultrasound scanning and power Doppler, MRI, and
microwave RTM. US criteria of uterine scar competence included the thickness of myometrium in the area of the lower uterine segment, typicality of the scar location, lack of deformities, “niches”, areas of retraction, lack of fibrous inclusions and liquid structures in the scar, blood feeding, and the condition of the retrouterine space. MRI criteria included the lack of local niche-like thinning of the myometrium.
The method of RTM (diagnostic complex RTM-01- RES, Russia) included the measurement of the internal myometrium temperature in the area of the uterine scar and the temperature of the skin and subcutaneous adipose tissue of the anterior abdominal wall. The study was performed in the supine position on a standard gynecological examination chair. The measurements were made in 3 points by a transabdominal sensor and in 3 points – by a transvaginal sensor. An antenna for receiving electromagnetic waves was applied to the studied point on the anterior abdominal wall and vaginally until the current temperature values were received. After the measurement of the internal temperature, the temperature was measured on the skin at the same points. The obtained results were analyzed. The RTM study of the myometrium in the area of the uterine scar revealed the most hypo- and hyperthermal areas along the scar, thermal asymmetry, and dispersion of the temperature. The results were presented as a graph (horizontal axis – points of measurements, vertical axis – temperature values) to evaluate the difference of temperatures in the area. To make a graphic image of a thermogram, a method of color visualization of thermal fields on the screen was used. The performed studies allowed the authors to identify the index of thermal asymmetry (ITA) as a ratio of hyper- and hypothermal areas of the myometrium. This method provides increased precision and objectivity of evaluation of the uterine scar competence. At the stage of studies, a great number of thermograms obtained from patients with cesarean section revealed 3 typical features that were formalized by the following factors:
1. Maximum temperature values in the area of the uterine scar in comparison with the average temperature tsc – tav, where tav = ∑6ti/6, ti — the temperature in 6 points (3 – transabdominal, 3 – transvaginal).
2. The mean quadratic difference of temperatures between the points in the uterine scar √∑6ti2/6 was compared in points 0…6.
3. Index of thermal asymmetry: ITA = (Tmax – Tmin); where Tmax is the maximum temperature in the uterine scar area, Tmin — the minimum temperature in the area of the uterine scar (3 transabdominal, 3 – transvaginal). When the ITA exceeds 0.9, this indicates an increased thermal asymmetry, which can be a sign of the uterine scar incompetence.
If the study is based on one parameter, the sensitivity of the method will be 60–75%. When all the features are considered, the sensitivity increases to 90% with the specificity not less than 85%.
The study design included 4 visits: visit 1 (preconception period) – informed consent, anamnesis, complex clinical study, evaluation of the uterine scar outside pregnancy (US, MRI, and RTM); visits 2, 3, and 4 (11th– 12th, 20th–21st, and 37th–38th week of pregnancy) – evaluation of the uterine scar during pregnancy (US and RTM); visit 5 (conservative/abdominal delivery) – visual and clinical evaluation of the uterine scar.
The obtained results were included in the statistical analysis with the calculation of the mean arithmetic value (M), the standard of the mean (m), and a statistically significant difference between the parameters (P) using the Student-Fisher test and Statistica 6.0.
Results
The study included 56 women aged 23–35 years old (mean age 28.3 ± 4.7 years old) who were examined and successfully delivered with one uterine scar after the cesarean section. The interval between the previous surgery
and the first visit was 22.4 ± 2.9 months. Anamnestic cesarean section was performed as a planned (11/56 – 19.6%) and urgent surgery (45/56 – 80.4%). The majority of operations were performed intranatally (31/56 – 55.4%). Anamnestic data on the previous operations were obtained from patients and delivery records from obstetrics centers. Primarily, these records did not contain the peculiarities of the surgery and post-operative period (43/56 – 76.8%). The collected anamnesis allowed the authors to reveal the peculiarities of previous pregnancies, indications to abdominal delivery, and the post-operative period. It was impossible to obtain the data on the method of the uterine section suturing and the used suturing material.
Discussion
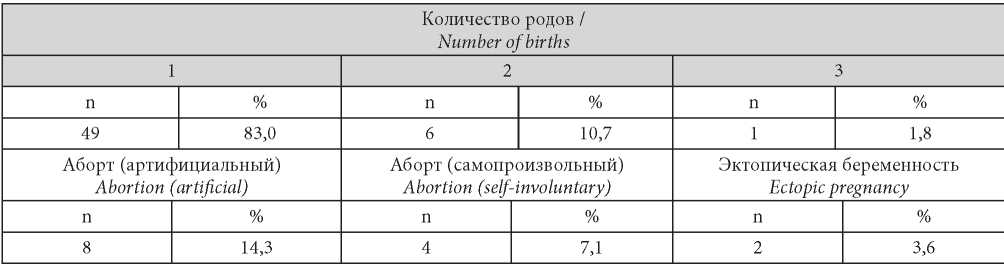
The mean age of the first pregnancy of patients was 21.4 ± 3.7 years old, the age of the first delivery was 26.1 ± 3.4 years old. Spontaneous miscarriage and missed miscarriage were registered in 7.1% (4/56) women, ectopic pregnancy was registered in 3.6% (2/56), which did not exceed the general population values. In the other parameters, there were no differences from the mean statistical values (Table 1).
Таблица / Table 1
Patient parity (n = 56)
Паритет пациенток (n = 56)
Indications for cesarean section in the patients were divided into the following groups (Letter of the Ministry of Healthcare of the Russian Federation dated May 6, 2014 No. 15-4/10/2-3190; Bezhenar, 2019) (Table 2):
Таблица / Table 2
Anamnestic evidence for abdominal delivery (n = 56)
Анамнестические показания к абдоминальному родоразрешению (n = 56)
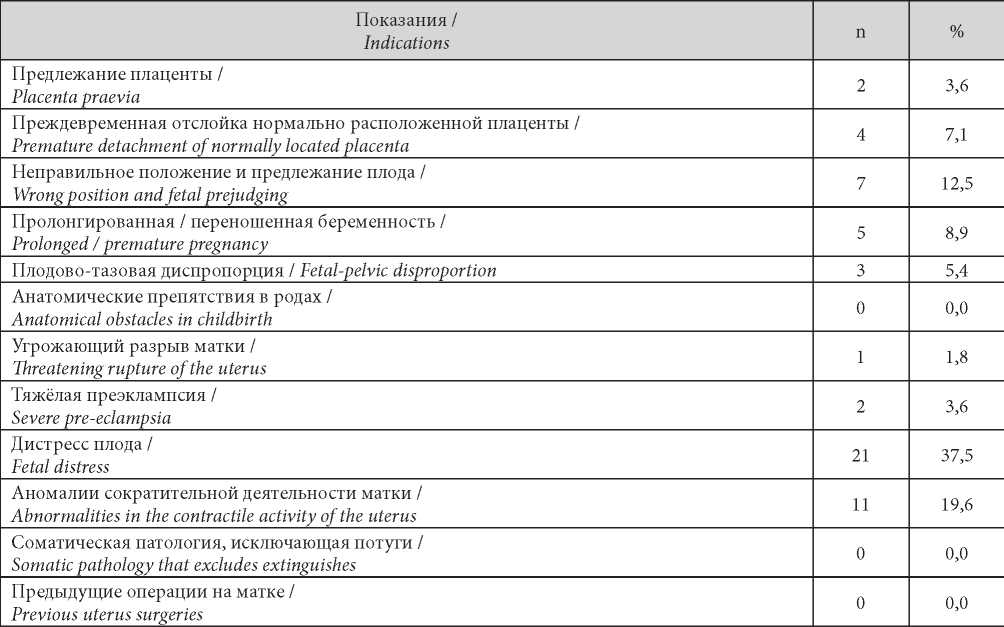
The most frequent indications for abdominal delivery were fetal distress in 37.5% (21/56) and abnormalities in the contractive activity of the uterus in 19.6% (11/56).
Ultrasound examination of patients in the preconception period showed the following results: the thickness of the uterine scar outside pregnancy ≥ 5.0 mm was revealed in 51/56 (91.1%) patients, the symptom of “niche” – in 2/56 (3.6%) women who planned pregnancy, increased acoustic density in the area of the former section — in 4/56 (7.1%) patients. MRI confirmed the obtained data. The thinning of the lower segment of the uterus < 4.3 mm was revealed in 5/56 (8.9%) women, the “niche” was confirmed in 2/56 (3.6%) patients. RTM revealed that the mean ITA in the studied group was 0.75 ± 0.13; in 4/56 women, it exceeded the threshold (mean value of ITA was 1.24 ± 0.41), which is an indirect sign of uterine scar incompetence (Figure 1).
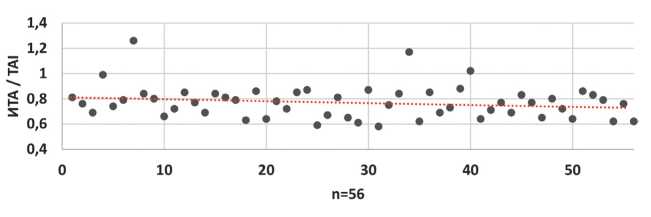
Рисунок 1. Индекс термоассиметрии пациенток (предгравидарная подготовка).
Figure 1. Patient thermoassymetry index (pre-gravity training).
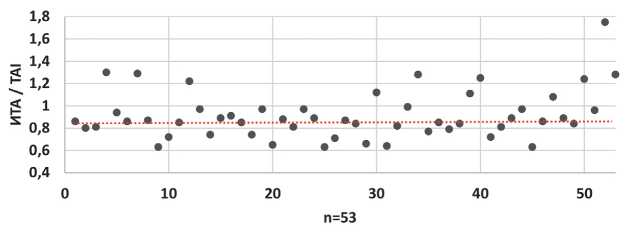
Рисунок 1. Индекс термоассиметрии пациенток (предгравидарная подготовка).
Figure 1. Patient thermoassymetry index (pre-gravity training).
A comparison of these three studies (US, MRI, and RTM) did not reveal any differences in their diagnostic value. The signs of the uterine scar incompetence (thinning of the lower segment, “niche”, thermal asymmetry) were detected in the same patients, four of them required further hysteroscopy for the verification of the diagnosis, three of them later underwent metroplasty, which was a criterion for the withdrawal from the study. The remaining 53 patients conceived with further embryo development within 34.2 ± 9.6 weeks after a pre-conception preparation. Taking into account that MRI during pregnancy is made only when medically strictly required, further comparison of the diagnostic value of methods was made between US and RTM in the screening dates (11th–12th and 20th–21st weeks) and full-term pregnancy (37th–38th weeks).
In weeks 11–12 of pregnancy, US of the lower uterine segment in 53 pregnant women revealed an average thickness of the scar 4.1 ± 0.8 mm (in 2/53 (3.8%) patients, the thickness of the scar was not less than 2.0 mm), the “niche” was not revealed in any patients. At this stage of pregnancy, the average ITA was 0.79 ± 0.14 (in 3/53 (5.7%) women, ITA was > 0.90). Despite indirect signs of thinning of the uterine wall in the area of the uterine scar in 2 patients and its inconsistency in 3 patients, the pregnancies were successfully preserved. The study performed in weeks 20–21 of pregnancy showed similar results: the mean thickness of the uterine scar was 3.8 ± 0.7 mm with the lack of “niches” in all the pregnant women. At this stage, the average ITA was 0.81 ± 0.17. Indirect signs of uterine scar incompetence were revealed in the same 3/53 (3.8%) patients.
In the case of full-term pregnancies (37–38 weeks), the results of the two methods of the study significantly differed. The mean thickness of the lower uterine segment in the area of the uterine scar in pregnant decreased by 2 times and was 2.3 ± 0.8 mm. At the same time, in 12/53 (22.6%) of patients, a thinning of the uterine scar was less than 2.0 mm, and in 5/53 (9.4%), a “niche” was revealed. The data obtained by RTM showed that at this stage of gestation, the mean ITA was 0.84 ± 0.16. Thermal asymmetry that exceeded the threshold values (0.9) was registered in 19/53 (35.8%) pregnant (Figure 2). In other words, at full-time pregnancy, RTM revealed indirect signs of uterine incompetence 1.6 times more often than US.
The next stage for all the patients was delivery. Abdominal delivery was observed in 41/53 (77.4%) patients. Out of them, the planned surgery was in 24/53 (45.3%) cases, the rest underwent antenatal (6/53 (11.3%)) and intranatal abdominal delivery (11/53 (20.7%)). The indications for the planned and urgent abdominal delivery are presented in Table 3.
Таблица / Table 3
Evidence for abdominal delivery (n = 41)
Показания к абдоминальному родоразрешению (n = 41)
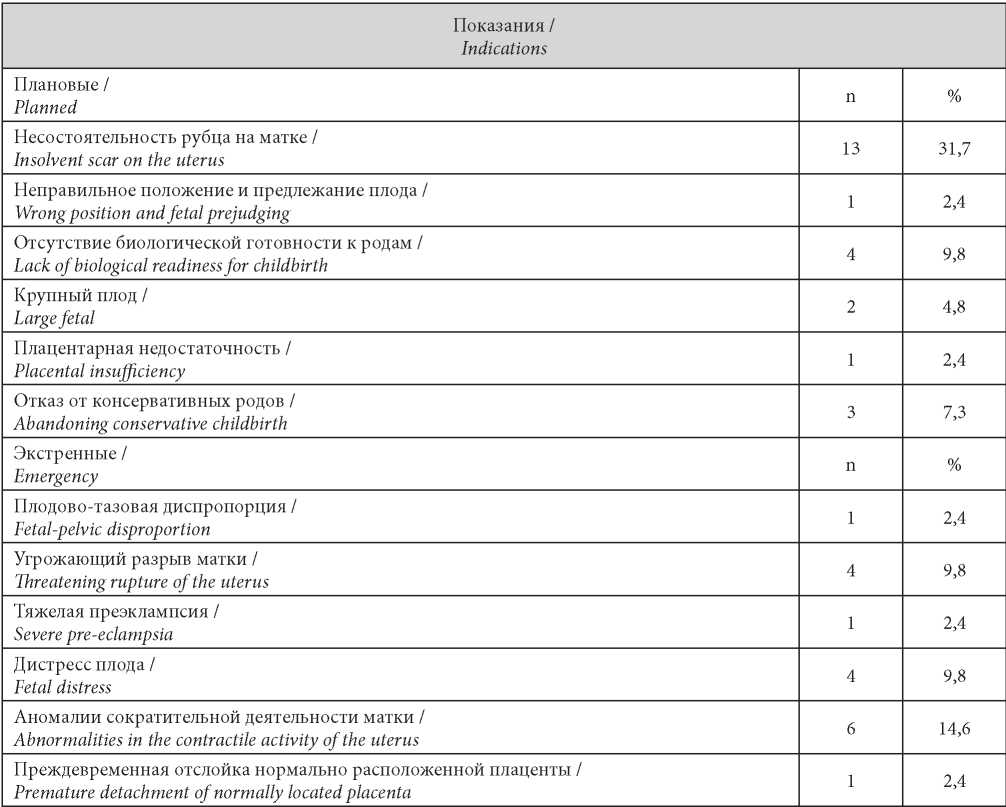
The most frequent indication for the planned abdominal delivery was the presence of clinical and functional signs of the uterine scar incompetence (13/53 (24.5%)). At the same time, intraoperatively, this diagnosis was confirmed in 100% of cases (thinning and defects of the muscular tissues in the area of the uterine tissue, which required metroplasty). Among urgent indications for cesarean section, there were abnormalities of contractive activity of the uterus (6/53 (11.3%)), threatening rupture of the uterus, and fetal distress 4/53 (7.5% each).
Besides, it should be mentioned that in 5/53 (9.4%) cases, the uterine scar incompetence was revealed during surgery, i.e. the number of incompetent uterine scars was 18/53 (34.0%).
Thus, the evaluation of the uterine scar competence in the pre-conception period by the three methods (US, MRI, and RTM) was comparable by sensitivity and specificity. In the case of full-time pregnancy, the evaluation of the uterine scar competence revealed a higher sensitivity of RTM diagnostics. Besides, this method does not require specific training and narrow specialization of a doctor (4- hour training). The apparatus is portable, compact, and economically more beneficial.
References
1. Mudrov V.A., Mochalova M.N., Mudrov A.A. Features of women’s vaginal delivery with uterine scar at present stage. Journal of Obstetrics and Women’s Diseases. 2018;67(1):26-37. (In Russ.). DOI: 10.17816/JOWD67126-37.
2. Zhukovskiy Y.G. C-section in the 21st century: new answers. Status Praesens. 2012;1(07):32-36. (In Russ.). eLIBRARY ID: 28340447
3. Kostin I.N., Lavrov A.Y., Knyazev S.A., Smirnova T.V., Kuznetsova O.A. Intranatal risk factors and neonatal outcomes. Herald RUDN. The series Medicine. 2010;(6):71-75. (In Russ.)
4. Wood S, Cooper S, Ross S. Does induction of labour increase the risk of caesarean section? A systematic review and metaanalysis of trials in women with intact membranes. BJOG. 2014;121(6):674-85; discussion 685. DOI: 10.1111/1471-0528.12328
5. Ananth CV, Vintzileos AM. Trends in cesarean delivery at preterm gestation and association with perinatal mortality. Am J Obstet Gynecol. 2011;204(6):505.e1-8. DOI: 10.1016/j.ajog.2011.01.062.
6. Martynov S.A. Cesarean scar defects: diagnosis and treatment in non-pregnant women. Gynecology. 2020;22(3):6-10. (In Russ.). DOI: 10.26442/20795696.2020.3.200189
7. Kesova M.I., Bolotova O.V., Kan N.Y., Ordjonikidze N.V. Prognostic criteria of the cesarean scar status appraisal. RUDN Journal of Medicine. 2009;(5):175-180. (In Russ.).
8. Shalashova Y.V. To the question of the psychological problems of women who have given birth by caesarean section. Siberian Journal of Psychology. 2001;(14-15):72-73. (In Russ.). eLIBRARY ID: 26002197
9. Menacker F, Declercq E, Macdorman MF. Cesarean delivery: background, trends, and epidemiology. Semin Perinatol. 2006;30(5):235-41. DOI: 10.1053/j.semperi.2006.07.002.
10. Gao L, Huang Z, Zhang X, Zhou N, Huang X, Wang X. Reproductive outcomes following cesarean scar pregnancy - a case series and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2016;200:102-7. DOI: 10.1016/j.ejogrb.2016.02.039
11. Nozhnitseva O.N., Semenov I.A., Bezhenar V.F. The scar on the uterus after cesarean section and the optimal algorithm for diagnostics. Diagnostic radiology and radiotherapy. 2019;(2):85-90. (In Russ.) DOI: 10.22328/2079-5343-2019-10-2-85-90
12. Setubal A, Alves J, Osório F, Guerra A, Fernandes R, et al. Treatment for Uterine Isthmocele, A Pouchlike Defect at the Site of a Cesarean Section Scar. J Minim Invasive Gynecol. 2018;25(1):38-46. DOI: 10.1016/j.jmig.2017.09.022
13. Nojinceva O.N., Bejenar V.F. The isthmocele of the scar on the uterus after the caesarean section is a new problem of a woman’s reproductive health. Journal of Obstetrics and Women’s Diseases. 2020;69(1):53-62. DOI: 10.17816/JOWD69153-62.
About the Authors
M. V. GalustyanRussian Federation
Marina V. Galustyan, graduate student of the Department of Obstetrics, Gynecology and Perinatology
Krasnodar
I. I. Kutsenko
Russian Federation
Irina I. Kutsenko, Dr. Sci. (Med.), Prof., Head of the Department of Obstetrics, Gynecology and Perinatology
Krasnodar
I. O. Borovikov
Russian Federation
Igor O. Borovikov, Dr. Sci. (Med.), As. Prof. of the Department of Obstetrics, Gynecology and Perinatology
Krasnodar
A. S. Magay
Russian Federation
Anton S. Magay, graduate student of the Department of Obstetrics, Gynecology and Perinatology
Krasnodar
Review
For citations:
Galustyan M.V., Kutsenko I.I., Borovikov I.O., Magay A.S. Opportunities for predicting cesarean scar insufficiency. Medical Herald of the South of Russia. 2021;12(1):54-61. https://doi.org/10.21886/2219-8075-2021-12-1-54-61







































