Перейти к:
Отмена препаратов в психиатрии: проблемы и возможности
https://doi.org/10.21886/2219-8075-2020-11-3-6-14
Аннотация
Многие рекомендации, протоколы описывают показания к началу приема лекарств, но только некоторые из них указывают, когда их приём следует прекратить. Анализ публикаций указывает на дефицит исследований в этой области, особенно в психиатрии. В рамках этого обзора мы постарались предоставить информацию, которая предоставляет ценную информацию об этой процедуре, об опыте других стран. На основании обзора литературы было установлено, что в некоторых странах уже существует консенсус в отношении того, как определить пациента, лечение которого может быть отменено, для этой процедуры были разработаны рекомендации и алгоритмы с минимальным риском для пациента.
Для цитирования:
Бибекова Ж.Б., Заровный К.В., Цыганова В.О. Отмена препаратов в психиатрии: проблемы и возможности. Медицинский вестник Юга России. 2020;11(3):6-14. https://doi.org/10.21886/2219-8075-2020-11-3-6-14
For citation:
Bibekova Zh.B., Zarovnyy K.V., Tsyganova V.O. Deprescribing in psychiatry: challenges and opportunities. Medical Herald of the South of Russia. 2020;11(3):6-14. https://doi.org/10.21886/2219-8075-2020-11-3-6-14
Deprescribing is the process of reducing or discontinuing medicines that are unnecessary or deemed to be harmful [1][2]. The goal of deprescribing is to reduce medication burden and harm, while maintaining or improving qualify of life [3]. Many guidelines describe the indications for treatment initiating, but only some of them give recommendation to stop therapy. The aim of the study was to present up-to-date information on deprescribing, its fields of application, and the experience of other countries.
Deprescribing is a proposed antidote to the harms of polypharmacy and is associated with numerous health benefits including improvement in cognition, a reduction in falls, a decrease in fractures, better medication adherence and improvement in qualify of life [1].
Deprescribing is an inherent component of good prescribing practice, but is rarely implemented in routine clinical care, and physician practice or views on deprescribing vary greatly [4][5][6]. It is important to recognize that deprescribing involves more than just identifying inappropriate medicine use [7]. It involves reviewing of all medical appointments, identifying un-necessary and potentially harmful drugs, deciding which of them can be stopped and setting the order of cancellation or change of dose, form of drug, with adequate monitoring for this. A deprescribing medication management plan is a final step of this process and should include discussion of changes with the patient and getting patient's consent.
Accordingly, the concept of deprescribing first arose in geriatric medicine. Recently, it has been mentioned that deprescribing is also associated with other medical specialties, including cardiology and psychiatry. The increase in potentially inadequate polypharmacy in child psychiatry (observed in many countries) without a clear improvement in functioning is just one reason to focus and stimulate the practice of a thoughtful withdrawal process [8][9].
The term deprescribing was used in the English language health literature in 2003 in an Australian hospital pharmacy journal in an article titled, «De-prescribing: achieving better health outcomes for older people through reducing medications» [10].
The literature from January 1, 2003 to March 30, 2020, was searched to identify published systematic reviews and metaanalyses that were relevant to the project. Search terms included Deprescribing, polypharmacy, suboptimal drug therapy, Deprescribing in psychiatry. Terms were searched alone and in combination. Search limits included human subjects, English language. Data sources for the initial search included PubMed, and references lists of selected articles that the panel.
The initial search identified 50 citations, of which 30 were selected for preliminary review. 20 were excluded for not meeting the study purpose or not containing primary data. An additional research was conducted with the supplementary terms such as antipsychotics and, geriatrics, and elderly prescribing. Previous searches were used to develop additional terms to be included in subsequent searches, such as a list of authors whose work was relevant to the goals of the project. When evidence was sparse on older medications, searches were conducted on drug class and individual medication names and included older search dates for these drugs. Additional articles were found in a manual search of the identified articles reference lists and the panelist's files, book chapter, and recent articles review.
Deprescribing is necessary in connection with the developing polypharmacy of the medical community, which is associated with the multimorbidity of patients, affecting more than 50% of people in primary care [11]. As a result, patients are often prescribed several drugs. In addition, old age and weakness contribute to a decrease in life expectancy [12]. Therefore, physicians often must balance a variety of factors, including the disease (s) the patient may have, the benefit-risk profile of the prescribed drugs, the personal views of the patients, and the opinions of other prescribers. Patients who visit four or more doctors experience problems, like a conflicting medical advice, because of which the number of drugs taken does not decrease [13].
Due to the stigma associated with mental illness, which is often heightened by news media coverage, and an initial treatment focus on remission, a patient's first impression of the psychiatrist may be that of a «pill pusher». Alternatively, a patient may desire to please the prescriber through continued adherence, which might also generate conflict regarding treatment [14]. Medicaid claims data have shown that psychotropic polypharmacy has risen consistently over the past two decades in various states [15][16]. Although certain combinations of psychotropics have been shown to be beneficial in «treatment resistant» psychiatric disorders, the stability of the treatment- resistant label over time is unknown. In fact, Stahl and Grady found in their review that most practitioners do not try to discontinue one of the drugs after a combination proves beneficial, even if cancellation is necessary [17].
Biological, psychological, and social factors must align to produce a favorable risk-benefit ratio such that a medication regimen becomes established for a patient. Over time, this risk- benefit ratio can change, providing an indication for deprescribing: certain adverse effects may develop only after longer-term use (for example, tardive dyskinesia with antipsychotics and renal impairment with lithium); normal aging alters both the pharmacodynamics and the kinetics of medications, increasing vulnerability to side effects; pregnancy; development of general medical comorbidities; new medication interactions; substance abuse raise. Psychological factors, such as patients' choice, their understanding of illness and medication, and their coping strategies, may evolve over time, shifting their individual risk-benefit ratio. Social factors, such as geographical relocation, changes in financial and insurance status, and changes in religion, may prompt a reappraisal. The growth of the recovery movement and patient-centered care in psychiatry, including in pharmacological management, further necessitates the development of deprescribing skills [14].
The imperfection of psychiatric classifications leads to the fact that in psychiatry (as in geriatrics) often several diagnoses can coexist in one patient. The practice of prescribing treatment «syndromically» is quite common, although international recommendations advise sticking to monotherapy. There are not so many combinations effectiveness of which would be confirmed by high-level studies. In the same way, the point of recommendations on the use of the lowest possible doses is not always followed: often the patient continues the therapy that was needed during the exacerbation, in spite of the fact that smaller doses are sufficient for maintenance therapy. Firstly, it is obvious, deprescribing is not suitable for all patients. This opportunity should be considered if: the patient is determined to participate in resolving issues about his treatment; the majority of the disorder symptom is currently absent; for this patient, unlikely behavior associated with a danger to themselves and others (auto- and hetero-aggressiveness), at the moment and for a long time there were no facts of drugs abuse; the social environment can support the patient, track changes in his condition; it is possible to turn to psychological therapy [18].
Secondly, to cancel drugs is the same science as to prescribe. There are only few studies that would specifically explore the cancellation process. A review of deprescribing processes in medical practice identified five key components: preparing a comprehensive medication history, identifying potentially inappropriate medications, determining whether a potentially inappropriate medication can be ceased, planning the withdrawal regimen (e.g. tapering where necessary), and provision of monitoring, support and documentation [19]. For use in psychiatry, this five-step process has been expanded to include appropriate timing, inclusion of the patient's family, friends and mental health team in the deprescribing process, and development of a plan for relapse identification, prevention and management (Table 1) [9][14][18].
Table 1
Steps of deprescribing in psychiatry
|
Step |
Purpose |
Implementation |
|
Assess the timing of the intervention |
To avoid initiating deprescribing at a time when the individual may be particularly vulnerable to a relapse, e.g. a period of psychosocial instability and/or heavy substance use, recent hospital admission |
Assess housing, employment, financial status, social relationships, impending changes in these, and substance use |
|
Review psychiatric and medication history |
To minimise chances of relapse or clinical risk during deprescribing |
Review psychiatric records, obtain history from the patient and available collateral sources Assess any previous trials of deprescribing/ attempts at reduction or discontinuation Contact other physicians involved in the patient's care and compile a complete medication list Document the dose, route, duration, indication, perceived benefit and side-effects for each medication |
|
Initiate the discussion about deprescribing |
To assess the patient's thoughts and feelings about deprescribing If appropriate (e.g. in antipsychotic polypharmacy) a hierarchy of medications with highest to lowest risk/ benefit ratio could be generated |
Assess the patient's learning style and check for understanding Explore preferences and values Explore current knowledge Explain risks and benefits Examine choices |
|
Involve the team and social supports |
If the patient agrees, to acknowledge and support them in their decision, help them maintain wellness, monitor for early signs of relapse and notify the care team if signs are noticed. With the patient's consent, all providers involved in care should be aware of the initiation of deprescribing, including visiting nurse services, therapists, case managers and primary care |
Consider a meeting with family, friends and other significant individuals Establish reliable means of contact, such as telephone or secure email Invite participation and contact from friends and family as desired by the patient |
|
Develop and initiate psychosocial interventions |
To help define, detect, and address any increase in symptoms To add supports to help the patient cope with anxiety, threats and challenges related to deprescribing |
Develop a relapse prevention plan such as WRAP Consider additional support through psychotherapy, potentially targeting specific symptoms Consider self-help and mutual support groups |
|
Develop and initiate the antipsychotic taper |
To reduce the dose in a controlled and conservative way, to minimize negative impact |
Decide which antipsychotic to taper Decide the rate of taper Adjust concomitant medications such as anticholinergics accordingly |
|
Monitor and adjust taper according to response |
To prevent, as much as possible, relapse or life disruptions due to the taper |
Monitor for early signs of relapse Monitor functioning Monitor metabolic and neurological side-effects Slow the rate of taper if needed Reverse the taper if needed |
Deprescribing hinges on effective relapse prevention. A biopsychosocial perspective on relapse prevention, for example, in schizophrenia highlights the significance of psychosocial stressors such as loss of employment or housing, bereavement or disruption of relationships. As well stressors of a biological nature such as substance misuse and, perhaps, precipitous, or ill- timed discontinuation of antipsychotics. They root deprescribing in psychiatry in recovery-oriented practices (Table 2), including shared decision-making, a person-centered approach and the nurturing of empowerment and hope [9][20][21][22][23].
Table 2
Recovery-oriented practices in mental healthcare and their application to deprescribing
|
Practice |
Description |
Application to deprescribing |
|
Shared decision-making |
A process of collaboration to arrive at a mutually acceptable treatment plan. It involves two experts: one who knows the scientific literature and has clinical experience, and one who knows their own preferences and subjective experiences |
Collaboration and solicitation of the patient's preferences and values at every step are essential components of deprescribing |
|
Person-centered care |
Designed to promote service engagement by increasing patient self-determination during treatment. It is defined as a highly individual comprehensive approach to assessment and services and is more focused on developing customized plans for achieving life goals rather than on symptom relief |
Deprescribing aims to increase patient engagement and participation in treatment. Person-centered care offers a framework in which individualized antipsychotic tapering plans as well as psychosocial supports are nested |
|
Hope |
Hope is the belief that recovery is possible. It involves the recognition and acceptance of the problem and a commitment to change |
With its emphasis on individual goals and preferences, deprescribing is based on hope and, by its nature, instils hope |
|
Empowerment |
Empowerment may be viewed as a corrective for the helplessness and lack of control that an individual may face in the mental health system. It includes autonomy, courage and responsibility |
Deprescribing empowers the individual by encouraging them to take charge of their treatment and providing the space for them to take risks, should they choose to do so |
Consider the clinical situations in psychiatry in which deprescription can be used. Maintenance Phase of Treatment of Chronic Psychotic Disorders or Bipolar Disorder - the dose of antipsychotic drugs needed to prevent relapse (maintenance therapy) can be reduced. Medications prescribed for certain side effects. Anticholinergics used to treat extrapyramidal symptoms may not be needed after a certain period due to the development of tolerance to the parkinsonian effects of antipsychotic drugs. Medications Prescribed for Off-Label Uses. Highly sedating antipsychotic medications such as quetiapine are often prescribed for management of insomnia in patients with psychiatric disorders. Similarly, antipsychotic medications are often prescribed for aggression and other behavioral problems not necessarily caused by psychosis or for the control of transient psychotic symptoms in post-traumatic stress disorder. These off-label uses put the patient at risk for serious side effects when other less risky medications or behavioral interventions such as cognitive behavioral therapy for insomnia may be equally or more effective [18][24].
Another example is Alzheimer's disease (AD) incidence. AD represents a significant challenge for the aging health of our over the world. Because of medical advances, the life expectancy of our residents is increasing. By the year 2030, it is estimated that more than 20% of the United States residents will be older than 65 yr [25]. Advancing age is related to an increased risk of dementia. AD is the most common cause of dementia, accounting for an estimated 60% to 80% of cases [26]. Review Renn examined published practice recommendations for discontinuation of cholinesterase inhibitors (ChEI) in AD. ChEI are widely used and typically employed as first-line pharmacotherapy for symptomatic treatment of major neurocognitive disorder caused by AD; however, treatment often continues through advanced disease stages [27]. A recent Cochrane Review found that ChEI treatment effects are small and of uncertain clinical importance [28]. The trials reviewed did not elucidate the relationship between duration of treatment and response. Because cognitive and behavioral impairments change during the progressive disease course, the effects of medications may be unpredictable, especially over long durations of treatment. Persons with advanced dementia may receive overly aggressive care that does not align with person-centered care goals, and polypharmacy from medications that are minimally beneficial may place patients at unnecessary risk [29][30][31]. However, ChEI treatment may contribute to meaningful improvements in noncognitive domains, such as reduction in neuropsychiatric symptoms and behavioral disturbance [32].
Twenty years ago antipsychotic polypharmacy (APP) was criticized as being more expensive, having unproven efficacy, and causing more side effects. However, in recent years, antipsychotic polypharmacy has become acceptable in the views of clinical practitioners and academic researchers. In an early 1970s survey of 4 states of the United States, the results revealed that New York psychiatrists most frequently prescribed a combination of 2 drugs, and some even prescribed 6 drugs at a time. Currently, no consensus regarding the definition of APP is available; however, most of the research papers have referred to it as the simultaneous use of 2 or more types of antipsychotic medication [33][34].
Interesting that Currently, APP has become more acceptable than in previous decades, and more evidence-based studies have proved its benefit. As there is no consensus on the ideal rate of APP and the combined use of other psychotropic drugs, the conception of a Health Care Quality Indicator Project can be utilized [35][36]. In this project, a set of indicators is developed by comparing data from different resources, and then the exact positions of these indicators can be learned by clinicians and health administrators to obtain consistent results. Thus, according to the 2 compatible results from Asia and Europe and previous reports of APP, they suggest the following approximated ideal rates of maintenance treatments in patients with schizophrenia: APP, 30%; combined mood stabilizer, 15%; combined antidepressant, 10%; combined anxiolytics, 30%; and combined hypnotic, 10%. A large discrepancy in the use of anticholinergics exists between Asia and Europe (45,1% vs 16%). This difference might be because Asian patients have been more susceptible to extrapyramidal side effects [37][38][39][40][41]. Thus, the doctor should constantly review the drugs that are prescribed to the patient, especially at the stage of maintenance therapy.
Other scientists-researchers from the Bruyere Research Institute and the Ontario Pharmacy Research Collaboration developed evidence-based guidelines for deprescribing. Each guideline is summarized in an easy-to-use algorithm and information brochure [42]. Algorithm of this guideline is shown in Figure 1. These recommendations apply to adult patients who have been prescribed antipsychotics for insomnia or behavioral and psychological symptoms in dementia (BPSD), provided the symptoms of the latter are controlled or the patient is unresponsive to a reasonable trial of therapy.
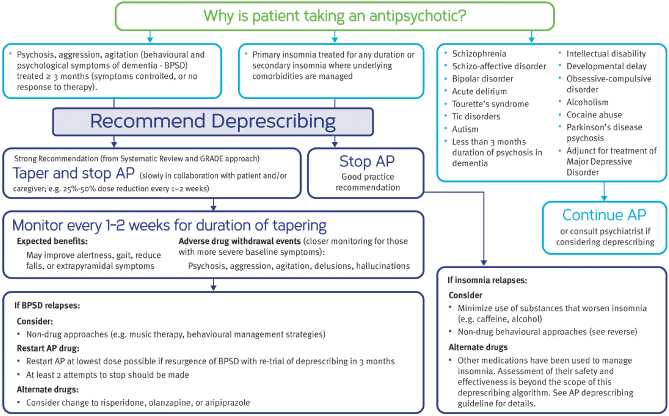
Figure 1. Antipsychotic (AP) Deprescribing Algorithm.
Combined with clinical judgment and an individualized approach to care, this guideline is intended to support clinicians and patients in successfully deprescribing antipsychotics, ultimately striving for better patient care. They also issued guidelines for the abolition of memantine and agonist benzodiazepine receptor [43][44].
A few studies have been conducted to study about doctors' opinion of this methodology. Many specialists were inclined to believe that deprescribing as «swimming against the tide» of patient expectations, the medical culture of prescribing, and organizational constraints; deprescribing came with inherent risks for both themselves and patients and conveyed a sense of vulnerability in practice. The only incentive to deprescribing they identified was the duty to do what was right for the patient. Some note that even despite existing drug withdrawal algorithms, specialists ignore them (Australia) or general practitioners refuse to do this, citing the fact that these are the duties of specialists. Very often, doctors simply do not have enough information on how to cancel the medication. Physicians fear that patients may perceive deprescribing as withdrawal of care before their end of life. These misconceptions prevent physicians from implementing deprescribing. For many GPs, «maintaining the status quo» for multimorbid patients with polypharmacy who are stable, is seen as the most reasonable course of action to undertake. In addition, clinicians recognize that clinical guidelines are rarely based on evidence from studies in older populations and rarely address modifying clinical targets with advancing age or care goals [12][45][46][47][48]. Physicians recommended organizational changes to support safer prescribing, including targeted funding for annual medicines reviews, computer prompts, improved information flows between prescribers, improved access to expert advice and user-friendly decision support, increased availability of nonpharmaceutical therapies, and enhanced patient engagement in medicines management.
There is another vulnerable group - adults with intellectual disabilities. There are many complexities in prescribing, dispensing, and administering psychotropic medication for such patients. Two large pharmaco-epidemiological studies in UK and England have indicated a marked disassociation between rates of psychotropic prescription in people with intellectual disabilities and recording of underlying mental illness for which they are indicated [49][50][51].
Ten principles of good deprescribing during medication review in the population with intellectual disabilities, based on the British Pharmacological Society's Principles for Good Prescribing 2010:
- Be clear about the reasons for de-prescribing psychotropic medication.
- Consider the patient's medication history before deprescribing.
- Consider other factors that might alter the benefits and risks of deprescribing psychotropic medication.
- Consider the patient's/carer's/families/advocates ideas, concerns and expectations. Share information about the benefits and harms of different options and allow patients/ carers to clarify what is important to them about these options.
- Ensure all medicines are effective, safe, cost-effective, in appropriate form and individualized for the patient with intellectual disability, behaviors that challenge and other conditions such as dysphagia, autism.
- Adhere to national guidelines and local formularies where appropriate. Use caution where the population with intellectual disabilities have not been considered in the guideline/formulary development process.
- Write unambiguous accurate documentation detailing reason for de-prescribing psychotropic medications (or other medications).
- Monitor and document the beneficial and adverse effects of de-prescribing psychotropic medicines and any effects on behavior.
- Communicate and document all de-prescribing decisions and the reasons for them and ensure information communicated to appropriate personnel such as GP, pharmacist, psychiatrist, epileptologist, carer and patient.
- Deprescribe psychotropic medications within the limitations of your knowledge, skills and experience of the population with intellectual disabilities and behavior disorders [52].
In conclusion, it should be noted disputes around this topic and researches are only gaining momentum. Even though some data on deprescribing are contradictory, there is security information for this recommendation. Possible negative effects are associated with the return of medical conditions or symptoms and adverse reactions to drug withdrawal, which emphasize necessary control and monitoring of the process by a medical professional. «Deprescribing clinics» are promising the development as a part of a large outpatient psychiatric service or even as a consultation service. Important areas for future researches include the suitability of deprescribing certain medications in specific populations, how to implement deprescribing processes into clinical care in a feasible and cost effective manner, and how to engage consumers throughout the process to achieve health and quality of life positive outcomes. Now, the «ideal» patient for deprescribing is getting used to living with side symptoms: the «working» scheme often is given to doctors and patients with difficulty, and neither one nor the other is interested in further experiments. Nevertheless, the results of a few studies so far on painless drug withdrawal and numerous ones on their longterm effects make one wonder whether this situation is correct. In the long term, evidence-based deprescribing, like any good practice, could be the final stage of assistance in the chain from the hospital to the outpatient or rehabilitation departments. The concept of deprescribing calls for a shift in focus, a revision of our goals: not to reduce or eliminate symptoms at all costs, but to strive primarily to improve the quality of patients' life.
Conflict of interest. The authors declare no conflict of interest.
Funding. The study had no sponsorship.
Финансирование. Исследование не имело спонсорской поддержки.
Конфликт интересов. Авторы заявляют об отсутствии конфликта интересов.
Список литературы
1. Ailabouni N.J., Nishtala P.S., Mangin D., Tordoff J.M. Challenges and Enablers of Deprescribing: A General Practitioner Perspective. // PLoS One. – 2016. – V.11(4). - e0151066. https://doi.org/10.1371/journal.pone.0151066
2. Reeve E., Shakib S., Hendrix I., Roberts M.S., Wiese M.D. The benefits and harms of deprescribing. // Med J Aust. – 2014. – V.201. – P.386–9. https://doi.org/10.5694/mja13.00200
3. Farrell B., Pottie K., Rojas-Fernandez C.H., Bjerre L.M., Thompson W., Welch V. Methodology for Developing Deprescribing Guidelines: Using Evidence and GRADE to Guide Recommendations for Deprescribing. // PLoS One. – 2016. – V.11(8). - e0161248. https://doi.org/10.1371/journal.pone.0161248
4. Scott I.A., Le Couteur D.G. Physicians need to take the lead in deprescribing. // Intern Med J. - 2015. – V.45(3). – P.352–6. https://doi.org/10.1111/imj.12693
5. Betteridge T.M., Frampton C.M., Jardine D.L. Polypharmacy— we make it worse! A cross-sectional study from an acute admissions unit. // Intern Med J. – 2012. – V.42(2). – P.208– 11. https://doi.org/10.1111/j.1445-5994.2011.02690.x
6. Farrell B., Tsang C., Raman-Wilms L., Irving H., Conklin J., Pottie K. What are priorities for deprescribing for elderly patients? Capturing the voice of practitioners: a modified delphi process. // PLoS One. – 2015. – V.10(4). - e0122246. https://doi.org/10.1371/journal.pone.0122246
7. Reeve E., Wiese M.D. Benefits of deprescribing on patients’ adherence to medications. // International journal of clinical pharmacy. – 2014. – V.36(1). – P.26–9. https://doi.org/10.1007/s11096-013-9871-z
8. Grudnikoff E., Bellonci C. Deprescribing in Child and Adolescent Psychiatry—A Sorely Needed Intervention. // American Journal of Therapeutics. - 2017. – V.24(1). e1-e2. https://doi.org/10.1097/MJT.0000000000000552.
9. Gupta S., Cahill J., Miller R. Deprescribing antipsychotics: A guide for clinicians. // BJPsych Advances. – 2018. – V.24(5). – P. 295-302. https://doi.org/10.1192/bja.2018.2
10. Woodward M.C. Deprescribing: Achieving Better Health Outcomes for Older People through Reducing Medications. // J. Pharm. Pract. Res. – 2003. – V.33. – P.323–328. https://doi.org/10.1002/jppr2003334323.
11. Sinnott C., Hugh S.M., Boyce M.B., Bradley C.P. What to give the patient who has everything? A qualitative study of prescribing for multimorbidity in primary care. // Br J Gen Pract. - 2015. – V.65(632). - e184–91. https://doi.org/10.3399/bjgp15X684001
12. Schuling J., Gebben H., Veehof L.J., Haaijer-Ruskamp F.M. Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. // BMC Fam Pract. – 2012. – V.13. – P.56. https://doi.org/10.1186/1471-2296-13-56
13. Schoen C., Osborn R., Squires D., Doty M., Pierson R., Applebaum S. New 2011 survey of patients with complex care needs in eleven countries finds that care is often poorly coordinated. // Health Aff (Millwood). – 2011. – V.30(12). – P.2437–48. https://doi.org/10.1377/hlthaff.2011.0923
14. Gupta S., Cahill J. A Prescription for “Deprescribing” in Psychiatry. // Psychiatric services (Washington, D.C.). - 2016. – V.67(8). – P.904-907. https://doi.org/10.1176/appi.ps.201500359.
15. Essock S.M., Covell N.H., Leckman-Westin E., Lieberman J.A., Sederer L.I., et al: Identifying clinically questionable psychotropic prescribing practices for Medicaid recipients in New York State. // Psychiatric Services. – 2009. – V.60(12). – P.1595–1602. https://doi.org/10.1176/ps.2009.60.12.1595
16. Ganguly R., Kotzan J.A., Miller L.S., Kennedy K., Martin B.C. Prevalence, trends, and factors associated with antipsychotic polypharmacy among Medicaid-eligible schizophrenia patients, 1998–2000. // Journal of Clinical Psychiatry. – 2004. – V.65(10). – P.1377–1388 https://doi.org/10.4088/jcp.v65n1013
17. Stahl S.M., Grady M.M. A critical review of atypical antipsychotic utilization: comparing monotherapy with polypharmacy and augmentation. // Current Medicinal Chemistry. – 2004. – V.11(3). – P.313–327. https://doi.org/10.2174/0929867043456070
18. Gupta S., Miller R. Deprescribing and Its Application to Psychiatry. In: Steingard S. (eds) Critical Psychiatry. Springer, Cham; 2019. https://doi.org/10.1007/978-3-030-02732-2_6
19. Reeve E, Shakib S, Hendrix I, Roberts MS, Wiese MD. Review of deprescribing processes and development of an evidence-based, patient-centred deprescribing process. // Br J Clin Pharmacol. – 2014. – V.78(4). – P.738–47. https://doi.org/10.1111/bcp.12386
20. Swofford CD, Kasckow JW, Scheller-Gilkey G, Inderbitzin LB. Substance use: a powerful predictor of relapse in schizophrenia. // Schizophr Res. – 1996. – V.20(1-2). – P.145- 151. https://doi.org/10.1016/0920-9964(95)00068-2
21. Deegan PE, Drake RE. Shared decision making and medication management in the recovery process. // Psychiatr Serv. – 2006. – V. 57(11). – P. 1636-9. https://doi.org/10.1176/ps.2006.57.11.1636
22. Stanhope V, Ingoglia C, Schmelter B, Marcus SC. Impact of person-centered planning and collaborative documentation on treatment adherence. // Psychiatr Serv. – 2013. – V. 64(1). – P. 76-9. https://doi.org/10.1176/appi.ps.201100489.
23. Jacobson L, Greeley D. What is recovery? A conceptual model and explication. // Psychiatric Services. – 2001. – V. 52(4). – P. 482–5. https://doi.org/10.1176/appi.ps.52.4.482
24. Taylor DJ, Pruiksma KE. Cognitive and behavioural therapy for insomnia (CBT-I) in psychiatric populations: a systematic review. // Int Rev Psychiatry. – 2014. – V.26(2). – P.205-13. https://doi.org/10.3109/09540261.2014.902808
25. Vincent G.K., Velkoff V. The next four decades: The older population in the United States: 2010-2050. // Current Population Reports. – 2010. – P.1-14.
26. Alzheimer’s Association. 2015 Alzheimer’s disease facts and figures. // Alzheimers Dement. – 2015. – V. 11(3). – P. 332-84. https://doi.org/10.1016/j.jalz.2015.02.003
27. Renn BN, Asghar-Ali AA, Thielke S, Catic A, Martini SR, et al. A Systematic Review of Practice Guidelines and Recommendations for Discontinuation of Cholinesterase Inhibitors in Dementia. // Am J Geriatr Psychiatry. – 2018. – V.26(2). – P.134-147. https://doi.org/10.1016/j.jagp.2017.09.027
28. Birks JS, Grimley Evans J. Rivastigmine for Alzheimer’s disease. // Cochrane Database Syst Rev. – 2015. – V.4. - CD001191. https://doi.org/10.1002/14651858.CD001191.pub4.
29. Mitchell SL, Morris JN, Park PS, Fries BE. Terminal care for persons with advanced dementia in the nursing home and home care settings. // J Palliat Med. – 2004. – V.7(6). – P.808- 16. https://doi.org/10.1089/jpm.2004.7.808
30. Parsons C, Hughes CM, Passmore AP, Lapane KL. Withholding, discontinuing and withdrawing medications in dementia patients at the end of life: a neglected problem in the disadvantaged dying? // Drugs Aging. – 2010. – V. 27(6). – P. 435-49. https://doi.org/10.2165/11536760-000000000-00000
31. Vetrano DL, Tosato M, Colloca G, Topinkova E, Fialova D, et al. Polypharmacy in nursing home residents with severe cognitive impairment: results from the SHELTER Study. // Alzheimers Dement. – 2013. – V.9(5). – P.587-93.. https://doi.org/10.1016/j.jalz.2012.09.009.
32. Birks J. Cholinesterase inhibitors for Alzheimer’s disease. // Cochrane Database Syst Rev. – 2006. – V.1. - CD005593. https://doi.org/10.1002/14651858.CD005593
33. Lin SK. Antipsychotic Polypharmacy: A Dirty Little Secret or a Fashion?. // Int J Neuropsychopharmacol. – 2020. – V.23(2). – P. 125–131. https://doi.org/10.1093/ijnp/pyz068
34. Brett J, Daniels B, Karanges EA, Buckley NA, Schneider C, et al. Psychotropic polypharmacy in Australia, 2006 to 2015: a descriptive cohort study. // Br J Clin Pharmacol. – 2017. – V.83(11). – P.2581-2588. https://doi.org/10.1111/bcp.13369
35. Arah OA, Westert GP, Hurst J, Klazinga NS. A conceptual framework for the OECD Health Care Quality Indicators Project. // Int J Qual Health Care. – 2006. – V.(1). – P. 5-13. https://doi.org/10.1093/intqhc/mzl024
36. Carinci F, Van Gool K, Mainz J, Veillard J, Pichora EC, et al. Towards actionable international comparisons of health system performance: expert revision of the OECD framework and quality indicators. // Int J Qual Health Care. – 2015. – V. 27(2). – P.137-46. https://doi.org/10.1093/intqhc/mzv004
37. Yang SY, Chen LY, Najoan E, Kallivayalil RA, Viboonma K, et al. Polypharmacy and psychotropic drug loading in patients with schizophrenia in Asian countries: Fourth survey of Research on Asian Prescription Patterns on antipsychotics. // Psychiatry Clin Neurosci. – 2018. – V.72(8). – P.572-579. https://doi.org/10.1111/pcn.12676
38. Toto S, Grohmann R, Bleich S, Frieling H, Maier HB, et al. Psychopharmacological Treatment of Schizophrenia Over Time in 30 908 Inpatients: Data From the AMSP Study. // Int J Neuropsychopharmacol. – 2019. – V.22(9). – P.560-573. https://doi.org/10.1093/ijnp/pyz037
39. Binder RL, Levy R. Extrapyramidal reactions in Asians. // Am J Psychiatry. - 1981. – V.138(9). – P.1243–1244. https://doi.org/10.1176/ajp.138.9.1243
40. Ormerod S, McDowell SE, Coleman JJ, Ferner RE. Ethnic differences in the risks of adverse reactions to drugs used in the treatment of psychoses and depression: a systematic review and meta-analysis. // Drug Saf. - 2008. V.31(7). – P.597–607. https://doi.org/10.2165/00002018-200831070-00005
41. Lin SK. Antipsychotic Polypharmacy: A Dirty Little Secret or a Fashion? // Int J Neuropsychopharmacol. – 2020. – V.23(2). – P.125–131. https://doi.org/10.1093/ijnp/pyz068
42. Bjerre LM, Farrell B, Hogel M, Graham L, Lemay G, et al. Deprescribing antipsychotics for behavioural and psychological symptoms of dementia and insomnia: Evidence-based clinical practice guideline. // Can Fam Physician. – 2018. – V.64(1). – P.17-27. PMID: 29358245.
43. Reeve E, Farrell B, Thompson W, Herrmann N, Sketris I, et al. Deprescribing cholinesterase inhibitors and memantine in dementia: guideline summary. // Med J Aust. – 2019. – V.210(4). – P.174-179. https://doi.org/10.5694/mja2.50015
44. Pottie K, Thompson W, Davies S, Grenier J, Sadowski CA, et al. Deprescribing benzodiazepine receptor agonists: Evidence-based clinical practice guideline. // Can Fam Physician. – 2018. – V.64(5). – P.339-351. PMID: 29760253
45. Wallis KA, Andrews A, Henderson M. Swimming Against the Tide: Primary Care Physicians’ Views on Deprescribing in Everyday Practice. // Ann Fam Med. – 2017. – V.15(4). – P.341–346. https://doi.org/10.1370/afm.2094
46. Kouladjian L, Gnjidic D, Reeve E, Chen TF, Hilmer SN. Health Care Practitioners’ Perspectives on Deprescribing Anticholinergic and Sedative Medications in Older Adults. // Ann Pharmacother. – 2016. – V.50(8). – P.625‐636. https://doi.org/10.1177/1060028016652997
47. Ailabouni NJ, Nishtala PS, Mangin D, Tordoff JM. Challenges and Enablers of Deprescribing: A General Practitioner Perspective. // PLoS One. – 2016. – V.11(4). - e0151066. https://doi.org/10.1371/journal.pone.0151066
48. Farrell B, Tsang C, Raman-Wilms L, Irving H, Conklin J, Pottie K. What are priorities for deprescribing for elderly patients? Capturing the voice of practitioners: a modified delphi process. // PLoS One. – 2015. – V.10(4). - e0122246. https://doi.org/10.1371/journal.pone.0122246
49. Sheehan R, Hassiotis A, Walters K, Osborn D, Strydom A, Horsfall L. Mental illness, challenging behaviour, and psychotropic drug prescribing in people with intellectual disability: UK population based cohort study. // BMJ. – 2015. – V.351. - h4326. https://doi.org/10.1136/bmj.h4326
50. Glover G.; Williams R.; et al. Prescribing of Psychotropic Drugs to People with Learning Disabilities and/or Autism by General Practitioners in England. - Public Health England: London, UK, 2015.
51. Flood B. De-Prescribing of Psychotropic Medications in the Adult Population with Intellectual Disabilities: A Commentary. // Pharmacy (Basel). – 2018. – V.6(2). – P.28. https://doi.org/10.3390/pharmacy6020028.
52. British Pharmacological Society. Ten Principles of Good Prescribing. British Pharmacological Society: London, UK, 2012.
Об авторах
Ж. Б. БибековаКазахстан
Жазира Бектурсыновна Бибекова — ассистент кафедры неврологии, нейрохирургии, психиатрии и реабилитологии
Караганда
К. В. Заровный
Казахстан
Кирилл Владимирович Заровный — врач-резидент кафедры неврологии, нейрохирургии, психиатрии и реабилитологии
Караганда
В. О. Цыганова
Казахстан
Виктория Олеговна Цыганова — врач-резидент кафедры психиатрии, наркологии и неврологии
Алмата
Рецензия
Для цитирования:
Бибекова Ж.Б., Заровный К.В., Цыганова В.О. Отмена препаратов в психиатрии: проблемы и возможности. Медицинский вестник Юга России. 2020;11(3):6-14. https://doi.org/10.21886/2219-8075-2020-11-3-6-14
For citation:
Bibekova Zh.B., Zarovnyy K.V., Tsyganova V.O. Deprescribing in psychiatry: challenges and opportunities. Medical Herald of the South of Russia. 2020;11(3):6-14. https://doi.org/10.21886/2219-8075-2020-11-3-6-14







































